Left ventricular aneurysm pathophysiology: Difference between revisions
No edit summary |
|||
| Line 3: | Line 3: | ||
{{CMG}};{{AE}}{{MehdiP}} | {{CMG}};{{AE}}{{MehdiP}} | ||
==Overview== | ==Overview== | ||
Aneurysm forms when [[intraventricular]] tension stretches the noncontracting [[Infarction|infarcted]] [[Myocardium|heart muscle]] | [[Aneurysm]] forms when [[intraventricular]] tension stretches the noncontracting [[Infarction|infarcted]] [[Myocardium|heart muscle]], producing expansion of the thin layer of [[necrotic]] muscle and [[fibrous]] tissue that bulges with each cardiac contraction. | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Gross Pathology=== | ===Gross Pathology=== | ||
*The wall of a mature aneurysm is a white [[fibrous]] [[scar]]. Characteristically, the aneurysmal portion of the [[Left ventricle|LV]] wall is thin and a mural [[thrombosis]] may be attached to the [[endocardial]] surfcace and may be [[Calcified lesion|calcified]].<ref name="pmid5842520">{{cite journal |vauthors=Dubnow MH, Burchell HB, Titus JL |title=Postinfarction ventricular aneurysm. A clinicomorphologic and electrocardiographic study of 80 cases |journal=Am. Heart J. |volume=70 |issue=6 |pages=753–60 |year=1965 |pmid=5842520 |doi= |url=}}</ref> The [[endocardium]] beneath retains its trabeculations, and the area of scarring is not clearly demarcated from the rest of the wall. | *The wall of a mature [[aneurysm]] is a white [[fibrous]] [[scar]]. Characteristically, the aneurysmal portion of the [[Left ventricle|LV]] wall is thin and a mural [[thrombosis]] may be attached to the [[endocardial]] surfcace and may be [[Calcified lesion|calcified]].<ref name="pmid5842520">{{cite journal |vauthors=Dubnow MH, Burchell HB, Titus JL |title=Postinfarction ventricular aneurysm. A clinicomorphologic and electrocardiographic study of 80 cases |journal=Am. Heart J. |volume=70 |issue=6 |pages=753–60 |year=1965 |pmid=5842520 |doi= |url=}}</ref> The [[endocardium]] beneath retains its trabeculations, and the area of scarring is not clearly demarcated from the rest of the wall. | ||
*The wall of the aneurysm becomes more densely [[Fibrous|fibrotic]] as the time passages, but it bulges outward with each [[Systole|cardiac contraction]] and causes some of the [[Left ventricle|left ventricular]] [[stroke volume]] to be ineffective. | *The wall of the aneurysm becomes more densely [[Fibrous|fibrotic]] as the time passages, but it bulges outward with each [[Systole|cardiac contraction]] and causes some of the [[Left ventricle|left ventricular]] [[stroke volume]] to be ineffective. | ||
Revision as of 15:50, 4 November 2016
|
Left ventricular aneurysm Microchapters |
|
Differentiating Left ventricular aneurysm from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Left ventricular aneurysm pathophysiology On the Web |
|
American Roentgen Ray Society Images of Left ventricular aneurysm pathophysiology |
|
Risk calculators and risk factors for Left ventricular aneurysm pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2]
Overview
Aneurysm forms when intraventricular tension stretches the noncontracting infarcted heart muscle, producing expansion of the thin layer of necrotic muscle and fibrous tissue that bulges with each cardiac contraction.
Pathophysiology
Gross Pathology
- The wall of a mature aneurysm is a white fibrous scar. Characteristically, the aneurysmal portion of the LV wall is thin and a mural thrombosis may be attached to the endocardial surfcace and may be calcified.[1] The endocardium beneath retains its trabeculations, and the area of scarring is not clearly demarcated from the rest of the wall.
- The wall of the aneurysm becomes more densely fibrotic as the time passages, but it bulges outward with each cardiac contraction and causes some of the left ventricular stroke volume to be ineffective.
Microscopic findings
- On microscopic histopathological analysis hyalinized fibrous tissue is the predominant finding. However, a small number of viable muscle cells are usually present.[2]
- It takes 1 month for fibrous tissue to forms however, collagen tissue is formed during the first 10 days. So, when an aneurysm is said to be present within 1 week of a first myocardial infarction, the wall is composed largely of necrotic muscle and is not therefore by definition a true aneurysm.[3]
Images
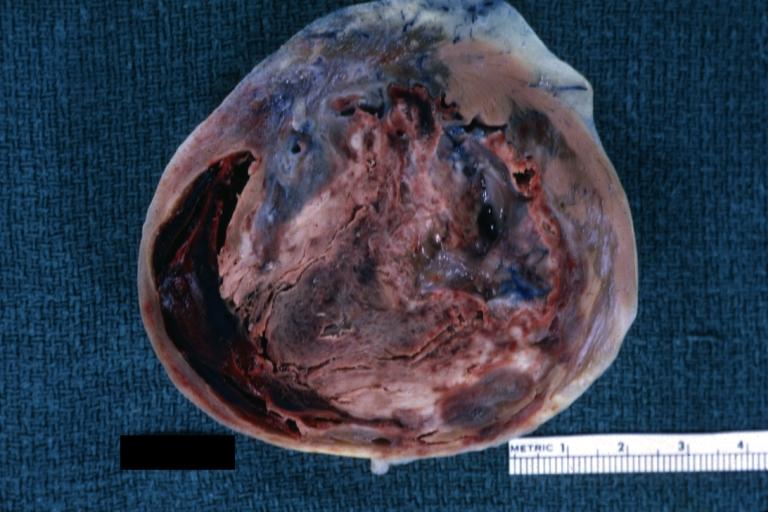
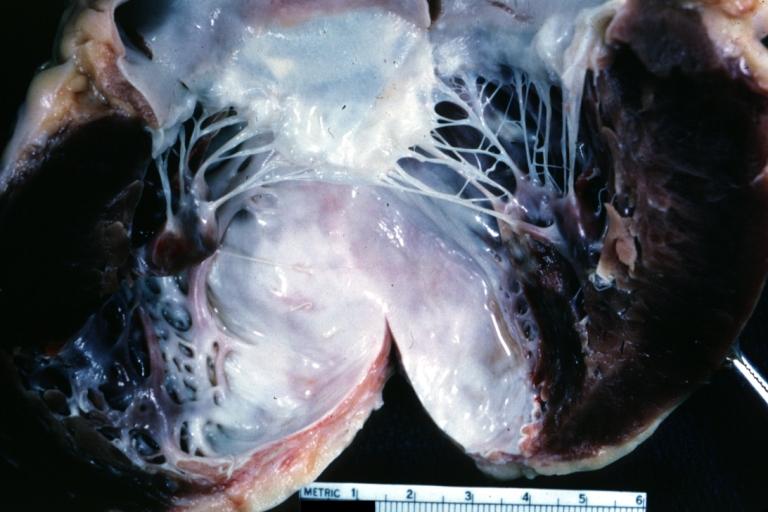
The gross pathologic features of LV aneurysm are shown below.[4]
-
Left ventricular aneurysm
-
Left Ventricle Aneurysm: Gross natural color horizontal section apex of left ventricle with aneurysmal dilation and mural thrombus. A large scar tissue in myocardium.
-
Left ventricular aneurysm.
-
Heart; old myocardial infarction with aneurysm formation
References
- ↑ Dubnow MH, Burchell HB, Titus JL (1965). "Postinfarction ventricular aneurysm. A clinicomorphologic and electrocardiographic study of 80 cases". Am. Heart J. 70 (6): 753–60. PMID 5842520.
- ↑ Gorlin R, Klein MD, Sullivan JM (1967). "Prospective correlative study of ventricular aneurysm. Mechanistic concept and clinical recognition". Am. J. Med. 42 (4): 512–31. PMID 6024720.
- ↑ PHARES WS, EDWARDS JE, BURCHELL HB (1953). "Cardiac aneurysms; clinicopathologic studies". Proc Staff Meet Mayo Clin. 28 (9): 264–71. PMID 13056012.
- ↑ Images courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology