Left ventricular aneurysm pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Left ventricular aneurysm}} | {{Left ventricular aneurysm}} | ||
{{CMG}} | {{CMG}};{{AE}}{{MehdiP}} | ||
==Overview== | |||
Aneurysm forms when intraventricular tension stretches the noncontracting infarcted heart muscle and thus produces expansion of the thin layer of necrotic muscle, and fibrous tissue that bulges with each cardiac contraction. | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Gross Pathology=== | ===Gross Pathology=== | ||
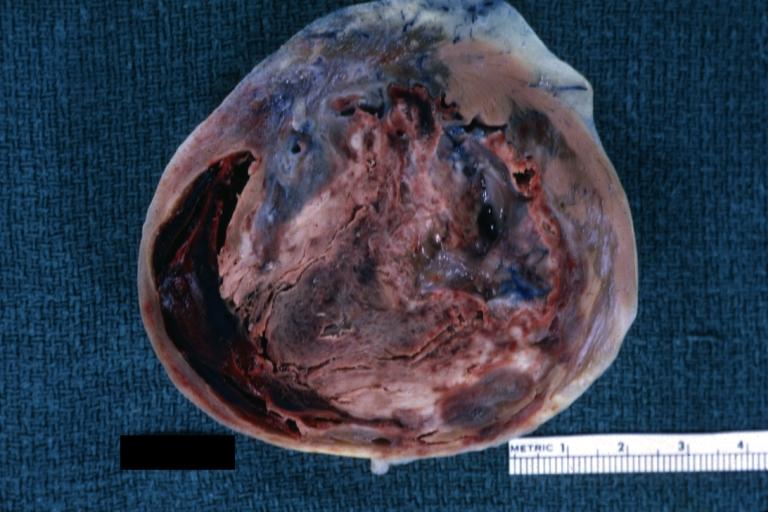
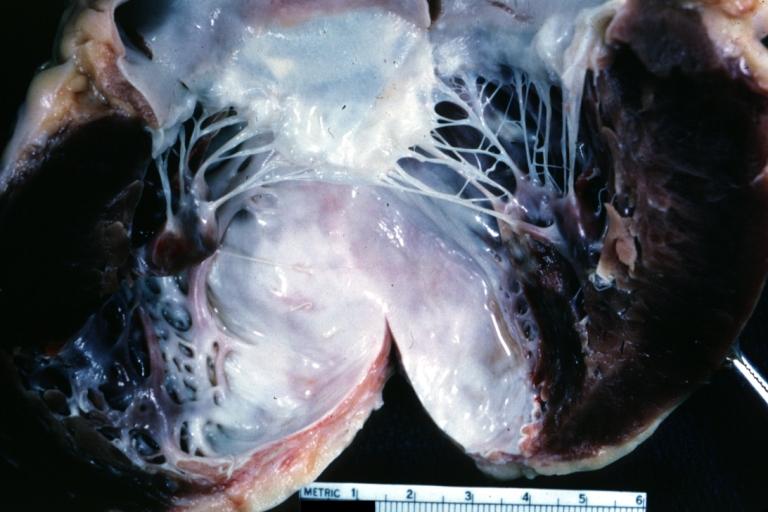
The wall of a mature aneurysm is a white fibrous scar. Characteristically, the aneurysmal portion of the LV wall is thin and a mural thrombosis may be attached to the endocardial surfcace and may be calcified. The endocardium beneath retains its trabeculations, and the area of scarring is not clearly demarcated from the rest of the wall. Finally, the wall of the aneurysm becomes more densely fibrotic, but it continues to bulge with each cardiac contraction and causes some of the left ventricular stroke volume to be ineffective. | |||
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. [http://www.peir.net © PEIR, University of Alabama at Birmingham, Department of Pathology] | Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. [http://www.peir.net © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
Revision as of 17:47, 2 November 2016
|
Left ventricular aneurysm Microchapters |
|
Differentiating Left ventricular aneurysm from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Left ventricular aneurysm pathophysiology On the Web |
|
American Roentgen Ray Society Images of Left ventricular aneurysm pathophysiology |
|
Risk calculators and risk factors for Left ventricular aneurysm pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2]
Overview
Aneurysm forms when intraventricular tension stretches the noncontracting infarcted heart muscle and thus produces expansion of the thin layer of necrotic muscle, and fibrous tissue that bulges with each cardiac contraction.
Pathophysiology
Gross Pathology
The wall of a mature aneurysm is a white fibrous scar. Characteristically, the aneurysmal portion of the LV wall is thin and a mural thrombosis may be attached to the endocardial surfcace and may be calcified. The endocardium beneath retains its trabeculations, and the area of scarring is not clearly demarcated from the rest of the wall. Finally, the wall of the aneurysm becomes more densely fibrotic, but it continues to bulge with each cardiac contraction and causes some of the left ventricular stroke volume to be ineffective.
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Left ventricular aneurysm
-
Left Ventricle Aneurysm: Gross natural color horizontal section apex of left ventricle with aneurysmal dilation and mural thrombus. A large scar tissue in myocardium.
-
Left ventricular aneurysm.
-
Heart; old myocardial infarction with aneurysm formation