Template:WikiDoc Cardiology News
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic:
There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Synonyms and related keywords: LBBB
Left bundle branch block (LBBB) is a cardiac conduction abnormality seen on the electrocardiogram (ECG). In this condition, activation of the left ventricle is delayed, which results in the left ventricle contracting later than the right ventricle.
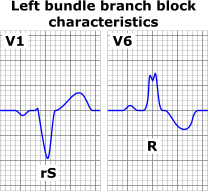
EKG diagnosis
The criteria to diagnose a left bundle branch block on the electrocardiogram:
- The heart rhythm must be supraventricular in origin
- The QRS duration must be = or > 120 ms
- There should be a QS or rS complex in lead V1
- There should be a monophasic R wave in leads I and V6.
The T wave should be deflected opposite the terminal deflection of the QRS complex. This is known as appropriate T wave discordance with bundle branch block. A concordant T wave may suggest ischemia or myocardial infarction.
Causes of LBBB
Among the causes of LBBB are:
Reading Ischemia In The Presence Of LBBB
LBBB can simulate an MI due to the associated secondary ST changes and pseudoinfarct q waves that it causes, and furthermore it can mask the EKG changes of an MI.
Sgarbossa Criteria
An EKG scoring system was developed and the independent criterion were assessed on patients from the GUSTO-1 trial patients were scored from 0-5 for presence of LBBB in the context of acute myocardial infarction.
| Criteria Score |
| #ST-segment elevation ≥ 1 mm and concordant with QRS complex 5 |
| #ST-segment depression ≥ 1 mm in lead V1,V2 or V3 3 |
| #ST-segment elevation ≥ 5 mm and discordant with QRS complex 2 |
|
Pseudoinfarct Patterns: Simulation of an Anterior MI
- Can cause poor R wave progression. Often see a decrease in the amplitude of R waves to the midprecordium in the absence of a septal infarct.
- QS complexes are often seen in the right precordial leads in uncomplicated LBBB and they may even extend as far out as V5 or V6.
- Non infarctional Q waves may be seen in aVL.
- The Reason: LBBB causes a loss of the normal septal r waves in the right precordial leads. The septum is no longer being depolarized from left to right as it normally does because of the delay down the left bundle.
- There can occasionally be Rs complexes in V1. These unanticipated initial positive forces are due to early RV depolarization and may actually mask the q waves (i.e. loss of initial septal forces) that accompany an anteroseptal MI.
Simulation of an Inferior MI
- Noninfarctional QS complexes can be seen in leads II, III, and aVF in LBBB.
- There are a number of autopsy cases were there are QS waves inferiorly without evidence of an MI.
- There are several reported cases of intermittent LBBB in which the QS waves inferiorly were present only in the aberrantly conducted beats.
- Conversely, LBBB may mask the development of Q waves in an MI.
- Primary ST segment and T wave changes are repolarization changes that are seen with ischemia or electrolyte imbalance and reflect actual changes in the myocardial action potentials.
- Secondary ST segment and T wave wave changes occur when the sequence of ventricular activation is altered without any disturbance in the electrical properties of the myocardial cells such as is seen in LBBB.
- As a result of secondary ST segment and T wave wave changes, the QRS and the T wave vectors are oriented in opposite directions which is known as discordance of the QRS and T wave vectors.
- Thus, the QRS is often predominantly negative in the right precordial leads while the T wave is oriented positively. In those leads where there is a tall positive R wave there is a negative T wave.
- These secondary ST segment and T wave changes often mimic infarction, and furthermore they may mask the ST segment and T wave changes of an MI.
- Sometimes primary ST segment and T wave changes will be superimposed on the LBBB pattern and the following suggests the diagnosis of ischemia or infarction:
- ST segment elevation in leads with a predominant R wave. In uncomplicated LBBB, the ST segment is isoelectric or depressed.
- T wave inversions in the right to midprecordial leads or in other leads with a predominantly negative QRS. In other words there is an absence of discordance, and there is the presence of concordance.
- Morphology: In leads with a predominant R wave, the ST segment begins to slope downwards and blends into the T wave. The ascending limb of the T wave ascends back to the baseline at a more acute angle.
- The ischemic T waves have a more symmetric appearance and a slightly upwardly bowed ST segment.
- ST segment and T wave elevations simulating acute infarction: The ST segment can be markedly elevated (up to 10 mm or more at the J point ) in leads with a QS or rS segment in uncomplicated LBBB. In addition, there can be a loss of R wave progression.
- T wave inversions in intermittent LBBB: May develop deep T wave inversions in the right to midprecordial leads of normally conducted beats in the absence of CAD. These T wave inversions are deepest in leads V1 to V4 with a symmetric or coved appearance.
Etiology of Q Waves
- As described earlier, in LBBB there is a loss of depolarization from left to right, which produced an initial r wave in the right precordial leads.
- Now there is depolarization from right to left. Consequently the initial r wave is lost, and the non infarctional QS complexes may appear in the precordial leads.
- The reversal of septal activation results in RS complexes in the left precordial leads.
Can You Read a Left Ventricular Free Wall Infarction In the Presence of a LBBB?
- No. This pattern of infarction results in abnormal q waves in the midprecordial to lateral precordial leads.
- In LBBB the initial septal depolarization forces are directed from right to left. These leftward septal forces will produce an initial R wave in the midprecordial to the lateral precordial leads, masking the loss of potential q waves produced by the infarction.
- Therefore left ventricular free wall infarction by itself will not produce diagnostic q waves in the presence of a LBBB.
- Poor R wave progression is seen in uncomplicated LBBB.
Can You Read a Septal Infarction in the Presence of LBBB?
- Yes. Again the septal forces are directed to the left in LBBB.
- If enough of the septum is infarcted to eliminate these initial leftward septal forces, abnormal QR, QRS, or qrs types of complexes may appear in the midprecordial to lateral precordial leads.
- These initial q waves may reflect posterior and superior forces from the spared basal portion of the septum.
- Small q waves of 0.03 sec or less may be seen in leads I, V5 to V6 in uncomplicated LBBB.
- The presence of q waves laterally is an example of false localization. [1]
Treatment
- Medical Care: Patients with LBBB require complete cardiac evaluation, and those with LBBB and near-syncope or syncope may require a pacemaker.
- Surgical Care: Some patients with LBBB, a markedly prolonged QRS, and congestive heart failure may benefit from a pacemaker, which provides rapid left ventricular contractions.
Classification
Some sources distinguish between a "left anterior fascicular block" (LAFB)[2] and a "left posterior fascicular block" (LAPB).[3] This refers to the bifurcation of the left bundle branch.
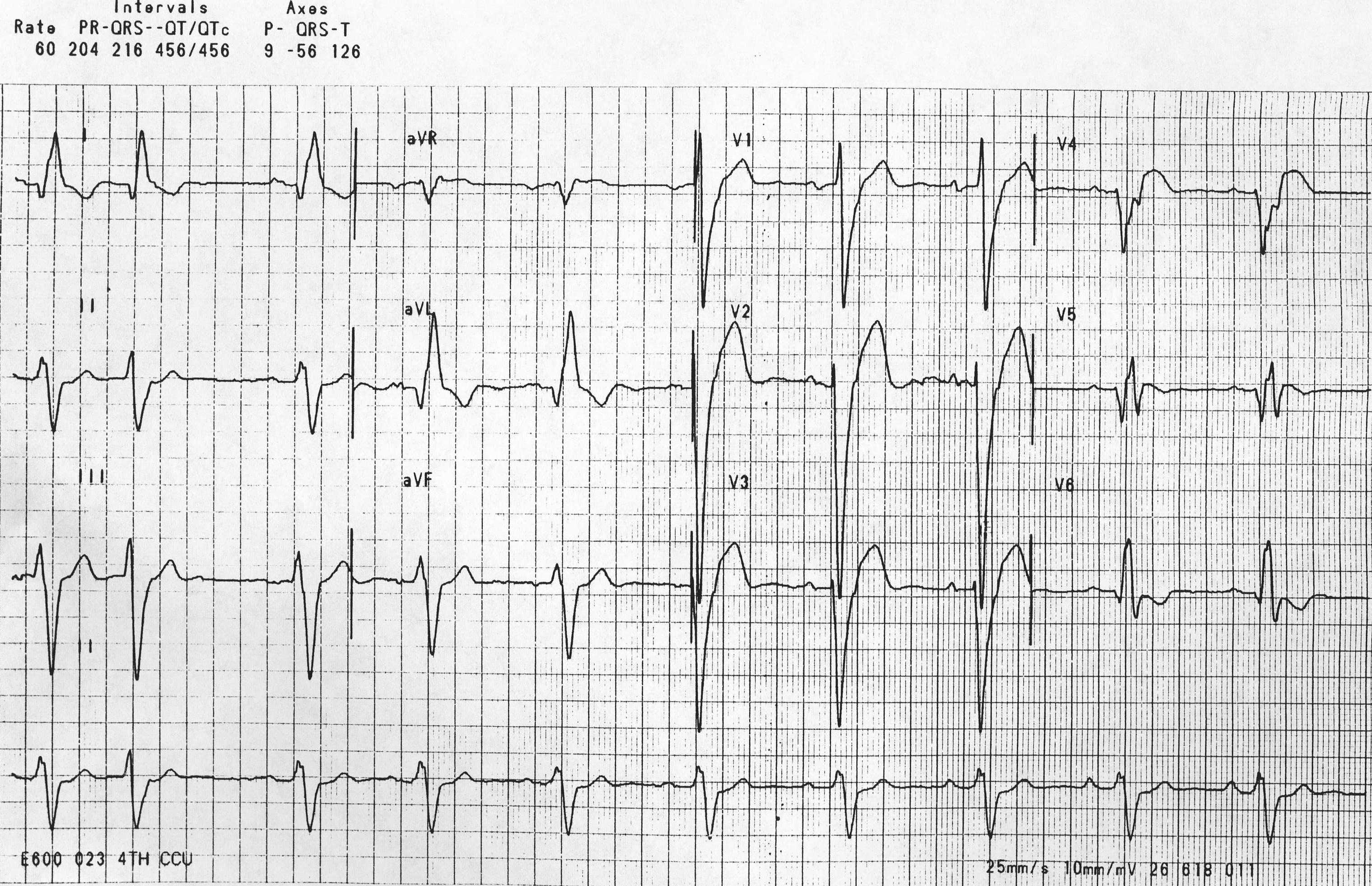
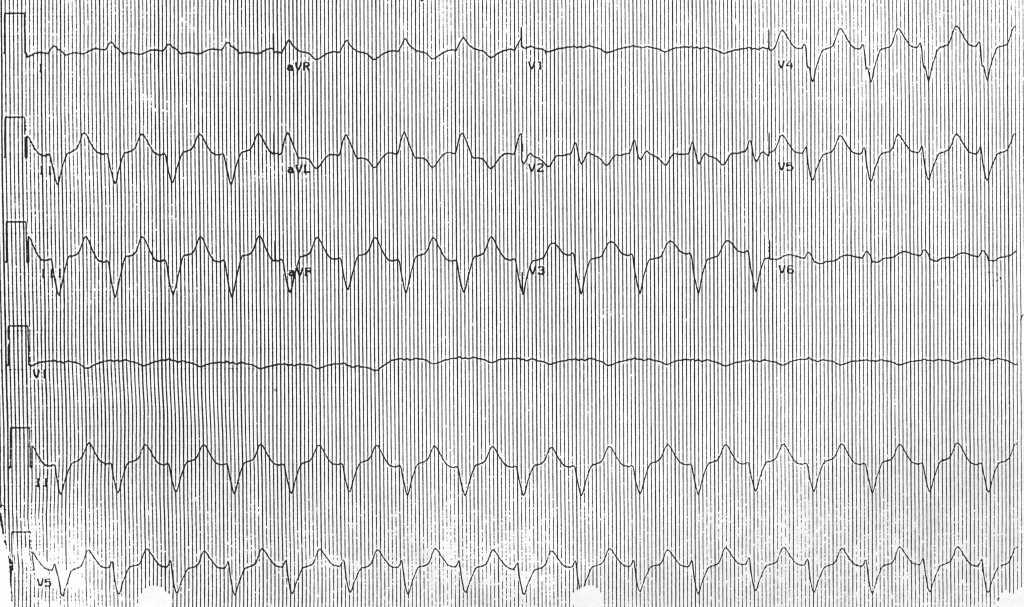
EKG Examples
-
Left Bundle Branch Block + Left Anterior Fascicular Block + Left atrial enlargement
-
Left Bundle Branch Block + Supraventricular tachycardia Image courtesy of Dr Jose Ganseman
See also
References
External links
Additional resources
Template:SIB
de:Linksschenkelblock
Template:WikiDoc Sources
|