Krukenberg tumor
| Krukenberg tumor | |
 | |
|---|---|
| Krukenberg tumor |
|
WikiDoc Resources for Krukenberg tumor |
|
Articles |
|---|
|
Most recent articles on Krukenberg tumor Most cited articles on Krukenberg tumor |
|
Media |
|
Powerpoint slides on Krukenberg tumor |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Krukenberg tumor at Clinical Trials.gov Trial results on Krukenberg tumor Clinical Trials on Krukenberg tumor at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Krukenberg tumor NICE Guidance on Krukenberg tumor
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Krukenberg tumor Discussion groups on Krukenberg tumor Patient Handouts on Krukenberg tumor Directions to Hospitals Treating Krukenberg tumor Risk calculators and risk factors for Krukenberg tumor
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Krukenberg tumor |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Soujanya Thummathati, MBBS [2]
Synonyms and keywords: carcinoma mucocellulare; Ovarian tumor
Overview
Krukenberg tumor is a rare metastatic signet ring cell adenocarcinoma of the ovary.[1] Krukenberg tumor was first described as a new type of primary ovarian malignancy by Friedrich Ernst Krukenberg (1871–1946), a German gynecologist and pathologist, in 1896 which was later confirmed to be of metastatic gastrointestinal tract origin.[1] The pathogenesis of Krukenberg tumors involves metastasis of tumor cells from the stomach, appendix or colon to the ovaries.[2] Metastasis is more likely via the lymphatic spread. However, direct seeding across the abdominal cavity may also occur. On gross pathology, asymmetrically enlarged ovaries with a bosselated contour, usually solid, yellow or white cross sectioned surfaces, and the absence of adhesions or peritoneal deposits are characteristic findings of Krukenberg tumors.[1] Krukenberg tumor must be differentiated from primary mucinous carcinoma, mucinous carcinoid tumor, signet ring stromal tumor, sclerosing stromal cell tumor, clear cell adenocarcinoma of the ovary, and sertoli-leydig cell tumor.[1] The incidence of Krukenberg tumors is estimated to be approximately 0.16 per 100,000 individuals.[3][4] Krukenberg tumor is more commonly observed among women in their fifth decade of lives, with an average around 45 years of age. The majority of patients with Krukenberg tumor remain asymptomatic or have non-specific gastrointestinal symptoms.[1] Early clinical features include abdominal pain and distension(from the large, bilateral ovarian masses). If left untreated, patients with Krukenberg tumors may progress to develop virilization from the excessive hormone production from the ovarian stroma.[5] Prognosis is generally poor, and the 5 year survival rate of patients with Krukenberg tumor is lower in patients in with a preoperative serum CA-125 levels greater than 75 U/mL when compared with patients with CA-125 levels less than 75 U/mL.[6] The median survival of patients is between 7 to 14 months.[5] X rays, ultrasound, CT, MRI and immunohistochemistry help in the diagnosis of Krukenberg tumors. Management of Krukenberg tumors is driven by the identification and treatment of the primary cancer. Bilateral oophorectomy may only be performed for patients where the metastasis is localized to the ovaries.[7] The significance of early detection of ovarian metastasis and the importance of monitoring serum CA-125 level may improve the prognosis. Surgical resection may not be an option if the tumor has already metastasized to other sites.
Historical Perspective
Krukenberg tumor was first described as a new type of primary ovarian malignancy by Friedrich Ernst Krukenberg (1871–1946), a German gynecologist and pathologist, in 1896 which was later confirmed to be of metastatic gastrointestinal tract origin.[1]
Pathophysiology
- The majority of Krukenberg tumors are bilateral.[1]
- Stomach and colon are the primary sites in the majority of Krukenberg tumor cases (70%).[1]
- The pathogenesis of Krukenberg tumors involves metastasis of tumor cells from the stomach, appendix, or colon to the ovaries.[2]
- Metastasis is more likely via the lymphatic spread. However, direct seeding across the abdominal cavity may also occur.
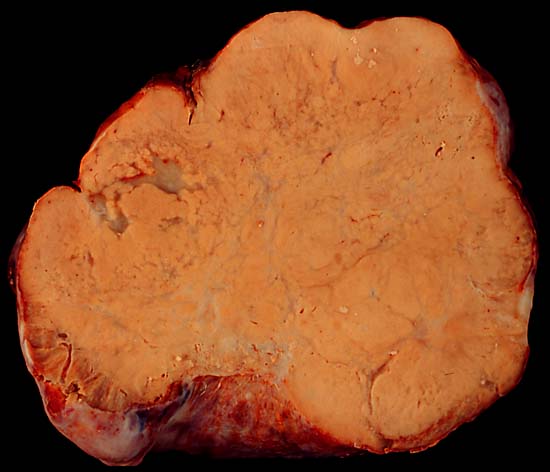
- On gross pathology, asymmetrically enlarged ovaries with a bosselated contour, usually solid, yellow or white cross sectioned surfaces, and the absence of adhesions or peritoneal deposits are characteristic findings of Krukenberg tumors.[1]
- On microscopic histopathological analysis, Krukenberg tumors are characterized by the following features:
- Tumor composed of two components:
- Epithelial
- Mucin-secreting signet ring cells with eccentric hyperchromatic nuclei
- Cytoplasm may be eosinophilic and granular, pale and vacuolated, or a bull's eye (targetoid) appearance with a large vacuole with a central to paracentral eosinophilic body composed of a droplet of mucin
- Signet ring cells may be single, clustered, nested, or arranged in tubules, acini, trabeculae, or cords
- Stromal
- Epithelial
- Tumor composed of two components:
- Stomach is the primary site in the majority of Krukenberg tumor cases (70%).[1]
-
Bilateral ovarian neoplasm retaining the shape of ovary. Cut section of the tumor shows solid with mucinous areas[8]
Causes
- Krukenberg tumor may be caused by metastasis of the tumor cells from a primary cancer in the stomach, appendix, or the colon via:[2]
- Lymphatic spread or
- Direct seeding across the abdominal cavity
Differentiating Krukenberg tumor from other Diseases
- Krukenberg tumor must be differentiated from:[1]
- Primary mucinous carcinoma
- Mucinous carcinoid tumor
- Signet ring stromal tumor
- Sclerosing stromal cell tumor
- Clear cell adenocarcinoma of the ovary
- Sertoli-Leydig cell tumor
Epidemiology and Demographics
Incidence
- The incidence of Krukenberg tumor is estimated to be approximately 0.16 per 100,000 individuals.[3][4]
Age
- Patients of all age groups may develop Krukenberg tumor.
- Krukenberg tumor is more commonly observed among women in the fifth decade, with an average age of presentation at 45 years of age.
Risk Factors
- There are no known direct causes for Krukenberg tumors. Common risk factors for ovarian cancer may include:[9]
- Nulliparity
- Early menarche
- Late menopause
- Hormone therapy
- Fertility medications
Natural History, Complications and Prognosis
- The majority of patients with Krukenberg tumor remain asymptomatic or have non-specific gastrointestinal symptoms.[1]
- Early clinical features include abdominal pain and distension (from the large, bilateral ovarian masses).[1]
- If left untreated, patients with Krukenberg tumor may progress to develop virilization from the excessive hormone production from the ovarian stroma.[5]
- Common complications of Krukenberg tumors include ascites, virilization, and pseudo-Meig syndrome.[5][1]
- Pseudo-Meig syndrome is defined as a hydrothorax with ascites, but with the absence of tumor cells.
- Prognosis is generally poor, and the 5 year survival rate of patients with Krukenberg tumor is lower in patients in with a preoperative serum CA-125 levels greater than 75 U/mL when compared with patients with CA-125 levels less than 75 U/mL.[6] The median survival of patients is between 7 to 14 months.[5]
Diagnosis
Symptoms
- Krukenberg tumor is usually asymptomatic.[1]
- Symptoms of Krukenberg tumor may include the following:[1][2]
- Non-specific gastrointestinal symptoms
- Abdominal or pelvic pain
- Abdominal distension
- Bloating
- Dyspareunia
- Vaginal bleeding
- Menstrual irregularities
- Hirsutism
Physical Examination
- Patients with Krukenberg tumor usually appear well in the early stages.
- Physical examination may be remarkable for:[1][2]
Laboratory Findings
- There are no specific laboratory findings associated with Krukenberg tumors.
Imaging Findings
X Ray
- On x ray, Krukenberg tumor may present with the following findings:[4]
- Prominent small bowel loops filled with gas
- No air-fluid level
- No radiographic signs of intestinal obstruction
-
X ray showing prominent small bowel loops filled with gas, no air-fluid level, no radiographic signs of intestinal obstruction[10]
Ultrasound
- On pelvic ultrasound, Krukenberg tumor is characterized by the following:[3][4]
- Bilateral, solid ovarian masses with clear, well defined margins
- An irregular hyper-echoic solid pattern and moth eaten like cyst formation is also considered a characteristic feature
-
Large, solid, well defined bilateral ovarian masses[10]
-
Large, solid, well defined bilateral ovarian masses[10]
-
Large, solid, well defined bilateral ovarian masses[10]
-
Large, solid, well defined bilateral ovarian masses[10]
CT
- On CT, Krukenberg tumor is characterized by the following:[4][11]
- Large, lobulated, and multicystic masses with soft-tissue components which are indistinguishable from primary ovarian cancers
- Presence of a concurrent gastric or colic mural lesion
-
Krukenberg tumour of the right ovary from colon cancer[10]
MRI
- On pelvic MRI, Krukenberg tumor is characterized by the following:[4][12][13][14]
- Bilateral complex masses with hypo-intense solid components (dense stromal reaction)
- Internal hyperintensity (mucin) on T1 and T2 weighted MR images
- Strong contrast enhancement is usually seen in the solid component or the wall of the intratumoral cyst
-
Coronal T2 image[10]
-
Axial T1 image[10]
-
Sagittal T2 image[10]
-
Axial T2 image[10]
-
Axial T1 C+ fat sat dynamic contrast study image[10]
Other Diagnostic Studies
Immunohistochemistry
- Krukenberg tumor may also be diagnosed using immunohistochemistry.[1]
- Findings on immunohistochemistry include:
Serum CA-125
- Serum concentrations of CA-125 may be helpful for:[1]
- Post-operative follow-up of patients for evaluation of complete resection of the tumor
- Follow-up of patients with a history of primary adenocarcinomas (particularly gastrointestinal) for early detection of ovarian metastasis
Treatment
Medical Therapy
- Management of Krukenberg tumor is driven by the identification and treatment of the primary cancer.
- Chemotherapy/radiation has no significant effect on the prognosis of patients with Krukenberg tumors.[1]
Surgery
- Bilateral oophorectomy may only be performed for patients where the metastasis is localized to the ovaries.[7]
- The significance of early detection of ovarian metastasis and the importance of monitoring serum CA-125 level may improve the prognosis.
- Surgical resection may not be an option if the tumor has already metastasized to other sites.
Prevention
- There are no preventive measures available for Krukenberg tumors.
Case Studies
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 Al-Agha OM, Nicastri AD (2006). "An in-depth look at Krukenberg tumor: an overview". Arch Pathol Lab Med. 130 (11): 1725–30. doi:10.1043/1543-2165(2006)130[1725:AILAKT]2.0.CO;2. PMID 17076540.
- ↑ 2.0 2.1 2.2 2.3 2.4 Krukenberg tumor. Wikipedia. https://en.wikipedia.org/wiki/Krukenberg_tumor#cite_note-Young2006-4 Accessed on March 21, 2016.
- ↑ 3.0 3.1 3.2 Tellier F, Steibel J, Chabrier R, Blé FX, Tubaldo H, Rasata R; et al. (2012). "Sentinel lymph nodes fluorescence detection and imaging using Patent Blue V bound to human serum albumin". Biomed Opt Express. 3 (9): 2306–16. doi:10.1364/BOE.3.002306. PMC 3447570. PMID 23024922.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Krukenberg tumour. Radiopedia. Accessed on March 23, 2016.
- ↑ 5.0 5.1 5.2 5.3 5.4 Hornung M, Vogel P, Schubert T, Schlitt HJ, Bolder U (2008). "A case of virilization induced by a Krukenberg tumor from gastric cancer". World J Surg Oncol. 6: 19. doi:10.1186/1477-7819-6-19. PMC 2275731. PMID 18279511.
- ↑ 6.0 6.1 Khan M, Bhatti RP, Mukherjee S, Ali AM, Gilman AD, Mirrakhimov AE; et al. (2015). "A 26-year-old female with metastatic primary gastrointestinal malignancy presenting as menorrhagia". J Gastrointest Oncol. 6 (2): E21–5. doi:10.3978/j.issn.2078-6891.2014.080. PMC 4311099. PMID 25830046.
- ↑ 7.0 7.1 Kim WY, Kim TJ, Kim SE, Lee JW, Lee JH, Kim BG; et al. (2010). "The role of cytoreductive surgery for non-genital tract metastatic tumors to the ovaries". Eur J Obstet Gynecol Reprod Biol. 149 (1): 97–101. doi:10.1016/j.ejogrb.2009.11.011. PMID 20018420.
- ↑ Krukenberg tumor. Wikipedia. https://en.wikipedia.org/wiki/Krukenberg_tumor#/media/File:Krukenberg_tumor_-3.jpg. Accessed on March 23, 2016
- ↑ Ovarian cancer. Wikipedia. https://en.wikipedia.org/wiki/Ovarian_cancer#Genetics Accessed on March 23, 2016.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 Image courtesy of Dr Hani Al Salam. Radiopaedia (original file ‘’here’’). Creative Commons BY-SA-NC
- ↑ Cho KC, Gold BM (1985). "Computed tomography of Krukenberg tumors". AJR Am J Roentgenol. 145 (2): 285–8. doi:10.2214/ajr.145.2.285. PMID 2992252.
- ↑ Jung SE, Lee JM, Rha SE, Byun JY, Jung JI, Hahn ST (2002). "CT and MR imaging of ovarian tumors with emphasis on differential diagnosis". Radiographics. 22 (6): 1305–25. doi:10.1148/rg.226025033. PMID 12432104.
- ↑ Ha HK, Baek SY, Kim SH, Kim HH, Chung EC, Yeon KM (1995). "Krukenberg's tumor of the ovary: MR imaging features". AJR Am J Roentgenol. 164 (6): 1435–9. doi:10.2214/ajr.164.6.7754887. PMID 7754887.
- ↑ Imaoka I, Wada A, Kaji Y, Hayashi T, Hayashi M, Matsuo M; et al. (2006). "Developing an MR imaging strategy for diagnosis of ovarian masses". Radiographics. 26 (5): 1431–48. doi:10.1148/rg.265045206. PMID 16973774.
![Bilateral ovarian neoplasm retaining the shape of ovary. Cut section of the tumor shows solid with mucinous areas[8]](/images/0/0c/Krukenberg_tumor_-3.jpg)
![X ray showing prominent small bowel loops filled with gas, no air-fluid level, no radiographic signs of intestinal obstruction[10]](/images/2/26/Krukenberg-tumour-2_%286%29.jpg)
![Large, solid, well defined bilateral ovarian masses[10]](/images/0/0b/Krukenberg-tumour-3.JPG)
![Large, solid, well defined bilateral ovarian masses[10]](/images/5/57/Krukenberg-tumour-3_%282%29.JPG)
![Large, solid, well defined bilateral ovarian masses[10]](/images/e/e6/Krukenberg-tumour-3_%283%29.JPG)
![Large, solid, well defined bilateral ovarian masses[10]](/images/4/4d/Krukenberg-tumour-3_%284%29.JPG)
![Krukenberg tumour of the right ovary from colon cancer[10]](/images/1/15/Kruckenberg-tumour.jpg)
![Coronal T2 image[10]](/images/7/77/Krukenberg-tumour-2_%281%29.jpg)
![Axial T1 image[10]](/images/6/63/Krukenberg-tumour-2_%282%29.jpg)
![Sagittal T2 image[10]](/images/a/af/Krukenberg-tumour-2_%283%29.jpg)
![Axial T2 image[10]](/images/a/a9/Krukenberg-tumour-2_%284%29.jpg)
![Axial T1 C+ fat sat dynamic contrast study image[10]](/images/0/08/Krukenberg-tumour-2_%285%29.jpg)