Intussusception (medical disorder): Difference between revisions
No edit summary |
|||
| Line 15: | Line 15: | ||
{{SI}} | {{SI}} | ||
{{CMG}} | {{CMG}} | ||
'''Associate Editor-In-Chief:''' {{CZ}} | |||
{{Editor Help}} | {{Editor Help}} | ||
Revision as of 03:06, 12 March 2009
Template:DiseaseDisorder infobox
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
An intussusception is a situation in which a part of the intestine has prolapsed into another section of intestine, similar to the way in which the parts of a collapsible telescope slide into one another.[1] The part which prolapses into the other is called the intussusceptum, and the part which receives it is called the intussuscipiens. The most frequent type of intussusception is one in which the ileum enters the cecum, however other types are known to occur, such as when a part of the ileum or jejunum prolapses into itself. Almost all intussusceptions occur with the intussusceptum having been located proximally to the intussuscipiens. The reason for this is that peristaltic action of the intestine pulls the proximal segment into the distal segment. There are, however, rare reports of the opposite being true.
Intussusception in humans is almost exclusively a disease of the young, usually those between 2 months and 36 months old. This may be a result of its link with certain childhood vaccinations. The CDC through the Federal Government of the United States through the National Vaccine Injury Compensation Program provides compensation for individuals who suffer intussusception as a result of their reaction to vaccines that contain "live, oral, rhesus-based rotavirus."[2]
Intussusception occurs more frequently in boys than in girls, with a ratio of approximately 3:1.[3]
In adults, intussusception represents the cause of approximately 1% of bowel obstructions and is frequently associated with neoplasm, malignant or otherwise.[4]
Symptoms
Early symptoms can include nausea, vomiting, pulling legs to the chest area, and intermittent moderate to severe cramping abdominal pain. Later signs include rectal bleeding, often with red currant jelly stool (stool mixed with blood and mucus), and lethargy. Physical examination may reveal a sausage-shaped mass felt upon palpation of the abdomen.
In children too young to communicate their symptoms verbally, they may cry, draw their knees up to their chest or experience dyspnea with paroxsyms of pain.
Fever is not a symptom of intussusception. However, intussusception can cause a loop of bowel to become necrotic. This leads to perforation and sepsis, which causes fever.
Diagnosis
Intussusception is often suspected based on history and physical exam, including observation of Dance's sign. Per rectal examination is particularly helpful in children as part of the intussusceptum may be felt by the finger.
A definite diagnosis often requires confirmation by diagnostic imaging modalities. Ultrasound is today considered the imaging modality of choice for diagnosis and exclusion of intussusception due to its high accuracy and lack of radiation. An x-ray of the abdomen may be indicated for evaluation of intestinal obstruction or the presence of free intraperitoneal gas; the latter finding would imply that bowel perforation has already occurred. In some institutions, air enema is used for diagnosis as the same procedure can be used for treatment.
Plain film
- May be normal
- Dilated small bowel and absence of gas in the region of the cecum.
- Occasionally, a mass impression within the colonic gas indicates an intraluminal mass created by the intussuscepting loop
Patient #1

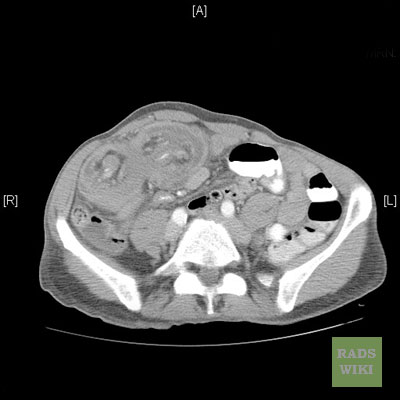
Patient #2: 65 y/o male with intermittent abdominal pain
-
Intussusception
-
Intussusception
-
Intussusception
Patient #3
-
Intussusception
-
Intussusception
-
Intussusception
-
Intussusception
-
Intussusception
-
Intussusception
-
Intussusception
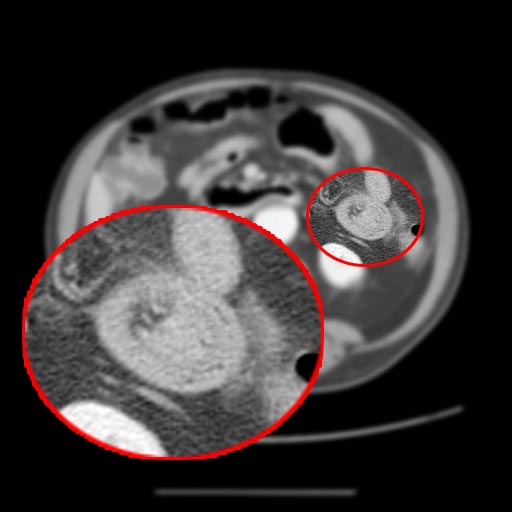
Patient #4: Colocolonic intussesception with a polyp as a lead point in a patient with Peutz-Jeghers syndrome
Treatment
When the condition is not immediately life-threatening, the intussusception is usually treated with either a barium enema or an air-contrast enema, which both confirms the diagnosis of intussusception, and in most cases successfully reduces it. The success rate is over 80%. However approximately 10% of these recur within 24 hours.
If it cannot be reduced by an enema or if the intestine is damaged, then a surgical reduction is necessary. In a surgical reduction, the abdomen is opened and the part that has telescoped in is pulled out manually by the surgeon or if the surgeon is unable to successfully reduce it or the bowel is damaged, the affected section will be resected. Often, the intussusception can be reduced by laparoscopy, whereby the segments of intestine are pulled apart by forceps.
Prognosis
Intussusception is a medical emergency, as it will eventually cause death if not reduced. When an intussusception or any other severe medical problem is suspected, the person must be taken to a hospital immediately.
The outlook for intussusception is excellent when treated quickly, but when untreated it can lead to death within 2–5 days. Fast treatment is a necessity, because the longer the intestine segment is prolapsed the longer it goes without bloodflow, and the less effective a non-surgical reduction will be. Prolonged intussusception also increases the likelihood of bowel ischemia and necrosis, requiring surgical resection.
Transient Intussusception
- Transient non obstructing intussusception without a lead point is known to occur in both adults and children and occurs more frequently than was previously reported. [5]
- Transient intussusception of the small bowel has been reported in adults with celiac disease and Crohn disease but is most frequently detected incidentally and is presumed to be innocuous.
- Intussusception without a lead point is known to appear as a non obstructing segment, usually smaller in diameter and shorter than an intussusception with a lead point.
-
Transient intussusception
-
Transient intussusception
-
Transient intussusception
-
Transient intussusception
References
- ↑ Template:Cite
- ↑ "Vaccines: documented risks". 2007. Retrieved 2007-11-15.
- ↑ Lonnie King, M.D., FACEP (2006). "Pediatrics: Intussusception". Retrieved 2006-06-05.
- ↑ Gayer G, Zissin R, Apter S, Papa M, Hertz M (2002). "Pictorial review: adult intussusception--a CT diagnosis". Br J Radiol. 75 (890): 185–90. PMID 11893645. Free Full Text.
- ↑ Young H. Kim, Michael A. Blake, Mukesh G. Harisinghani, Krystal Archer-Arroyo, Peter F. Hahn, Martha B. Pitman, and Peter R. Mueller. Adult Intestinal Intussusception: CT Appearances and Identification of a Causative Lead Point. RadioGraphics 2006 26: 733-744.
Template:Gastroenterology
Template:SIB