Intravenous leiomyomatosis: Difference between revisions
No edit summary |
Sunny Kumar (talk | contribs) No edit summary |
||
| Line 2: | Line 2: | ||
{{SI}} | {{SI}} | ||
1{{CMG}} '''Associate Editor-In-Chief:''' {{CZ}}; {{Ammu}} | 1{{CMG}} '''Associate Editor-In-Chief:''' {{CZ}}; {{Ammu}};{{Sonia Sandeep}} | ||
{{SK}} Nesidioblastoma, IVLM | {{SK}} Nesidioblastoma, IVLM | ||
Revision as of 04:31, 16 August 2019
1Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Ammu Susheela, M.D. [3];Template:Sonia Sandeep
Synonyms and keywords: Nesidioblastoma, IVLM
Overview
Intravenous leiomyomatosis is also refered as [IVL]. Intravenous leiomyomatosis is characterized by the extension into venous channels of histologically benign smooth muscle tumor arising from either the wall of a vessel or from a uterine leiomyoma. The etiology of intravenous leiomyomatosis is unclear. Intravenous leiomyomatosis must be differentiated from other diseases such as renal malignancies and sarcoma. The median age is 45 years, with patients ranging from 26 to 70 years old. Only females may develop intravenous leiomyomatosis. Common complications of intravenous leiomyomatosis include embolization, recurrence of the tumor, and metastasis. Surgery is the mainstay of therapy for intravenous leiomyomatosis. It can grow in to lymphatics /veins.[1]
Historical Perspective
- first described in 1896 German Pathologist Birch-Hirschfeld PMID 11904348
- first reported case of leiomyo-matosis of pelvic origin with intravascular extension to cardiac cavities was described in 1907 in Germany by Dürck and Hörmann. [2]
Pathophysiology
- Intravenous leiomyomatosis is characterized by the extension into venous channels of histologically benign smooth muscle tumor arising from either the wall of a vessel or from a uterine leiomyoma.[3]
- Approximately 40% of leiomyomata have cytogenetic abnormalities.
- They are benign tumors of uterus that extend to veins system but do not invade the surrounding tissues [4]
- They contains receptors to Estrogen and progesterone and hence response to these hormones [5]
- It is also referred as quasi-malignant behavior due to its speedy spreading behavior. PMID 11904348
- Patients are exclusively female, and the majority are white, premenopausal, and parous.PMID 12649198
- Intravenous leiomyomatosis should be considered in young women with cardiac symptoms who have a right atrial mass as well as a pelvic mass or who have previously undergone hysterectomy for leiomyoma uterus with intravenous involvement.(PMID 12508249)
Causes
- The etiology of intravenous leiomyomatosis is unclear.[6]
- Only two cytogenetic reports in IVL and both exhibited a karyotype with a der(14)t(12;14)(q15;q24) and two normal copies of chromosome 12 which has close association to uterine leiomyoma genetics
Differentiating Intravenous Leiomyomatosis from other Diseases
- Intravenous leiomyomatosis must be differentiated from other diseases such as:
- Renal malignancies
- Sarcoma
- Thrombosis of the intravenous catheter
Epidemiology and Demographics
- The median age is 45 years, with patients ranging from 26 to 70 years old. PMID: 7850080
- Female only are exclusively affected with intravenous leiomyomatosis.
Age
- Patients affected are of reproductive age group mostly around fifth decade of life.
- Age from 28 to 76 years (median, 42 years) (DOI: S0368-2315(04)96638-0)
Gender
- It is diagnosis only of female PMID: 18312983
Race
- They are seen more in white female.
Risk Factors
- Common risk factors in the development of intravenous leiomyomatosis are age, cytogenetics , and prior history,
Natural History, Complications and Prognosis
- The majority of patients with [IVL] remain asymptomatic for 10-15 years. PMID: 10805899
- The involvement seen is Right atrium 31 (45.6%), Right ventricle 31 (45.6%), Pulmonary vessel 6 (8.8%). PMID: 28414995
- Route of extension is seen Bilateral 4 (5.9%), Iliac only 32 (47.1%), Ovarian only 17 (25.0%) PMID: 28414995
- Early clinical features from complications include [Congestive heart failure] in 45 (66.1%), [Abdominal distension] in 10 (14.7%), and [Venous obstruction] in 4 (5.9%). Sudden death in 1 (1.5%). PMID: 28414995
- Prognosis is generally excellent.
- Common complications of intravenous leiomyomatosis include embolization, recurrence of the tumor, and metastasis.
- The tumor is slow growing, and the prognosis is favorable.
Diagnosis
Diagnostic Criteria
- There is no specific diagnostic Criteria for intravenous leiomyomatosis. Early diagnosis may be difficult because patients may be asymptomatic. How ever the diagnosis of intravenous leiomyomatosis is made when following findings are seen:
- benign tumors arising from smooth muscle of the uterus PMID: 24027407
- proliferating smooth muscle cells PMID: 20492407
- intravenous plug is mainly smooth muscle in origin PMID: 11904348
- tumor cells invaginating the vascular tree with no evidence of atypi PMID: 24027407
Symptoms
Patients may be asymptomatic or have symptoms of uterine leiomyomas, syncopal episodes, and dyspnea on exertion.PMID: 7820530 PMID: 15985146 PMID: 18312983
- Signs and Symptoms of intravenous Leiomyomatosis may include the following:
- Dyspnoea
- Syncope
- Oedema of the lower extremities
- Palpitation
- Fatigue
- Ascites
- Jugular vein distension
- Chest pain
- Abdominal pain
- Asymptomatic
Physical Examination
- Patients with intravenous Leiomyomatosis usually depends on location and extension which may include as :
- Iliac vein
- Ovarian vein
- Renal vein
- Both iliac and ovarian veins
- Gonadal vein
- Hypogastric vein
- Uterine vein
- Hypohepatic or hepatic vein
- Pelvic vein
- Intracardiac
- Right ventricle
- Pulmonary vessels
Laboratory Findings
- There are no specific laboratory findings associated with intravenous Leiomyomatosis. The corner stone of diagnosis of IVL is microscopic smooth muscle tumor in the absence of, or beyond the limits of, uterine leiomyoma. Most of the diagnosis is made after the patient is seen for symptoms making them suspension of extension of intravenous Leiomyomatosis. Differentiation between benign and malignant smooth muscle tumor can be difficult without biopsy.PMID: 11373202
- On microscopy it is seen as :
- benign, well-differentiated tumor
- smooth muscle growingwithin veins as worm-like projections
- Immunohistochemical studies show presence of desminand smooth muscle actin, confirming their smooth muscle nature.
- Tumor cells showed bizarre nuclear morphology with hyperchromatic multilobated nuclei, the mitotic activity was low, with mitotic index of less than 1 per 50 high-power fields
- It has been divided in subtitles based on microscopic appearance as namely, cellular, myxoid and bizarre,however it is not commonly used.
Imaging Findings
- Imaging is most helpful to make diagnosis of intravenous Leiomyomatosis however it depends on the location and extension of intravenous Leiomyomatosis to particular organ and location.PMID: 20409533
- Ultrasound scan, CT scan, magnetic resonance imaging, or venography are modalities to stratify the location and extension of of IVL.PMID: 12886157
- Multislice computed tomography (MSCT) displays the panorama of the lesions. PMID: 19001649
Treatment
Medical Therapy
- The mainstay of therapy for [IVL] is surgery.
Surgery
- Surgery is the treatment of choice, and complete removal of the tumor is mandatory.
- Recurrences up to 15 years after the primary occurrence in the patients with Incomplete resection of the tumor PMID: 25743551
- Bilateral oophorectomy causes shutdown of hormonal stimulation hence helps preventing recurrence.PMID: 16583249
- Surgical removal can be done in single or staged procedures,PMID: 12694674
- If staged procedure is chosen than it is done with abdominopelvic and intrathoracic components in two separate operations within a short time interval. PMID: 20802437
- In literature it is seen the Complete excision with one-stage operation was used in 19 (27.9%) and Complete excision with two-stage operation in 29 (42.7%)
Prevention
- There are no primary preventive measures available for [IVL].
References
- ↑ Mariyappa N, Manikyam UK, Krishnamurthy D, Preeti K, Agarwal Y, Prakar U (2012). "Intravenous leiomyomatosis". Niger J Surg. 18 (2): 105–6. doi:10.4103/1117-6806.103122. PMC 3762011. PMID 24027407.
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/23563052
- ↑ Mariyappa N, Manikyam UK, Krishnamurthy D, Preeti K, Agarwal Y, Prakar U (2012). "Intravenous leiomyomatosis". Niger J Surg. 18 (2): 105–6. doi:10.4103/1117-6806.103122. PMC 3762011. PMID 24027407.
- ↑ Dal Cin P, Quade BJ, Neskey DM, Kleinman MS, Weremowicz S, Morton CC (2003). "Intravenous leiomyomatosis is characterized by a der(14)t(12;14)(q15;q24)". Genes Chromosomes Cancer. 36 (2): 205–6. doi:10.1002/gcc.10159. PMID 12508249.
- ↑ Dal Cin P, Quade BJ, Neskey DM, Kleinman MS, Weremowicz S, Morton CC (2003). "Intravenous leiomyomatosis is characterized by a der(14)t(12;14)(q15;q24)". Genes Chromosomes Cancer. 36 (2): 205–6. doi:10.1002/gcc.10159. PMID 12508249.
- ↑ "Leiomyomas beyond the Uterus: Unusual Locations, Rare Manifestations1". line feed character in
|title=at position 18 (help)
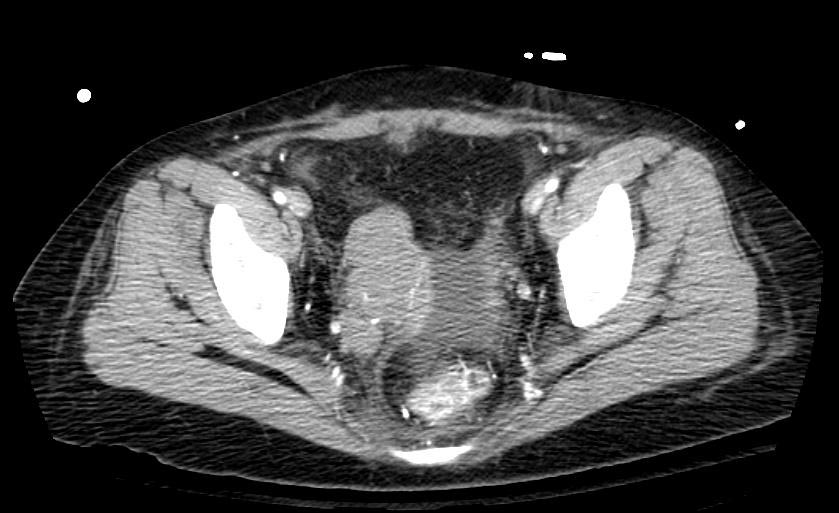
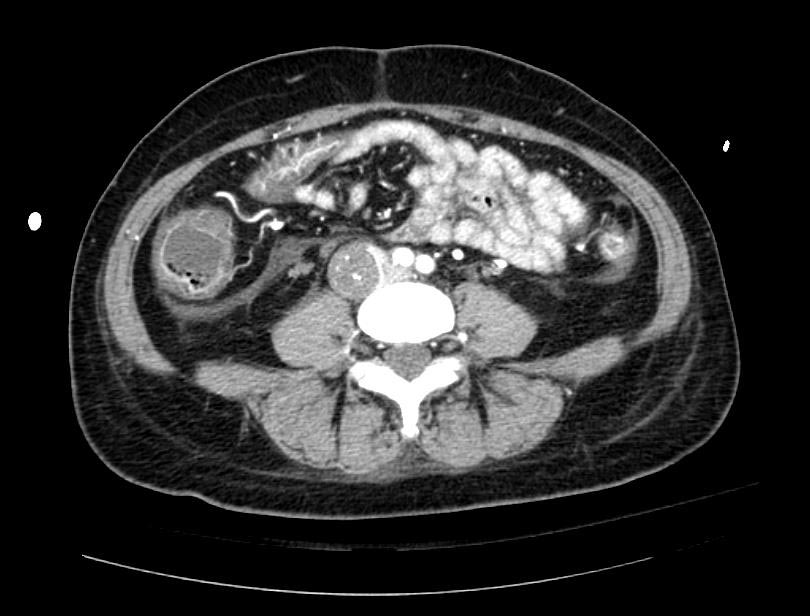
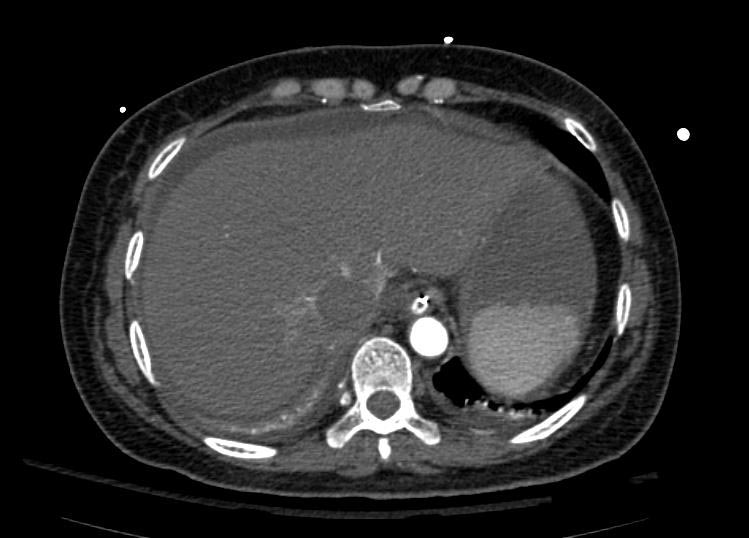
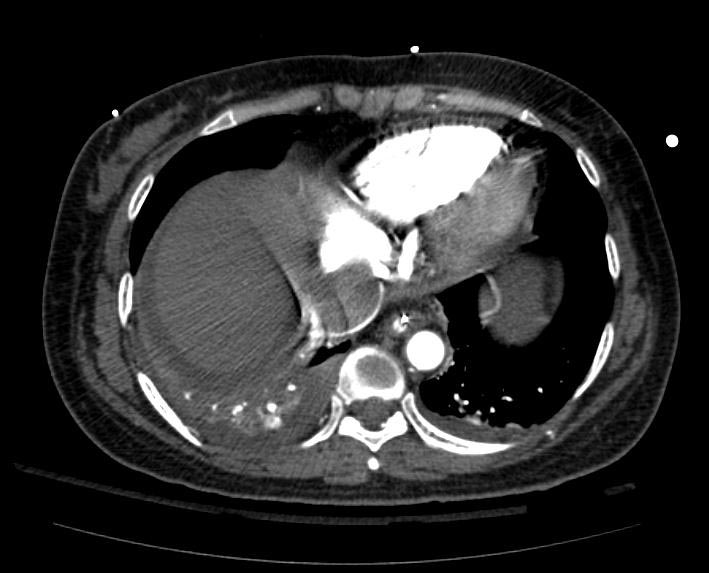
Images
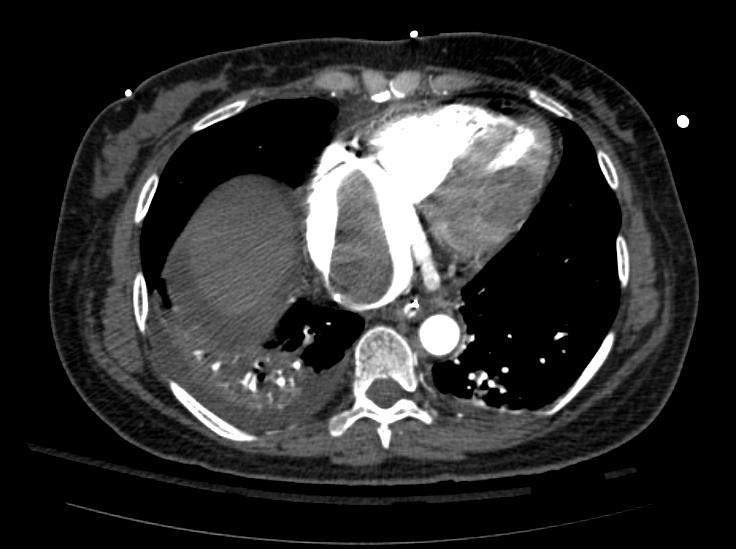
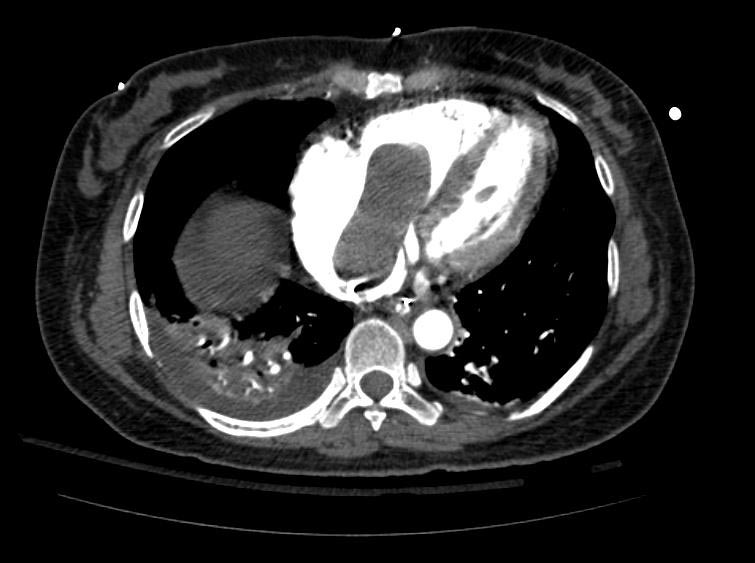
Example #1
The patient presented with S.O.B. one year after hysterectomy for a leiomyomatous uterus.
Treatment
- Surgery is the mainstay of therapy for intravenous leiomyomatosis.
Related Chapters
- Uterine leiomyoma
- Benign metastasizing leiomyoma