Intracranial pressure
| Intracranial pressure | |
 | |
|---|---|
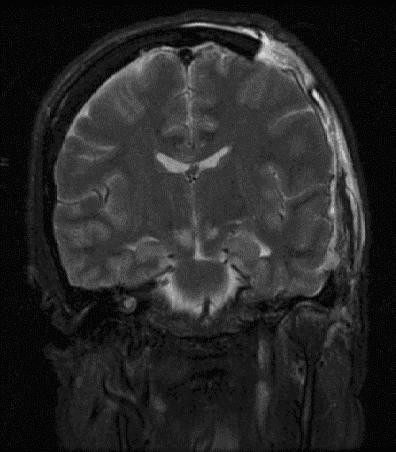
| Severely high ICP can cause herniation. |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Luke Rusowicz-Orazem, B.S.
Overview
Intracranial pressure, (ICP), is the pressure in the cranium and thus in the brain tissue and cerebrospinal fluid (CSF); this pressure is exerted on the brain's intracranial blood circulation vessels. ICP is maintained in a tight normal range dynamically, through the production and absorption of CSF. Because the entire system is contained by bone and strong ligamentous connections, the pressures of the body, such as those caused by straining, exercise, and coughing, do not affect the brain or its environment. ICP is measured in millimeters of mercury (mmHg) and, at rest, is normally 7–15 mmHg for a supine adult, and becomes negative (averaging −10 mmHg) in the vertical position.[1] Changes in ICP are attributed to volume changes in one or more of the constituents contained in the cranium.
Intracranial hypertension, commonly abbreviated IH, is elevation of the pressure in the cranium. ICP is normally 0–10 mm Hg; at 20–25 mm Hg, the upper limit of normal, treatment to reduce ICP is needed.[2]
The Monro-Kellie Hypothesis
The pressure-volume relationship between ICP, volume of CSF, blood, and brain tissue, and cerebral perfusion pressure (CPP) is known as the Monro-Kellie doctrine or the Monro-Kellie hypothesis.[3][4][5]
The Monro-Kellie hypothesis states that the cranial compartment is incompressible, and the volume inside the cranium is a fixed volume. The cranium and its constituents (blood, CSF, and brain tissue) create a state of volume equilibrium, such that any increase in volume of one of the cranial constituents must be compensated by a decrease in volume of another.[5]
The principal buffers for increased volumes include both CSF and, to a lesser extent, blood volume. These buffers respond to increases in volume of the remaining intracranial constituents. For example, an increase in lesion volume (e.g. epidural hematoma) will be compensated by the downward displacement of CSF and venous blood.[5] These compensatory mechanisms are able to maintain a normal ICP for any change in volume less than approximately 100–120 mL.
Increased ICP
One of the most damaging aspects of brain trauma and other conditions, directly correlated with poor outcome, is an elevated intracranial pressure.[6] ICP is very likely to cause severe harm if it rises beyond 40 mmHg in an adult.[7] Even intracranial pressures between 25 and 30 mm Hg are usually fatal if prolonged, except in children, who can tolerate higher pressures for longer periods.[8] An increase in pressure, most commonly due to head injury leading to intracranial hematoma or cerebral edema can crush brain tissue, shift brain structures, contribute to hydrocephalus, cause the brain to herniate, and restrict blood supply to the brain, leading to an ischemic cascade.[9]
Causes
Common Causes
- Aneurysm
- Arnold-chiari malformation
- Behçet's disease
- Brain tumor
- Cerebral edema
- Cerebral venous sinus thrombosis
- Choroid plexus tumor
- Chronic kidney disease
- Colloid cyst of third ventricle
- Contusions
- Crouzon craniofacial dysostosis
- Cushing's syndrome
- Dural arteriovenous fistula
- Encephalitis
- Epidural haemorrhage
- Epidural hematoma
- Erdheim-chester disease
- Excess cerebrospinal fluid
- Head trauma
- Hydrocephalus
- Hypertensive brain hemorrhage
- Hypertensive encephalopathy
- Idiopathic intracranial hypertension
- Insulin like growth factor 1
- Intracranial granuloma
- Intracranial haemorrhage
- Intraventricular hemorrhage
- Meningioma
- Meningitis
- Meningoencephalitis
- Multiple hamartoma syndrome
- Obstruction of superior mediastinal veins
- Obstruction of jugular veins
- Status epilepticus
- Stroke
- Subarachnoid haemorrhage
- Subdural haemorrhage
- Subdural hematoma
- Vasculitis
- Venous sinus thrombosis
Causes by Organ System
Causes in Alphabetical Order
- Abscess
- Accutane
- Acute liver failure
- Albendazole
- Aneurysm
- Arnold-chiari malformation
- Aschemic-anoxia states
- Behçet's disease
- Brain tumor
- Cerebral oedema
- Cerebral venous sinus thrombosis
- Choroid plexus tumor
- Chronic kidney disease
- Ciprofloxacin
- Claravis
- Colloid cyst of third ventricle
- Contusions
- Craniosynostosis
- Crouzon craniofacial dysostosis
- Cushing's syndrome
- Dandy-walker syndrome
- Dural arteriovenous fistula
- Encephalitis
- Epidural haemorrhage
- Epidural hematoma
- Erdheim-chester disease
- Excess cerebrospinal fluid
- Head trauma
- Heart failure
- Hepatic failure
- Hydrocephalus
- Hypercarbia
- Hypertension
- Hypertensive brain hemorrhage
- Hypertensive encephalopathy
- Hyperthyroidism
- Hypoparathyroidism
- Hypothyroidism
- Hypoxemia
- Idiopathic intracranial hypertension
- Infarction with edema
- Insulin like growth factor 1
- Intracranial abscess / granuloma
- Intracranial granuloma
- Intracranial haemorrhage
- Intracranial space-occupying lesion
- Intraventricular hemorrhage
- Iron deficiency
- Isotretinoin
- Lead
- Meningioma
- Meningitis
- Meningoencephalitis
- Minocycline
- Multiple hamartoma syndrome
- Neurocysticercosis
- Obstruction of superior mediastinal veins
- Obstruction of jugular veins
- Obstructive sleep apnea
- Pineal tumour
- Polycythaemia vera
- Pseudotumor cerebri
- Reye hepatocerebral syndrome
- Sotret
- Status epilepticus
- Stroke
- Subarachnoid haemorrhage
- Subdural haemorrhage
- Subdural hematoma
- Sudanophilic cerebral sclerosis
- Systemic lupus erythematosus
- Vasculitis
- Venous sinus thrombosis
- Vitamin a
Complete Differential Diagnosis of Increased Intracranial Pressure (ICP)
In alphabetical order. [10] [11]
- Acromegaly
- Addison's Disease
- Antiphospholipid Antibody Syndrome
- Arteriovenous malformation
- Brain abscess
- Cor pulmonale
- Cushing's Disease
- Decerebrate posture
- Decorticate posture
- Diabetic Ketoacidosis
- Drugs- Dexamethasone, Pergolide, toxins
- Epidural hemorrhage
- Encephalitis
- Hepatic encephalopathy
- HIV infection
- Hypercoagulable state
- Hyperosmolality
- Hyponatremia
- Hypoosmolality
- Hypoparathyroidism
- Hypothyroidism
- Hypoxic-ischemic injury
- Idiopathic intracranial hypertension
- Intraventricular hemorrhage
- Iron deficiency anemia
- Jugular vein cut
- Mastoiditis
- Meningitis
- Meningoencephalitis
- Obesity
- Orthostatic edema
- Otitis media
- Polycystic ovary syndrome
- Pregnancy
- Reye's Syndrome
- Severe head trauma
- Sleep Apnea
- Subdural hematoma
- Superior Vena Cava Syndrome
- Systemic Lupus Erythematosus
- Turner's Syndrome
- Water intoxication
Pathophysiology
The cranium and the vertebral body, along with the relatively inelastic dura, form a rigid container, such that the increase in any of its contents—brain, blood, or CSF—will increase the ICP. In addition, any increase in one of the components must be at the expense of the other two; this relationship is known as the Monro-Kellie doctrine. Small increases in brain volume do not lead to immediate increase in ICP because of the ability of the CSF to be displaced into the spinal canal, as well as the slight ability to stretch the falx cerebri between the hemispheres and the tentorium between the hemispheres and the cerebellum. However, once the ICP has reached around 25 mmHg, small increases in brain volume can lead to marked elevations in ICP.
Traumatic brain injury is a devastating problem with both high mortality and high subsequent morbidity. Injury to the brain occurs both at the time of the initial trauma (the primary injury) and subsequently due to ongoing cerebral ischemia (the secondary injury). Cerebral edema, hypotension, and axonal hypoxic conditions are well recognized causes of this secondary injury. In the intensive care unit, raised intracranial pressure (intracranial hypertension) is seen frequently after a severe diffuse brain injury (one that occurs over a widespread area) and leads to cerebral ischemia by compromising cerebral perfusion.
Cerebral perfusion pressure (CPP), the pressure causing blood flow to the brain, is normally fairly constant due to autoregulation, but for abnormal mean arterial pressure (MAP) or abnormal ICP the cerebral perfusion pressure is calculated by subtracting the intracranial pressure from the mean arterial pressure: CPP = MAP − ICP [1].[12] One of the main dangers of increased ICP is that it can cause ischemia by decreasing CPP. Once the ICP approaches the level of the mean systemic pressure, it becomes more and more difficult to squeeze blood into the intracranial space. The body’s response to a decrease in CPP is to raise blood pressure and dilate blood vessels in the brain. This results in increased cerebral blood volume, which increases ICP, lowering CPP further and causing a vicious cycle. This results in widespread reduction in cerebral flow and perfusion, eventually leading to ischemia and brain infarction. Increased blood pressure can also make intracranial hemorrhages bleed faster, also increasing ICP.
Highly increased ICP, if caused by a one-sided space-occupying process (e.g., hematoma) can result in midline shift, a dangerous condition in which the brain moves toward one side as the result of massive swelling in a cerebral hemisphere. Midline shift can compress the ventricles and lead to buildup of CSF.[13] Prognosis is much worse in patients with midline shift than in those without it. Another dire consequence of increased ICP combined with a space-occupying process is brain herniation (usually uncal or cerebellar), in which the brain is squeezed past structures within the skull, severely compressing it. If brainstem compression is involved, it may lead to decreased respiratory drive and is potentially fatal. This herniation is often referred to as "coning".
Major causes of morbidity due to increased intracranial pressure are due to global brain infarction as well as decreased respiratory drive due to brain herniation.
Intracranial Hypertension
Minimal increases in ICP due to compensatory mechanisms is known as stage 1 of intracranial hypertension. When the lesion volume continues to increase beyond the point of compensation, the ICP has no other resource, but to increase. Any change in volume greater than 100–120 mL would mean a drastic increase in ICP. This is stage 2 of intracranial hypertension. Characteristics of stage 2 of intracranial hypertension include compromise of neuronal oxygenation and systemic arteriolar vasoconstriction to increace MAP and CPP. Stage 3 intracranial hypertension is characterised by a sustained increased ICP, with dramatic changes in ICP with small changes in volume. In stage 3, as the ICP approaches the MAP, it becomes more and more difficult to squeeze blood into the intracranial space. The body’s response to a decrease in CPP is to raise blood pressure and dilate blood vessels in the brain. This results in increased cerebral blood volume, which increases ICP, lowering CPP further and causing a vicious cycle. This results in widespread reduction in cerebral flow and perfusion, eventually leading to ischemia and brain infarction. Neurologic changes seen in increased ICP are mostly due to hypoxia and hypercapnea and are as follows: decreased LOC, Cheyne-Stokes respirations, hyperventilation, sluggish dilated pupils and widened pulse pressure.
Causes of increased ICP
Causes of increased intracranial pressure can be classified by the mechanism in which ICP is increased:
- mass effect such as brain tumor, infarction with edema, contusions, subdural or epidural hematoma, or abscess all tend to deform the adjacent brain.
- generalized brain swelling can occur in ischemic-anoxia states, acute liver failure, hypertensive encephalopathy, pseudotumor cerebri, hypercarbia, and Reye hepatocerebral syndrome. These conditions tend to decrease the cerebral perfusion pressure but with minimal tissue shifts.
- increase in venous pressure can be due to venous sinus thrombosis, heart failure, or obstruction of superior mediastinal or jugular veins.
- obstruction to CSF flow and/or absorption can occur in hydrocephalus (blockage in ventricles or subarachnoid space at base of brain, e.g., by Arnold-Chiari malformation), extensive meningeal disease (e.g., infectious, carcinomatous, granulomatous, or hemorrhagic), or obstruction in cerebral convexities and superior sagittal sinus (decreased absorption).
- increased CSF production can occur in meningitis, subarachnoid hemorrhage, or choroid plexus tumor.
- Drugs Albendazole, Ciprofloxacin
Signs and symptoms of increased ICP
In general, symptoms and signs that suggest a rise in ICP including headache, nausea, vomiting, ocular palsies, altered level of consciousness, and papilledema. If papilledema is protracted, it may lead to visual disturbances, optic atrophy, and eventually blindness.
In addition to the above, if mass effect is present with resulting displacement of brain tissue, additional signs may include pupillary dilatation, abducens (CrN VI) palsies, and the Cushing's triad. Cushing's triad involves an increased systolic blood pressure, a widened pulse pressure, bradycardia, and an abnormal respiratory pattern.[14] In children, a slow heart rate is especially suggestive of high ICP.
Irregular respirations occur when injury to parts of the brain interfere with the respiratory drive. Cheyne-Stokes respiration, in which breathing is rapid for a period and then absent for a period, occurs because of injury to the cerebral hemispheres or diencephalon.[15] Hyperventilation can occur when the brain stem or tegmentum is damaged.[15]
As a rule, patients with normal blood pressure retain normal alertness with ICP of 25 to 40 mmHg (unless there's concurrent tissue shift). Only when ICP exceeds 40 to 50 mmHg do CPP and cerebral perfusion decrease to a level that results in loss of consciousness. Any further elevations will lead to brain infarction and brain death.
In infants and small children, the effects of ICP differ due to the fact that their cranial sutures have not closed. In infants, the fontanels, or soft spots on the head where the skull bones have not yet fused, bulge when ICP gets too high.
Treatment
In addition to management of the underlying causes, major considerations in acute treatment of increased ICP relates to the management of stroke and cerebral trauma.
One of the most important treatments for high ICP is to ensure adequate airway, breathing, and oxygenation, since inadequate oxygen levels or excess carbon dioxide cause cerebral blood vessels to dilate and ICP to rise.[16] Inadequate oxygen also forces brain cells to produce energy using anaerobic metabolism, which produces lactic acid and lowers pH, which dilates blood vessels.[6] On the other hand, blood vessels constrict when carbon dioxide levels are below normal, so hyperventilating a patient with a ventilator or bag valve mask can temporarily reduce ICP but limits blood flow to the brain in a time when the brain may already be ischemic. Artificially ventilating a patient at a fast rate used to be a standard part of head trauma treatment because of its ability to rapidly lower ICP, but the chance of developing ischemia was later recognized to be too much of a risk.[17] Furthermore, the brain adjusts to the new level of carbon dioxide after 48 to 72 hours of hyperventilation, which could cause the vessels to rapidly dilate if carbon dioxide levels were returned to normal too quickly.[17] Now hyperventilation is used when signs of brain herniation are apparent because the damage herniation can cause is so severe that it may be worthwhile to constrict blood vessels even if doing so reduces blood flow. Another way to lower ICP is to raise the head of the bed, allowing for venous drainage. A side effect of this is that it could lower pressure of blood to the head, resulting in inadequate blood supply to the brain. Another simple method used to lower ICP (particularly in trauma cases) is to loosen neck collars and clothing. This method is more useful is the patient is sedated and thus movement is minimal. Sandbags may be used to further limit neck movement.
In the hospital, blood pressure can be artificially raised in order to increase CPP, increase perfusion, oxygenate tissues, remove wastes and thereby lessen swelling.[17] Since hypertension is the body's way of forcing blood into the brain, medical professionals do not normally interfere with it when it is found in a head injured patient.[15] When it is necessary to decrease cerebral blood flow, MAP can be lowered using common antihypertensive agents such as calcium channel blockers.[6]
Struggling can increase metabolic demands and oxygen consumption, as well as increasing blood pressure.[18][16] Thus children may be paralyzed with drugs if other methods for reducing ICP fail. Paralysis allows the cerebral veins to drain more easily, but can mask signs of seizures, and the drugs can have other harmful effects.[16]
Pain is also treated to reduce agitation and metabolic needs of the brain, but some pain medications may cause low blood pressure and other side effects.[6]
Intracranial pressure can be measured continuously with intracranial transducers (only used in neurosurgical intensive care). A catheter can be surgically inserted into one of the brain's lateral ventricles and can be used to drain CSF (cerebrospinal fluid) in order to decrease ICP's. This type of drain is known as an EVD (extraventricular drain).[6] In rare situations when only small amounts of CSF are to be drained to reduce ICP's, drainage of CSF via lumbar puncture can be used as a treatment.
Craniotomies are holes drilled in the skull to remove intracranial hematomas or relieve pressure from parts of the brain.[6] As raised ICP's may be caused by the presence of a mass, removal of this via craniotomy will decrease raised ICP's.
A drastic treatment for increased ICP is decompressive craniectomy, in which a part of the skull is removed and the dura mater is expanded to allow the brain to swell without crushing it or causing herniation.[17] The section of bone removed, known as a bone flap, can be stored in the patient's abdomen and resited back to complete the skull once the acute cause of raised ICP's has resolved.
Contraindicated medications
Increased intracranial pressure is considered an absolute contraindication to the use of the following medications:
Low ICP
It is also possible for the intracranial pressure to drop below normal levels, though increased intracranial pressure is a far more common (and far more serious) sign. The symptoms for both conditions are often the same, leading many medical experts to believe that it is the change in pressure rather than the pressure itself causing the above symptoms.
Spontaneous intracranial hypotension may occur as a result of an occult leak of CSF into another body cavity. More commonly, decreased ICP is the result of lumbar puncture or other medical procedures involving the brain or spinal cord. Various medical imaging technologies exist to assist in identifying the cause of decreased ICP. Often, the syndrome is self-limiting, especially if it is the result of a medical procedure. If persistent intracranial hypotension is the result of a lumbar puncture, a "blood patch" may be applied to seal the site of CSF leakage. Various medical treatments have been proposed; only the intravenous administration of caffeine and theophylline has shown to be particularly useful.[19]
References
- ↑ 1.0 1.1 Steiner LA, Andrews PJ (2006). "Monitoring the injured brain: ICP and CBF". British Journal of Anaesthesia. 97 (1): 26–38. doi:10.1093/bja/ael110. PMID 16698860.
- ↑
Ghajar J (2000). "Traumatic brain injury". Lancet. 356 (9233): 923–9. doi:10.1016/S0140-6736(00)02689-1. PMID 11036909. Unknown parameter
|month=ignored (help) - ↑ Monro A (1783). Observations on the structure and function of the nervous system. Edinburgh: Creech & Johnson.
- ↑ Kelly G (1824). "Appearances observed in the dissection of two individuals; death from cold and congestion of the brain". Trans Med Chir Sci Edinb. 1: 84–169.
- ↑ 5.0 5.1 5.2 Mokri B (2001). "The Monro-Kellie hypothesis: applications in CSF volume depletion". Neurology. 56 (12): 1746–8. PMID 11425944. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Orlando Regional Healthcare, Education and Development. 2004. "Overview of Adult Traumatic Brain Injuries." Accessed September 6, 2007.
- ↑ Dawodu S. 2005. "Traumatic Brain Injury: Definition, Epidemiology, Pathophysiology" Emedicine.com.Accessed January 4, 2007.
- ↑ Tolias C and Sgouros S. 2006. "Initial Evaluation and Management of CNS Injury." Emedicine.com. Accessed January 4, 2007.
- ↑ Graham DI and Gennareli TA. Chapter 5, "Pathology of Brain Damage After Head Injury" In, Cooper P and Golfinos G. 2000. Head Injury, 4th Ed. Morgan Hill, New York.
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ Duschek S, Schandry R (2007). "Reduced brain perfusion and cognitive performance due to constitutional hypotension". Clinical Autonomic Research. 17 (2): 69–76. doi:10.1007/s10286-006-0379-7. PMC 1858602. PMID 17106628.
- ↑ Downie A. 2001. "Tutorial: CT in Head Trauma" Accessed January 4, 2007.
- ↑ Sanders MJ and McKenna K. 2001. Mosby’s Paramedic Textbook, 2nd revised Ed. Chapter 22, "Head and Facial Trauma." Mosby.
- ↑ 15.0 15.1 15.2 Singh J and Stock A. 2006. "Head Trauma." Emedicine.com. Accessed January 4, 2007.
- ↑ 16.0 16.1 16.2 Su F and Huh J. 2006. "Neurointensive Care for Traumatic Brain Injury in Children." Emedicine.com. Accessed January 4, 2007.
- ↑ 17.0 17.1 17.2 17.3 Shepherd S. 2004. "Head Trauma." Emedicine.com. Accessed January 4, 2007.
- ↑ Bechtel K. 2004. "Pediatric Controversies: Diagnosis and Management of Traumatic Brain Injuries." Trauma Report. Supplement to Emergency Medicine Reports, Pediatric Emergency Medicine Reports, ED Management, and Emergency Medicine Alert. Volume 5, Number 3. Thomsom American Health Consultants.
- ↑ Paldino M, Mogilner AY, Tenner MS (2003). "Intracranial hypotension syndrome: a comprehensive review". Neurosurg Focus. 15 (6): ECP2. doi:10.3171/foc.2003.15.6.8. PMID 15305844. Unknown parameter
|month=ignored (help)
Additional Resources
- Monroe A. Observations on the structure and function of the nervous system, Edinburgh: Creech & Johnson; 1783.
- Kelly G. An account of the appearances observed in the dikssection of two of three individuals presumed to have perished in the storm of the 3rd, and whose bodies were deiscovered in the vicinity of the Leith on the morning of the 4th of November 1821, with some reflections on the pathology of the brain, Trans Med Chir Sci Edinb 1824;1:84–169.
External links
- Gruen P. 2002. "Monro-Kellie Model" Neurosurgery Infonet. USC Neurosurgery. Accessed January 4, 2007.
- National Guideline Clearinghouse. 2005. Guidelines for the management of severe traumatic brain injury. Firstgov. Accessed January 4, 2007.