Insulinoma pathophysiology: Difference between revisions
| Line 28: | Line 28: | ||
*Insulinoma is a rare benign [[pancreatic neuroendocrine tumor]] that arises from B islet cells, which are cells that are normally involved in the production of [[insulin]]. Few insulinomas can also produce other hormones such as [[Serotonin]], [[gastrin]], [[ACTH]], [[glucagon]], and [[somatostatin]] <ref name="AlJadir2015">{{cite journal|last1=AlJadir|first1=Saadi|title=Insulinoma: Literature’s Review (Part 1)|journal=Endocrinology&Metabolism International Journal|volume=2|issue=3|year=2015|issn=24730815|doi=10.15406/emij.2015.02.00025}}</ref> | *Insulinoma is a rare benign [[pancreatic neuroendocrine tumor]] that arises from B islet cells, which are cells that are normally involved in the production of [[insulin]]. Few insulinomas can also produce other hormones such as [[Serotonin]], [[gastrin]], [[ACTH]], [[glucagon]], and [[somatostatin]] <ref name="AlJadir2015">{{cite journal|last1=AlJadir|first1=Saadi|title=Insulinoma: Literature’s Review (Part 1)|journal=Endocrinology&Metabolism International Journal|volume=2|issue=3|year=2015|issn=24730815|doi=10.15406/emij.2015.02.00025}}</ref> | ||
* They are usually small(90%), sporadic(90%), solitary(90%) and benign(90%) tumors. Those associated with the MEN1 syndrome are usually malignant and higher recurrence rate(21% at 10 and 20 years) than in those without [[MEN I]] (5% at 10 and 7% at 20 years). <ref name="pmid1677058">{{cite journal| author=Service FJ, McMahon MM, O'Brien PC, Ballard DJ| title=Functioning insulinoma--incidence, recurrence, and long-term survival of patients: a 60-year study. | journal=Mayo Clin Proc | year= 1991 | volume= 66 | issue= 7 | pages= 711-9 | pmid=1677058 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1677058 }} </ref>. | * They are usually small(90%), sporadic(90%), solitary(90%) and benign(90%) tumors. Those associated with the MEN1 syndrome are usually malignant and higher recurrence rate(21% at 10 and 20 years) than in those without [[MEN I]] (5% at 10 and 7% at 20 years). <ref name="pmid1677058">{{cite journal| author=Service FJ, McMahon MM, O'Brien PC, Ballard DJ| title=Functioning insulinoma--incidence, recurrence, and long-term survival of patients: a 60-year study. | journal=Mayo Clin Proc | year= 1991 | volume= 66 | issue= 7 | pages= 711-9 | pmid=1677058 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1677058 }} </ref>. | ||
*It is thought that insulinoma is mediated by mTOR/P70S6K signaling pathway. Inhibitors of mTOR(rapamycin) or dual PI3K/mTOR(NVP-BEZ2235)thus have become new drugs for treating insulinoma. An oral mTOR inhibitor, Everolimus, make better glycemic control in people having insulinoma.<ref name="pmid19129539">{{cite journal| author=Kulke MH, Bergsland EK, Yao JC| title=Glycemic control in patients with insulinoma treated with everolimus. | journal=N Engl J Med | year= 2009 | volume= 360 | issue= 2 | pages= 195-7 | pmid=19129539 | doi=10.1056/NEJMc0806740 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19129539 }} </ref> The pathway will give more possibilities for medical treatment.<ref name="pmid22711648">{{cite journal| author=Zhan HX, Cong L, Zhao YP, Zhang TP, Chen G, Zhou L et al.| title=Activated mTOR/P70S6K signaling pathway is involved in insulinoma tumorigenesis. | journal=J Surg Oncol | year= 2012 | volume= 106 | issue= 8 | pages= 972-80 | pmid=22711648 | doi=10.1002/jso.23176 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22711648 }} </ref> | *It is thought that insulinoma is mediated by mTOR/P70S6K signaling pathway. Inhibitors of mTOR(rapamycin) or dual PI3K/mTOR(NVP-BEZ2235)thus have become new drugs for treating insulinoma. An oral mTOR inhibitor, Everolimus, make better glycemic control in people having insulinoma.<ref name="pmid19129539">{{cite journal| author=Kulke MH, Bergsland EK, Yao JC| title=Glycemic control in patients with insulinoma treated with everolimus. | journal=N Engl J Med | year= 2009 | volume= 360 | issue= 2 | pages= 195-7 | pmid=19129539 | doi=10.1056/NEJMc0806740 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19129539 }} </ref> The pathway will give more possibilities for medical treatment.<ref name="pmid22711648">{{cite journal| author=Zhan HX, Cong L, Zhao YP, Zhang TP, Chen G, Zhou L et al.| title=Activated mTOR/P70S6K signaling pathway is involved in insulinoma tumorigenesis. | journal=J Surg Oncol | year= 2012 | volume= 106 | issue= 8 | pages= 972-80 | pmid=22711648 | doi=10.1002/jso.23176 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22711648 }} </ref> | ||
Revision as of 16:55, 17 August 2017
|
Insulinoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Insulinoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Insulinoma pathophysiology |
|
Risk calculators and risk factors for Insulinoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Amandeep Singh M.D.[2]Parminder Dhingra, M.D. [3]
Overview
Insulinoma may occur as part of other genetic syndromes such as multiple endocrine neoplasia type 1 and von Hippel-Lindau syndrome. On microscopic histopathological analysis, solid or gyriform patterns, usually without glands are characteristic findings of insulinoma.
Genetics
- Insulinoma can occur in association with inherited syndromes, such as multiple endocrine neoplasia type 1, von Hippel-Lindau syndrome or sporadic.[1]
- Multiple endocrine neoplasia type 1 is an autosomal dominant disorder caused by alterations of the MEN1 gene located at chromosomal region 11q13.
Microscopic Pathology
On microscopic histopathological analysis characteristic findings of insulinoma are:
- Solid or gyriform patterns, usually without glands
Overview
- The exact pathogenesis of [disease name] is not fully understood.
OR
- It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
- [Pathogen name] is usually transmitted via the [transmission route] route to the human host.
- Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
- [Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
- The progression to [disease name] usually involves the [molecular pathway].
- The pathophysiology of [disease/malignancy] depends on the histological subtype.
Pathophysiology
Pathogenesis
- Insulinoma is a rare benign pancreatic neuroendocrine tumor that arises from B islet cells, which are cells that are normally involved in the production of insulin. Few insulinomas can also produce other hormones such as Serotonin, gastrin, ACTH, glucagon, and somatostatin [2]
- They are usually small(90%), sporadic(90%), solitary(90%) and benign(90%) tumors. Those associated with the MEN1 syndrome are usually malignant and higher recurrence rate(21% at 10 and 20 years) than in those without MEN I (5% at 10 and 7% at 20 years). [3].
- It is thought that insulinoma is mediated by mTOR/P70S6K signaling pathway. Inhibitors of mTOR(rapamycin) or dual PI3K/mTOR(NVP-BEZ2235)thus have become new drugs for treating insulinoma. An oral mTOR inhibitor, Everolimus, make better glycemic control in people having insulinoma.[4] The pathway will give more possibilities for medical treatment.[5]
- The progression to hypoglycemia is actually because of decreased glucose synthesis rather than increased use due to the direct effect of insulin on the liver.[7]
Genetics
- Insulinoma is transmitted in [mode of genetic transmission] pattern.
- Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3].
- The development of [disease name] is the result of multiple genetic mutations.
Associated Conditions
- Other pancreatic neuroendocrine tumors like gastrinoma, glucagonoma, VIPoma, somatostatinoma
- MEN 1[3]
- von Hippel-Lindau
- Neurofibromatosis type 1
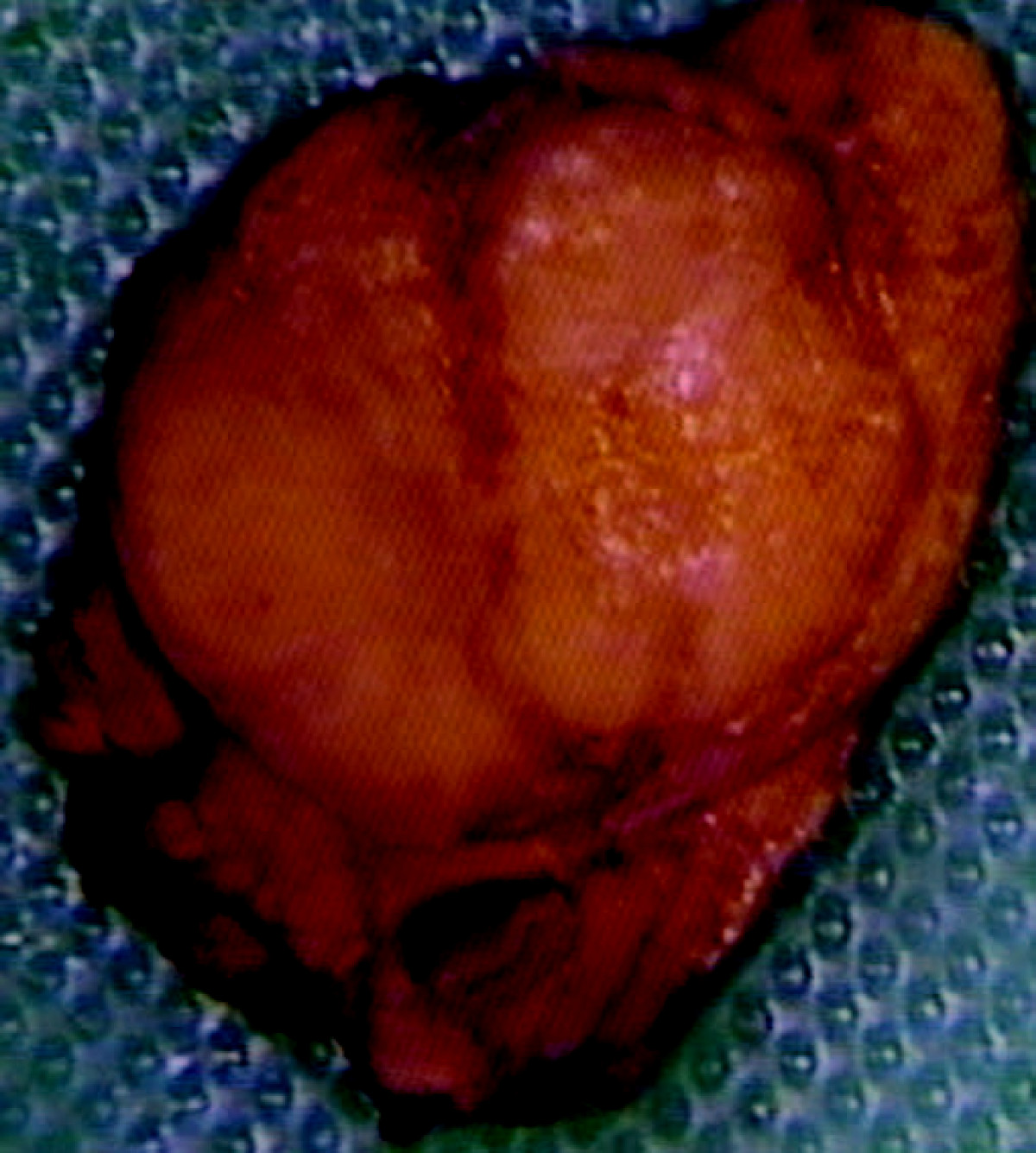
Gross Pathology
- On gross pathology insulinomas have a red brown appearance, are usually solitary, can be present anywhere in the pancreas(extrapancreatic are very rare).
Microscopic Pathology
- On microscopic histopathological analysis, [feature2], and [feature3] are characteristic findings of insulinoma.
-
Histopathology of pancreatic endocrine tumor (insulinoma). H&E stain[8]
-
Histopathology of pancreatic endocrine tumor (insulinoma)[8]
-
Histopathology of pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain[8]
-
Histopathology of pancreatic endocrine tumor (insulinoma). Insulin immunostain[8]
References
- ↑ Murray PD, McKenzie DT, Swain SL, Kagnoff MF (1987). "Interleukin 5 and interleukin 4 produced by Peyer's patch T cells selectively enhance immunoglobulin A expression". J Immunol. 139 (8): 2669–74. PMID 3498768.
- ↑ AlJadir, Saadi (2015). "Insulinoma: Literature's Review (Part 1)". Endocrinology&Metabolism International Journal. 2 (3). doi:10.15406/emij.2015.02.00025. ISSN 2473-0815.
- ↑ 3.0 3.1 Service FJ, McMahon MM, O'Brien PC, Ballard DJ (1991). "Functioning insulinoma--incidence, recurrence, and long-term survival of patients: a 60-year study". Mayo Clin Proc. 66 (7): 711–9. PMID 1677058.
- ↑ Kulke MH, Bergsland EK, Yao JC (2009). "Glycemic control in patients with insulinoma treated with everolimus". N Engl J Med. 360 (2): 195–7. doi:10.1056/NEJMc0806740. PMID 19129539.
- ↑ Zhan HX, Cong L, Zhao YP, Zhang TP, Chen G, Zhou L; et al. (2012). "Activated mTOR/P70S6K signaling pathway is involved in insulinoma tumorigenesis". J Surg Oncol. 106 (8): 972–80. doi:10.1002/jso.23176. PMID 22711648.
- ↑ Cao, Yanan; Gao, Zhibo; Li, Lin; Jiang, Xiuli; Shan, Aijing; Cai, Jie; Peng, Ying; Li, Yanli; Jiang, Xiaohua; Huang, Xuanlin; Wang, Jiaqian; Wei, Qing; Qin, Guijun; Zhao, Jiajun; Jin, Xiaolong; Liu, Li; Li, Yingrui; Wang, Weiqing; Wang, Jun; Ning, Guang (2013). "Whole exome sequencing of insulinoma reveals recurrent T372R mutations in YY1". Nature Communications. 4. doi:10.1038/ncomms3810. ISSN 2041-1723.
- ↑ Rizza, R. A.; Haymond, M. W.; Verdonk, C. A.; Mandarino, L. J.; Miles, J. M.; Service, F. J.; Gerich, J. E. (1981). "Pathogenesis of Hypoglycemia in Insulinoma Patients: Suppression of Hepatic Glucose Production by Insulin". Diabetes. 30 (5): 377–381. doi:10.2337/diab.30.5.377. ISSN 0012-1797.
- ↑ 8.0 8.1 8.2 8.3 Neuroendocrine tumour of the pancreas. Libre Pathology. http://librepathology.org/wiki/index.php/Neuroendocrine_tumour_of_the_pancreas
![Histopathology of pancreatic endocrine tumor (insulinoma). H&E stain[8]](/images/2/2d/Pancreatic_insulinoma_Histology_1.JPG)
![Histopathology of pancreatic endocrine tumor (insulinoma)[8]](/images/2/2f/Pancreatic_insulinoma_histology_2.JPG)
![Histopathology of pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain[8]](/images/a/a3/Pancreatic_insulinoma_histopathology_3.JPG)
![Histopathology of pancreatic endocrine tumor (insulinoma). Insulin immunostain[8]](/images/d/d5/Pancreatic_insulinoma_histology_4.JPG)