In vitro fertilization procedure
|
In vitro fertilization Microchapters |
|
Case Studies |
|---|
|
In vitro fertilization procedure On the Web |
|
American Roentgen Ray Society Images of In vitro fertilization procedure |
|
Risk calculators and risk factors for In vitro fertilization procedure |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4]
Overview
Procedure
Ovarian Stimulation
Treatment cycles are typically started on the third day of menstruation and consist of a regimen of fertility medications to stimulate the development of multiple follicles of the ovaries. In most patients injectable gonadotropins (usually FSH analogues) are used under close monitoring. Such monitoring frequently checks the estradiol level and, by means of gynecologic ultrasonography, follicular growth. Usually injections for 10 days are necessary. Spontanenous ovulation during the cycle is prevented by the use of GnRH agonists or GnRH antagonists, which block the natural surge of luteinizing hormone (LH).
Oocyte Retrieval
When follicular maturation is judged to be adequate, human chorionic gonadotropin (β-hCG) is given. This agent, which acts as an analogue of luteinizing hormone, would cause ovulation about 36 hours after injection, but a retrieval procedure takes place just prior to that, in order to recover the egg cells from the ovary. The eggs are retrieved from the patient using a transvaginal technique involving an ultrasound-guided needle piercing the vaginal wall to reach the ovaries. Through this needle follicles can be aspirated, and the follicular fluid is handed to the IVF laboratory to identify ova. The retrieval procedure takes about 20 minutes and is usually done under conscious sedation or general anesthesia.
Fertilization
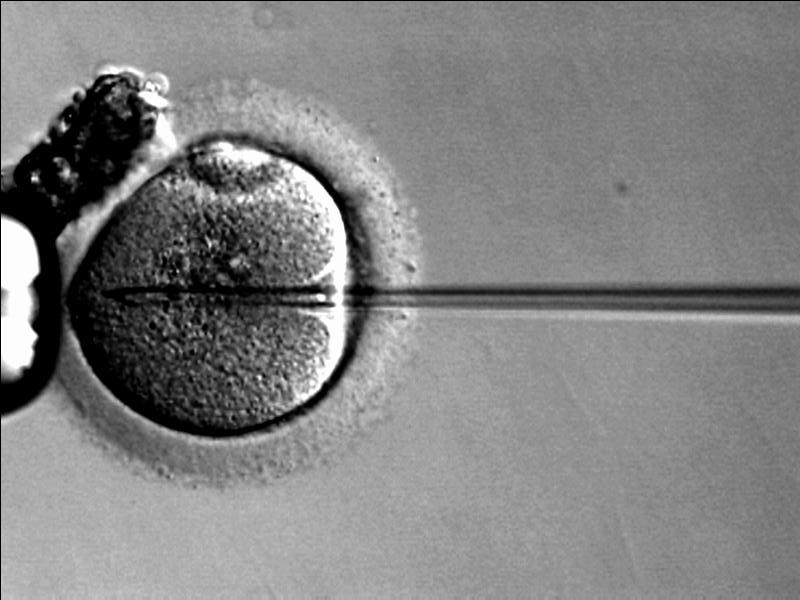
In the laboratory, the identified eggs are stripped of surrounding cells and prepared for fertilisation. In the meantime, semen is prepared for fertilization by removing inactive cells and seminal fluid. The sperm and the egg are incubated together (at a ratio of about 75,000:1) in the culture media for about 18 hours. By that time fertilization should have taken place and the fertilised egg would show two pronuclei. In situations where the sperm count is low, a single sperm is injected directly into the egg using intracytoplasmic sperm injection (ICSI). The fertilised egg is passed to a special growth medium and left for about 48 hours until the egg has reached the 6-8 cell stage.

Selection
Laboratories have developed grading methods to judge oocyte and embryo quality. Typically, embryos that have reached the 6-8 cell stage are transferred three days after retrieval. In many American and Australian programmes, however, embryos are placed into an extended culture system with a transfer done at the blastocyst stage, especially if many good-quality day-3 embryos are available. Blastocyst stage transfers have been shown to result in higher pregnancy rates.[1]. In Europe, day-2 transfers are common.
Embryo Transfer
Embryos are graded by the embryologist based on the number of cells, evenness of growth and degree of fragmentation. The number to be transferred depends on the number available, the age of the woman and other health and diagnostic factors. In countries such as the UK, Australia and New Zealand, a maximum of two embryos are transferred except in unusual circumstances. For instance, a woman over 35 may have up to three embryos transferred. This is to limit the number of multiple pregnancies. The embryos judged to be the "best" are transferred to the patient's uterus through a thin, plastic catheter, which goes through her vagina and cervix. Several embryos may be passed into the uterus to improve chances of implantation and pregnancy.

Post Transfer
The patient has to wait two weeks before she returns to the clinic for the pregnancy test. During this time she may receive progesterone—a hormone that keeps the uterus lining thickened and suitable for implantation. Many IVF programmes provide additional medications as part of their protocol.
Cryopreservation
Embryo cryopreservation
If multiple embryos are generated, patients may choose to freeze embryos that are not transferred. Those embryos are placed in liquid nitrogen and can be preserved for a long time. There are currently 500,000 frozen embryos in the United States.[5] The advantage is that patients who fail to conceive may become pregnant using such embryos without having to go through a full IVF cycle. Or, if pregnancy occurred, they could return later for another pregnancy.
Oocyte Cryopreservation
Cryopreservation of unfertilised mature oocytes has been successfully accomplished, e.g. in women who are likely to lose their ovarian reserve due to undergoing chemotherapy.[2]
Ovarian Tissue Cryopreservation
Cryopreservation of ovarian tissue is of interest to women who want to preserve their reproductive function beyond the natural limit, or whose reproductive potential is threatened by cancer therapy. Research on this issue is promising.
Adjunctive Interventions
There are several variations or improvements of IVF, such as ICSI, ZIFT, GIFT and PGD. An increasing number of fertility specialists and centers offer acupuncture as a part of their IVF protocol, or maintain a list of acupuncturists specializing in infertility.
ICSI
Intracytoplasmic sperm injection (ICSI) is a more recent development associated with IVF which allows the sperm to be directly injected in to the egg using micromanipulation. This is used for sperm that have difficulty penetrating the egg and when sperm numbers are very low. ICSI results in success rates equal to IVF fertilisation.
ZIFT
In Zygote intrafallopian transfer (ZIFT) eggs are removed from the woman, fertilized and then placed in the woman's fallopian tubes rather than the uterus.
GIFT
In gamete intrafallopian transfer (GIFT) eggs are removed from the woman, and placed in one of the fallopian tubes, along with the man's sperm. This allows fertilization to take place inside the woman's body. Therefore, this variation is actually an in vivo fertilisation, and not an in vitro fertilisation.
PGD
PGD can be performed on embryos prior to the embryo transfer. A similar, but more general test has been developed called Preimplantation Genetic Haplotyping (PGH).
Acupuncture
An increasing number of fertility specialists and centers recognize the benefits of acupuncture and offer acupuncture as a part of their IVF protocol. Limited but supportive[3] evidence from clinical trials and case series suggests that acupuncture may improve the success rate of IVF and the quality of life[3] of patients undergoing IVF and that it is a safe[3] adjunct therapy.
Mechanism of acupuncture
Scientific literature lists four[3] mechanisms of how acupuncture can improve IVF outcomes ; these include
- Neuroendicrinological modulations
- Increased blood flow to uterus and ovaries
- Modulation in cytokines
- Reducing stress, anxiety and depression
Studies
Summarizing four acupuncture trials published in peer reviewed scientific journal Fertility and sterility, involving a total of just under 800 women, the results clearly showed a pregnancy was twice as likely to occur in the acupuncture group compared to the control group[6]. Many fertility specialists recognize the positive role of acupuncture, although there are some methodological issues to be taken into account when assessing non-pharmacological studies, furthermore there are issues when assessing effectiveness of acupuncture, as the treatment is performed in person and is very difficult to fake acupuncture. Even the fake needles used in acupuncture trials as a placebo are considered to be able to produce a therapeutic effect through acupressure, making the research even more difficult.
Following are examples of individual studies.
According to a report published in Fertility and Sterility, if done correctly, Acupuncture significantly improves IVF success rate[7].
Researchers in Adelaide has evaluated the effect of acupuncture on women undergoing IVF, and couldn't exclude a smaller treatment effect. However, there was no (statistically) significant difference compared to a control group of women not getting acupuncture[4]
A randomized, prospective study [8] showed that acupuncture significantly (p<0.01) increased IVF implantation rates and pregnancy rates. Positive trends were also observed in miscarriage rates although the results were not statistically significant. The study has been criticized by one scientist for lacking traditional scientific practices when interpreting the data [5], and by another scientist that positive impact of acupuncture on IVF success rates is not definitive. [6]. However, assessments of nonpharmacological treatments must take into consideration additional methodological issues. This criticism is possibly arising from lack of understanding of methodological differences in clinical trials evaluating nonpharmacological and pharmacological treatments[7] and in particular methodological issues in trials of acupuncture [8].
Electro-acupuncture in oocyte retrieval for IVF
Electro-acupuncture has a proven analgesic effect in oocyte retrieval for IVF.
Complementary medicines
Infertility patients commonly use complementary medicines. Health-care practitioners and fertility specialists need to be proactive in acquiring and documenting the use of these practices. There is a need to provide further information to patients on the use of CMs and therapies. Further research examining the reasons for use of CMs and therapies is needed.[9]
Hypnosis
A study of hypnotherapy suggests a higher success rate when integrated with treatment [10]. However, this study is not without criticism. Experts say the study failed to take into account key differences between the groups compared in the study. These differences would have had a major influence on their chances of conceiving [9].
References
- ↑ Papanikolaou EG, Camus M, Kolibianakis EM, Van Landuyt L, Van Steirteghem A, Devroey P (2006). "In Vitro Fertilization with Single Blastocyst-Stage versus Single Cleavage-Stage Embryos". N Engl J Med. 354: 1139. PMID 16540614.
- ↑ Porcu E, Fabbri R, Damiano G, Fratto R, Giunchi S, Venturoli S (2004). "Oocyte cryopreservation in oncological patients". Eur J Obstet Gynecol Reprod Biol. 113 Suppl 1: S14–6. PMID 15041124.
- ↑ 3.0 3.1 3.2 3.3 [1] Anderson BJ, Haimovici F, Ginsburg ES, Schust DJ, Wayne PM. Pacific College of Oriental Medicine, New York, USA.
- ↑ [2] Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer. Smith C, Coyle M, Norman RJ. School of Health Science, The University of South Australia, South Australia, Australia. caroline.smith@acnhw.com.au
- ↑ [3] Collins J. Department of Obstetrics and Gynecology, McMaster University, Hamilton, Ontario, Canada. collinsj@auracom.com
- ↑ Domar AD. Domar Center for Complementary Healthcare, Boston IVF, Massachusetts, USA. Domar@domarcenter.com
- ↑ Methodological Differences in Clinical Trials Evaluating Nonpharmacological and Pharmacological Treatments of Hip and Knee Osteoarthritis Isabelle Boutron, MD; Florence Tubach, MD; Bruno Giraudeau, PhD; Philippe Ravaud, MD, PhD JAMA. 2003;290:1062-1070
- ↑ Methodological Issues in Trials of Acupuncture Kaptchuk et al. JAMA.2001; 285: 1015-1016.
- ↑ BBC Hypnosis 'doubles IVF success'