Hypomagnesemia: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 22: | Line 22: | ||
==References== | ==References== | ||
| Line 80: | Line 55: | ||
==External links== | ==External links== | ||
*[http://ods.od.nih.gov/factsheets/magnesium.asp Magnesium ] | *[http://ods.od.nih.gov/factsheets/magnesium.asp Magnesium ] | ||
*[http://www.ctds.info/5_13_magnesium.html Magnesium Deficiency] | *[http://www.ctds.info/5_13_magnesium.html Magnesium Deficiency] | ||
{{Endocrine, nutritional and metabolic pathology}} | {{Endocrine, nutritional and metabolic pathology}} | ||
Revision as of 18:02, 20 September 2012
| Hypomagnesemia | |
 | |
|---|---|
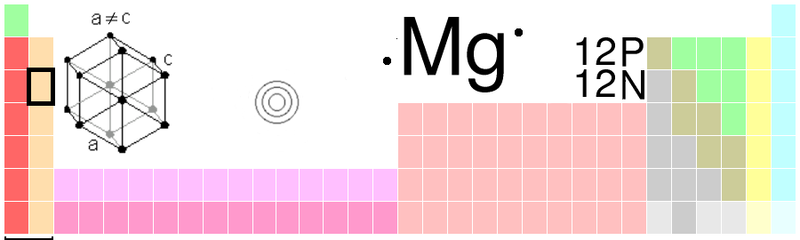
| Magnesium | |
| ICD-10 | E83.4 |
| ICD-9 | 275.2 |
| DiseasesDB | 6469 |
| MedlinePlus | 000315 |
|
Hypomagnesemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hypomagnesemia On the Web |
|
American Roentgen Ray Society Images of Hypomagnesemia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Hypomagnesaemia; magnesium levels low (plasma or serum)
References
- Cecil Textbook of Medicine
- Harrison's Principles of Internal Medicine
- Intensive Care Medicine by Irwin and Rippe
- The ICU Book by Marino
- The Oxford Textbook of Medicine
- Saeed M.G. Al-Ghamdi, Eugene C. Cameron, MD and Roger A.L. Sutton, "Magnesium Deficiency: Pathophysiology And Clinical Overview", American Journal Of Kidney Diseases, 1994; 24 (5), 737-752.
- Delhumeau, J.C. Granry, J.P. Monrigal, F. Costerousse, "Indications Du Magnésium En Anesthésie-Réanimation", Annales Francaises D'Anesthésie Et De Réanimation, 1995; 14, 406-416.
- J. Durlach, V. Durlach, P. Bac, M. Bara and A. Gulet-Bara, "Magnesium And Therapeutics", Magnesium Research 1994; 7 (3-4), 313-328.
- Mark D. Faber, Warren L. Kupin, Charles W. Heilig and Robert G. Narins, "Common Fluid-Electrolyte and Acid-Base Problems In The Intensive Care Unit: Selected Issues", Seminars In Nephrology 1994; 14 (1), 8-22.
- Lee Goldman, J. Claude Bennett, Cecil's Textbook of Medicine, 21st Edition, 2000, 1137-1139.
- Paul L. Marino, The ICU Book, Second Edition 1998, Chapter 42, 660-672.
- A.E. Meinders, Professor of Internal Medicine at Leids Universitair Medisch Centrum, "Magnesium", Bij Intensive Care Patiënten
- R. Mills, M. Leadbeater and A. Ravalia, "Case Report: Intravenous Magnesium Sulphate In The Management Of Refractory Bronchospasm In A Ventilated Asthmatic", Anaesthesia, 1997; 52, 782-785.
- Michael A. Olerich, MD; Robert K. Rude, MD, "Should We Supplement Magnesium In Critically Ill Patients?", New Horizons, 1994; 2 (2),186-192.
- James G. Ramsay, MD, "Cardiac Management In The ICU", Chest, 1999; 115: 138S-144S.
- Richard A. Reinhart, MD, "Magnesium Deficiency: Recognition And Treatment In The Emergency Medicine Setting", American Journal Of Emergency Medicine, 1992; 10 (1), 76-83.
- Richard A. Reinhart, MD; Norman A. Desbiens, MD, "Hypomagnesemia In Patients Entering The ICU", Critical Care Medicine, 1985; 13 (6), 506-507.
- Elisabeth Ryzen, MD; Park W. Wagers, MD; Frederick R. Singer, MD; Robert K. Rude, MD, "Magnesium Deficiency In A Medical ICU Population", Critical Care Medicine, 1985; 13 (1), 19-21.
- Elisabeth Ryzen, MD, "Magnesium Homeostasis In Critically Ill Patients", Magnesium, 1998; 8, 201-212.
- Robert Whang, Edward M. Hampton and David D. Whang, "Magnesium Homeostasis And Clinical Disorders Of Magnesium Deficiency", The Annals Of Pharmacotherapy, 1994; 28, 220-226.
- Selenium deficiency as a cause of overload of iron and unbalanced distribution of other minerals