Hydroxychloroquine: Difference between revisions
m (Protected "Hydroxychloroquine": Protecting pages from unwanted edits ([edit=sysop] (indefinite) [move=sysop] (indefinite))) |
No edit summary |
||
| Line 1: | Line 1: | ||
{{ | {{DrugProjectFormSinglePage | ||
| | |authorTag= | ||
{{VP}} | |||
<!--Overview--> | |||
= | |genericName= | ||
Hydroxychloroquine | |||
= | |aOrAn= | ||
a | |||
|drugClass= | |||
|indication= | |||
acute attacks of malaria due to Plasmodium vivax, P. malariae, P. ovale and susceptible strains of P. falciparum, discoid and systemic lupus erythematosus, and rheumatoid arthritis. | |||
|hasBlackBoxWarning= | |||
Yes | |||
|adverseReactions= | |||
[[ | |||
{{ | |||
<!--Black Box Warning--> | |||
|blackBoxWarningTitle= | |||
FAMILIARIZE WITH LEAFLET | |||
|blackBoxWarningBody= | |||
<i><span style="color:#FF0000;">ConditionName: </span></i> | |||
*PHYSICIANS SHOULD COMPLETELY FAMILIARIZE THEMSELVES WITH THE COMPLETE CONTENTS OF THIS LEAFLET BEFORE PRESCRIBING HYDROXYCHLOROQUINE. | |||
<!--Adult Indications and Dosage--> | |||
<!--FDA-Labeled Indications and Dosage (Adult)--> | |||
|fdaLIADAdult= | |||
=====Malaria===== | |||
* Dosing Information | |||
:*One tablet of 200 mg of Hydroxychloroquine Sulfate is equivalent to 155 mg base. | |||
:*Malaria: Suppression–In adults, 400 mg (=310 mg base) on exactly the same day of each week. In infants and children, the weekly suppressive dosage is 5 mg, calculated as base, per kg of body weight, but should not exceed the adult dose regardless of weight. | |||
:*If circumstances permit, suppressive therapy should begin two weeks prior to exposure. However, failing this, in adults an initial double (loading) dose of 800 mg (=620 mg base), or in children 10 mg base/kg may be taken in two divided doses, six hours apart. The suppressive therapy should be continued for eight weeks after leaving the endemic area. | |||
:*Treatment of the acute attack–In adults, an initial dose of 800 mg (=620 mg base) followed by 400 mg (=310 mg base) in six to eight hours and 400 mg (=310 mg base) on each of two consecutive days (total 2 g hydroxychloroquine sulfate or 1.55 g base). An alternative method, employing a single dose of 800 mg (=620 mg base), has also proved effective. | |||
:*The dosage for adults may also be calculated on the basis of body weight; this method is preferred for infants and children. A total dose representing 25 mg of base per kg of body weight is administered in three days as follows: | |||
:*First dose: 10 mg base per kg (but not exceeding a single dose of 620 mg base). | |||
:*Second dose: 5 mg base per kg (but not exceeding a single dose of 310 mg base) 6 hours after first dose. | |||
:*Third dose: 5 mg base per kg 18 hours after second dose. | |||
:*Fourth dose: 5 mg base per kg 24 hours after third dose. | |||
:*For radical cure of vivax and malariae malaria concomitant therapy with an 8-aminoquinoline compound is necessary. | |||
=====Systemic Lupus Erythematosus===== | |||
* Dosing Information | |||
:*Initially, the average adult dose is 400 mg (=310 mg base) once or twice daily. This may be continued for several weeks or months, depending on the response of the patient. For prolonged maintenance therapy, a smaller dose, from 200 mg to 400 mg (=155 mg to 310 mg base) daily will frequently suffice. | |||
=====Rheumatoid Arthritis===== | |||
* Dosing Information | |||
:*Initial dosage–In adults from 400 mg to 600 mg (=310 mg to 465 mg base) daily, each dose to be taken with a meal or a glass of milk. In a small percentage of patients, troublesome side effects may require temporary reduction of the initial dosage. Later (usually from five to ten days), the dose may gradually be increased to the optimum response level, often without return of side effects. | |||
:*Maintenance dosage–When a good response is obtained (usually in four to twelve weeks), the dosage is reduced by 50 percent and continued at a usual maintenance level of 200 mg to 400 mg (=155 mg to 310 mg base) daily, each dose to be taken with a meal or a glass of milk. The incidence of retinopathy has been reported to be higher when this maintenance dose is exceeded. | |||
:*Should a relapse occur after medication is withdrawn, therapy may be resumed or continued on an intermittent schedule if there are no ocular contraindications. | |||
:*Corticosteroids and salicylates may be used in conjunction with this compound, and they can generally be decreased gradually in dosage or eliminated after the drug has been used for several weeks. When gradual reduction of steroid dosage is indicated, it may be done by reducing every four to five days the dose of cortisone by no more than from 5 mg to 15 mg; of hydrocortisone from 5 mg to 10 mg; of prednisolone and prednisone from 1 mg to 2.5 mg; of methylprednisolone and triamcinolone from 1 mg to 2 mg; and of dexamethasone from 0.25 mg to 0.5 mg. | |||
<!--Off-Label Use and Dosage (Adult)--> | |||
<!--Guideline-Supported Use (Adult)--> | |||
|offLabelAdultGuideSupport= | |||
=====Condition1===== | |||
* Developed by: | |||
* Class of Recommendation: | |||
* Strength of Evidence: | |||
* Dosing Information | |||
:* Dosage | |||
=====Condition2===== | |||
There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | |||
<!--Non–Guideline-Supported Use (Adult)--> | |||
|offLabelAdultNoGuideSupport= | |||
=====Condition1===== | |||
* Dosing Information | |||
:* Dosage | |||
=====Condition2===== | |||
There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | |||
<!--Pediatric Indications and Dosage--> | |||
<!--FDA-Labeled Indications and Dosage (Pediatric)--> | |||
|fdaLIADPed= | |||
=====Condition1===== | |||
* Dosing Information | |||
:* Dosage | |||
=====Condition2===== | |||
There is limited information regarding <i>FDA-Labeled Use</i> of {{PAGENAME}} in pediatric patients. | |||
<!--Off-Label Use and Dosage (Pediatric)--> | |||
<!--Guideline-Supported Use (Pediatric)--> | |||
|offLabelPedGuideSupport= | |||
=====Condition1===== | |||
* Developed by: | |||
* Class of Recommendation: | |||
* Strength of Evidence: | |||
* Dosing Information | |||
:* Dosage | |||
=====Condition2===== | |||
There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | |||
<!--Non–Guideline-Supported Use (Pediatric)--> | |||
|offLabelPedNoGuideSupport= | |||
=====Condition1===== | |||
* Dosing Information | |||
:* Dosage | |||
=====Condition2===== | |||
There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | |||
<!--Contraindications--> | |||
|contraindications= | |||
*Use of this drug is contraindicated (1) in the presence of retinal or visual field changes attributable to any 4-aminoquinoline compound, (2) in patients with known hypersensitivity to 4-aminoquinoline compounds, and (3) for long-term therapy in children. | |||
<!--Warnings--> | |||
|warnings= | |||
*General - Hydroxychloroquine sulfate is not effective against chloroquine-resistant strains of P. falciparum. | |||
*Children are especially sensitive to the 4-aminoquinoline compounds. A number of fatalities have been reported following the accidental ingestion of chloroquine, sometimes in relatively small doses (0.75 g or 1 g in one 3-year-old child). Patients should be strongly warned to keep these drugs out of the reach of children. | |||
*Use of hydroxychloroquine sulfate in patients with psoriasis may precipitate a severe attack of psoriasis. When used in patients with porphyria the condition may be exacerbated. The preparation should not be used in these conditions unless in the judgement of the physician the benefit to the patient outweighs the possible hazard. | |||
*Usage in Pregnancy - Usage of this drug during pregnancy should be avoided except in the suppression or treatment of malaria when in the judgement of the physician the benefit outweighs the possible hazard. It should be noted that radioactively-tagged chloroquine administered intravenously to pregnant, pigmented, CBA mice passed rapidly across the placenta. It accumulated selectively in the melanin structures of the fetal eyes and was retained in the ocular tissues for five months after the drug had been eliminated from the rest of the body. | |||
====Precautions==== | |||
* General - Antimalarial compounds should be used with caution in patients with hepatic disease or alcoholism or in conjunction with known hepatotoxic drugs. | |||
*Periodic blood cell counts should be made if patients are given prolonged therapy. If any severe blood disorder appears which is not attributable to the disease under treatment, discontinuation of the drug should be considered. The drug should be administered with caution in patients having G-6-PD (glucose-6-phosphate dehydrogenase) deficiency. | |||
<!--Adverse Reactions--> | |||
<!--Clinical Trials Experience--> | |||
|clinicalTrials= | |||
*Following the administration in doses adequate for the treatment of an acute malarial attack, mild and transient headache, dizziness, and gastrointestinal complaints (diarrhea, anorexia, nausea, abdominal cramps and, on rare occasions, vomiting) may occur. Cardiomyopathy has been rarely reported with high daily dosages of hydroxychloroquine. | |||
*Not all of the following reactions have been observed with every 4-aminoquinoline compound during long-term therapy, but they have been reported with one or more and should be borne in mind when drugs of this class are administered. Adverse effects with different compounds vary in type and frequency. | |||
=====CNS Reactions===== | |||
Irritability, nervousness, emotional changes, nightmares, psychosis, headache, dizziness, vertigo, tinnitus, nystagmus, nerve deafness, convulsions, ataxia. | |||
=====Neuromuscular Reactions===== | |||
Skeletal muscle palsies or skeletal muscle myopathy or neuromyopathy leading to progressive weakness and atrophy of proximal muscle groups which may be associated with mild sensory changes, depression of tendon reflexes and abnormal nerve conduction. | |||
=====Ocular Reactions===== | |||
*Ciliary body: Disturbance of accommodation with symptoms of blurred vision. This reaction is dose related and reversible with cessation of therapy. | |||
*Cornea: Transient edema, punctate to lineal opacities, decreased corneal sensitivity. The corneal changes, with or without accompanying symptoms (blurred vision, halos around lights, photophobia), are fairly common, but reversible. Corneal deposits may appear as early as three weeks following initiation of therapy. | |||
*The incidence of corneal changes and visual side effects appears to be considerably lower with hydroxychloroquine than with chloroquine. | |||
*Retina: Macula: Edema, atrophy, abnormal pigmentation (mild pigment stippling to a “bulls-eye” appearance), loss of foveal reflex, increased macular recovery time following exposure to a bright light (photo-stress test), elevated retinal threshold to red light in macular, paramacular and peripheral retinal areas. | |||
*Other fundus changes include optic disc pallor and atrophy, attenuation of retinal arterioles, fine granular pigmentary disturbances in the peripheral retina and prominent choroidal patterns in advanced stage. | |||
*Visual field defects: Pericentral or paracentral scotoma, central scotoma with decreased visual acuity, rarely field constriction. | |||
*The most common visual symptoms attributed to the retinopathy are: reading and seeing difficulties (words, letters, or parts of objects missing), photophobia, blurred distance vision, missing or blacked out areas in the central or peripheral visual field, light flashes and streaks. | |||
*Retinopathy appears to be dose related and has occurred within several months (rarely) to several years of daily therapy; a small number of cases have been reported several years after antimalarial drug therapy was discontinued. It has not been noted during prolonged use of weekly doses of the 4-aminoquinoline compounds for suppression of malaria. | |||
*Patients with retinal changes may have visual symptoms or may be asymptomatic (with or without visual field changes). Rarely scotomatous vision field defects may occur without obvious retinal change. | |||
*Retinopathy may progress even after the drug is discontinued. In a number of patients, early retinopathy (macular pigmentation sometimes with central field defects) diminished or regressed completely after therapy was discontinued. Paracentral scotoma to red targets (sometimes called “premaculopathy”) is indicative of early retinal dysfunction which is usually reversible with cessation of therapy. | |||
*A small number of cases of retinal changes have been reported as occurring in patients who received only hydroxychloroquine. These usually consisted of alteration in retinal pigmentation which was detected on periodic ophthalmologic examination; visual field defects were also present in some instances. A case of delayed retinopathy has been reported with loss of vision starting one year after administration of hydroxychloroquine had been discontinued. | |||
=====Dermatologic Reactions===== | |||
Bleaching of hair, alopecia, pruritus, skin and mucosal pigmentation, photosensitivity, and skin eruptions (urticarial, morbilliform, Iichenoid, maculopapular, purpuric, erythema annulare centrifugum, Stevens-Johnson syndrome, acute generalized exanthematous pustulosis, and exfoliative dermatitis). | |||
=====Hematologic Reactions===== | |||
Various blood dyscrasias such as aplastic anemia, agranulocytosis, leukopenia, thrombocytopenia (hemolysis in individuals with glucose-6-phosphate dehydrogenase [G6-PD] deficiency). | |||
=====Gastrointestinal Reactions===== | |||
Anorexia, nausea, vomiting, diarrhea, and abdominal cramps. Isolated cases of abnormal liver function and fulminant hepatic failure. | |||
=====Miscellaneous Reactions===== | |||
Weight loss, lassitude, exacerbation or precipitation of porphyria and nonlight-sensitive psoriasis. | |||
*Cardiomyopathy has been rarely reported with high daily doses of hydroxychloroquine. | |||
<!--Postmarketing Experience--> | |||
|postmarketing= | |||
There is limited information regarding <i>Postmarketing Experience</i> of {{PAGENAME}} in the drug label. | |||
<!--Drug Interactions--> | |||
|drugInteractions= | |||
* Drug | |||
:* Description | |||
<!--Use in Specific Populations--> | |||
|useInPregnancyFDA= | |||
* '''Pregnancy Category''' | |||
|useInPregnancyAUS= | |||
* '''Australian Drug Evaluation Committee (ADEC) Pregnancy Category''' | |||
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | |||
|useInLaborDelivery= | |||
There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | |||
|useInNursing= | |||
There is no FDA guidance on the use of {{PAGENAME}} with respect to nursing mothers. | |||
|useInPed= | |||
There is no FDA guidance on the use of {{PAGENAME}} with respect to pediatric patients. | |||
|useInGeri= | |||
There is no FDA guidance on the use of {{PAGENAME}} with respect to geriatric patients. | |||
|useInGender= | |||
There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | |||
|useInRace= | |||
There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | |||
|useInRenalImpair= | |||
There is no FDA guidance on the use of {{PAGENAME}} in patients with renal impairment. | |||
|useInHepaticImpair= | |||
There is no FDA guidance on the use of {{PAGENAME}} in patients with hepatic impairment. | |||
|useInReproPotential= | |||
There is no FDA guidance on the use of {{PAGENAME}} in women of reproductive potentials and males. | |||
|useInImmunocomp= | |||
There is no FDA guidance one the use of {{PAGENAME}} in patients who are immunocompromised. | |||
<!--Administration and Monitoring--> | |||
|administration= | |||
* Oral | |||
|monitoring= | |||
There is limited information regarding <i>Monitoring</i> of {{PAGENAME}} in the drug label. | |||
<!--IV Compatibility--> | |||
|IVCompat= | |||
There is limited information regarding <i>IV Compatibility</i> of {{PAGENAME}} in the drug label. | |||
<!--Overdosage--> | |||
|overdose= | |||
===Acute Overdose=== | |||
====Signs and Symptoms==== | |||
*The 4-aminoquinoline compounds are very rapidly and completely absorbed after ingestion, and in accidental overdosage, or rarely with lower doses in hypersensitive patients, toxic symptoms may occur within 30 minutes. These consist of headache, drowsiness, visual disturbances, cardiovascular collapse, and convulsions, followed by sudden and early respiratory and cardiac arrest. The electrocardiogram may reveal atrial standstill, nodal rhythm, prolonged intraventricular conduction time, and progressive bradycardia leading to ventricular fibrillation and/or arrest. Treatment is symptomatic and must be prompt with immediate evacuation of the stomach by emesis (at home, before transportation to the hospital) or gastric lavage until the stomach is completely emptied. If finely powdered, activated charcoal is introduced by the stomach tube, after lavage, and within 30 minutes after ingestion of the tablets, it may inhibit further intestinal absorption of the drug. To be effective, the dose of activated charcoal should be at least five times the estimated dose of hydroxychloroquine ingested. Convulsions, if present, should be controlled before attempting gastric lavage. If due to cerebral stimulation, cautious administration of an ultrashort-acting barbiturate may be tried but, if due to anoxia, it should be corrected by oxygen administration, artificial respiration or, in shock with hypotension, by vasopressor therapy. Because of the importance of supporting respiration, tracheal intubation or tracheostomy, followed by gastric lavage, may also be necessary. Exchange transfusions have been used to reduce the level of 4-aminoquinoline drug in the blood. | |||
====Management==== | |||
*A patient who survives the acute phase and is asymptomatic should be closely observed for at least six hours. Fluids may be forced, and sufficient ammonium chloride (8 g daily in divided doses for adults) may be administered for a few days to acidify the urine to help promote urinary excretion in cases of both overdosage and sensitivity. | |||
===Chronic Overdose=== | |||
There is limited information regarding <i>Chronic Overdose</i> of {{PAGENAME}} in the drug label. | |||
<!--Pharmacology--> | |||
<!--Drug box 2--> | |||
|drugBox= | |||
<!--Mechanism of Action--> | |||
|mechAction= | |||
*The drug possesses antimalarial actions and also exerts a beneficial effect in lupus erythematosus (chronic discoid or systemic) and acute or chronic rheumatoid arthritis. The precise mechanism of action is not known. | |||
*Malaria | |||
:*Like chloroquine phosphate, hydroxychloroquine sulfate is highly active against the erythrocytic forms of P. vivax and malariae and most strains of P. falciparum (but not the gametocytes of P. falciparum). | |||
:(Hydroxychloroquine sulfate does not prevent relapses in patients with vivax or malariae malaria because it is not effective against exo-erythrocytic forms of the parasite, nor will it prevent vivax or malariae infection when administered as a prophylactic. It is highly effective as a suppressive agent in patients with vivax or malariae malaria, in terminating acute attacks, and significantly lengthening the interval between treatment and relapse. In patients with falciparum malaria, it abolishes the acute attack and effects complete cure of the infection, unless due to a resistant strain of P. falciparum. | |||
<!--Structure--> | |||
|structure= | |||
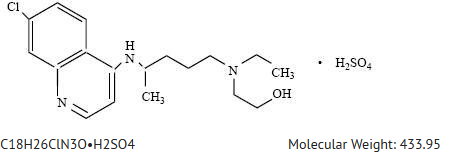
* Hydroxychloroquine sulfate is a colorless crystalline solid, soluble in water to at least 20 percent; chemically the drug is (±)-2-[[4-[(7-Chloro-4-quinolyl)amino]pentyl]-ethylamino]ethanol sulfate (1:1) (salt). It has the following structural formula: | |||
: [[File:{{PAGENAME}}01.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
*Each tablet, for oral administration, contains 200 mg of hydroxychloroquine sulfate. In addition, each tablet contains the following inactive ingredients: colloidal silicon dioxide, dextrates, hypromellose, magnesium stearate, maltodextrin, microcrystalline cellulose, polydextrose, polyethylene glycol, sodium starch glycolate, starch (corn), titanium dioxide, and triacetin. | |||
<!--Pharmacodynamics--> | |||
|PD= | |||
There is limited information regarding <i>Pharmacodynamics</i> of {{PAGENAME}} in the drug label. | |||
<!--Pharmacokinetics--> | |||
|PK= | |||
There is limited information regarding <i>Pharmacokinetics</i> of {{PAGENAME}} in the drug label. | |||
<!--Nonclinical Toxicology--> | |||
|nonClinToxic= | |||
There is limited information regarding <i>Nonclinical Toxicology</i> of {{PAGENAME}} in the drug label. | |||
<!--Clinical Studies--> | |||
|clinicalStudies= | |||
There is limited information regarding <i>Clinical Studies</i> of {{PAGENAME}} in the drug label. | |||
<!--How Supplied--> | |||
|howSupplied= | |||
* | |||
<!--Patient Counseling Information--> | |||
|fdaPatientInfo= | |||
There is limited information regarding <i>Patient Counseling Information</i> of {{PAGENAME}} in the drug label. | |||
<!--Precautions with Alcohol--> | |||
|alcohol= | |||
* Alcohol-{{PAGENAME}} interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |||
<!--Brand Names--> | |||
|brandNames= | |||
* ®<ref>{{Cite web | title = | url = }}</ref> | |||
<!--Look-Alike Drug Names--> | |||
|lookAlike= | |||
* A® — B®<ref name="www.ismp.org">{{Cite web | last = | first = | title = http://www.ismp.org | url = http://www.ismp.org | publisher = | date = }}</ref> | |||
<!--Drug Shortage Status--> | |||
|drugShortage= | |||
}} | |||
<!--Pill Image--> | |||
{{PillImage | |||
|fileName=No image.jpg|This image is provided by the National Library of Medicine. | |||
|drugName= | |||
|NDC= | |||
|drugAuthor= | |||
|ingredients= | |||
|pillImprint= | |||
|dosageValue= | |||
|dosageUnit= | |||
|pillColor= | |||
|pillShape= | |||
|pillSize= | |||
|pillScore= | |||
}} | |||
<!--Label Display Image--> | |||
{{LabelImage | |||
|fileName={{PAGENAME}}11.png|This image is provided by the National Library of Medicine. | |||
}} | |||
{{LabelImage | |||
|fileName={{PAGENAME}}11.png|This image is provided by the National Library of Medicine. | |||
}} | |||
<!--Category--> | |||
[[Category:Drug]] | |||
Revision as of 14:10, 15 October 2014
{{DrugProjectFormSinglePage |authorTag=
Vignesh Ponnusamy, M.B.B.S. [1]
|genericName=
Hydroxychloroquine
|aOrAn=
a
|drugClass=
|indication=
acute attacks of malaria due to Plasmodium vivax, P. malariae, P. ovale and susceptible strains of P. falciparum, discoid and systemic lupus erythematosus, and rheumatoid arthritis.
|hasBlackBoxWarning=
Yes
|adverseReactions=
|blackBoxWarningTitle=
FAMILIARIZE WITH LEAFLET
|blackBoxWarningBody= ConditionName:
- PHYSICIANS SHOULD COMPLETELY FAMILIARIZE THEMSELVES WITH THE COMPLETE CONTENTS OF THIS LEAFLET BEFORE PRESCRIBING HYDROXYCHLOROQUINE.
|fdaLIADAdult=
Malaria
- Dosing Information
- One tablet of 200 mg of Hydroxychloroquine Sulfate is equivalent to 155 mg base.
- Malaria: Suppression–In adults, 400 mg (=310 mg base) on exactly the same day of each week. In infants and children, the weekly suppressive dosage is 5 mg, calculated as base, per kg of body weight, but should not exceed the adult dose regardless of weight.
- If circumstances permit, suppressive therapy should begin two weeks prior to exposure. However, failing this, in adults an initial double (loading) dose of 800 mg (=620 mg base), or in children 10 mg base/kg may be taken in two divided doses, six hours apart. The suppressive therapy should be continued for eight weeks after leaving the endemic area.
- Treatment of the acute attack–In adults, an initial dose of 800 mg (=620 mg base) followed by 400 mg (=310 mg base) in six to eight hours and 400 mg (=310 mg base) on each of two consecutive days (total 2 g hydroxychloroquine sulfate or 1.55 g base). An alternative method, employing a single dose of 800 mg (=620 mg base), has also proved effective.
- The dosage for adults may also be calculated on the basis of body weight; this method is preferred for infants and children. A total dose representing 25 mg of base per kg of body weight is administered in three days as follows:
- First dose: 10 mg base per kg (but not exceeding a single dose of 620 mg base).
- Second dose: 5 mg base per kg (but not exceeding a single dose of 310 mg base) 6 hours after first dose.
- Third dose: 5 mg base per kg 18 hours after second dose.
- Fourth dose: 5 mg base per kg 24 hours after third dose.
- For radical cure of vivax and malariae malaria concomitant therapy with an 8-aminoquinoline compound is necessary.
Systemic Lupus Erythematosus
- Dosing Information
- Initially, the average adult dose is 400 mg (=310 mg base) once or twice daily. This may be continued for several weeks or months, depending on the response of the patient. For prolonged maintenance therapy, a smaller dose, from 200 mg to 400 mg (=155 mg to 310 mg base) daily will frequently suffice.
Rheumatoid Arthritis
- Dosing Information
- Initial dosage–In adults from 400 mg to 600 mg (=310 mg to 465 mg base) daily, each dose to be taken with a meal or a glass of milk. In a small percentage of patients, troublesome side effects may require temporary reduction of the initial dosage. Later (usually from five to ten days), the dose may gradually be increased to the optimum response level, often without return of side effects.
- Maintenance dosage–When a good response is obtained (usually in four to twelve weeks), the dosage is reduced by 50 percent and continued at a usual maintenance level of 200 mg to 400 mg (=155 mg to 310 mg base) daily, each dose to be taken with a meal or a glass of milk. The incidence of retinopathy has been reported to be higher when this maintenance dose is exceeded.
- Should a relapse occur after medication is withdrawn, therapy may be resumed or continued on an intermittent schedule if there are no ocular contraindications.
- Corticosteroids and salicylates may be used in conjunction with this compound, and they can generally be decreased gradually in dosage or eliminated after the drug has been used for several weeks. When gradual reduction of steroid dosage is indicated, it may be done by reducing every four to five days the dose of cortisone by no more than from 5 mg to 15 mg; of hydrocortisone from 5 mg to 10 mg; of prednisolone and prednisone from 1 mg to 2.5 mg; of methylprednisolone and triamcinolone from 1 mg to 2 mg; and of dexamethasone from 0.25 mg to 0.5 mg.
|offLabelAdultGuideSupport=
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Hydroxychloroquine in adult patients.
|offLabelAdultNoGuideSupport=
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Hydroxychloroquine in adult patients.
|fdaLIADPed=
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding FDA-Labeled Use of Hydroxychloroquine in pediatric patients.
|offLabelPedGuideSupport=
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Hydroxychloroquine in pediatric patients.
|offLabelPedNoGuideSupport=
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Hydroxychloroquine in pediatric patients.
|contraindications=
- Use of this drug is contraindicated (1) in the presence of retinal or visual field changes attributable to any 4-aminoquinoline compound, (2) in patients with known hypersensitivity to 4-aminoquinoline compounds, and (3) for long-term therapy in children.
|warnings=
- General - Hydroxychloroquine sulfate is not effective against chloroquine-resistant strains of P. falciparum.
- Children are especially sensitive to the 4-aminoquinoline compounds. A number of fatalities have been reported following the accidental ingestion of chloroquine, sometimes in relatively small doses (0.75 g or 1 g in one 3-year-old child). Patients should be strongly warned to keep these drugs out of the reach of children.
- Use of hydroxychloroquine sulfate in patients with psoriasis may precipitate a severe attack of psoriasis. When used in patients with porphyria the condition may be exacerbated. The preparation should not be used in these conditions unless in the judgement of the physician the benefit to the patient outweighs the possible hazard.
- Usage in Pregnancy - Usage of this drug during pregnancy should be avoided except in the suppression or treatment of malaria when in the judgement of the physician the benefit outweighs the possible hazard. It should be noted that radioactively-tagged chloroquine administered intravenously to pregnant, pigmented, CBA mice passed rapidly across the placenta. It accumulated selectively in the melanin structures of the fetal eyes and was retained in the ocular tissues for five months after the drug had been eliminated from the rest of the body.
Precautions
- General - Antimalarial compounds should be used with caution in patients with hepatic disease or alcoholism or in conjunction with known hepatotoxic drugs.
- Periodic blood cell counts should be made if patients are given prolonged therapy. If any severe blood disorder appears which is not attributable to the disease under treatment, discontinuation of the drug should be considered. The drug should be administered with caution in patients having G-6-PD (glucose-6-phosphate dehydrogenase) deficiency.
|clinicalTrials=
- Following the administration in doses adequate for the treatment of an acute malarial attack, mild and transient headache, dizziness, and gastrointestinal complaints (diarrhea, anorexia, nausea, abdominal cramps and, on rare occasions, vomiting) may occur. Cardiomyopathy has been rarely reported with high daily dosages of hydroxychloroquine.
- Not all of the following reactions have been observed with every 4-aminoquinoline compound during long-term therapy, but they have been reported with one or more and should be borne in mind when drugs of this class are administered. Adverse effects with different compounds vary in type and frequency.
CNS Reactions
Irritability, nervousness, emotional changes, nightmares, psychosis, headache, dizziness, vertigo, tinnitus, nystagmus, nerve deafness, convulsions, ataxia.
Neuromuscular Reactions
Skeletal muscle palsies or skeletal muscle myopathy or neuromyopathy leading to progressive weakness and atrophy of proximal muscle groups which may be associated with mild sensory changes, depression of tendon reflexes and abnormal nerve conduction.
Ocular Reactions
- Ciliary body: Disturbance of accommodation with symptoms of blurred vision. This reaction is dose related and reversible with cessation of therapy.
- Cornea: Transient edema, punctate to lineal opacities, decreased corneal sensitivity. The corneal changes, with or without accompanying symptoms (blurred vision, halos around lights, photophobia), are fairly common, but reversible. Corneal deposits may appear as early as three weeks following initiation of therapy.
- The incidence of corneal changes and visual side effects appears to be considerably lower with hydroxychloroquine than with chloroquine.
- Retina: Macula: Edema, atrophy, abnormal pigmentation (mild pigment stippling to a “bulls-eye” appearance), loss of foveal reflex, increased macular recovery time following exposure to a bright light (photo-stress test), elevated retinal threshold to red light in macular, paramacular and peripheral retinal areas.
- Other fundus changes include optic disc pallor and atrophy, attenuation of retinal arterioles, fine granular pigmentary disturbances in the peripheral retina and prominent choroidal patterns in advanced stage.
- Visual field defects: Pericentral or paracentral scotoma, central scotoma with decreased visual acuity, rarely field constriction.
- The most common visual symptoms attributed to the retinopathy are: reading and seeing difficulties (words, letters, or parts of objects missing), photophobia, blurred distance vision, missing or blacked out areas in the central or peripheral visual field, light flashes and streaks.
- Retinopathy appears to be dose related and has occurred within several months (rarely) to several years of daily therapy; a small number of cases have been reported several years after antimalarial drug therapy was discontinued. It has not been noted during prolonged use of weekly doses of the 4-aminoquinoline compounds for suppression of malaria.
- Patients with retinal changes may have visual symptoms or may be asymptomatic (with or without visual field changes). Rarely scotomatous vision field defects may occur without obvious retinal change.
- Retinopathy may progress even after the drug is discontinued. In a number of patients, early retinopathy (macular pigmentation sometimes with central field defects) diminished or regressed completely after therapy was discontinued. Paracentral scotoma to red targets (sometimes called “premaculopathy”) is indicative of early retinal dysfunction which is usually reversible with cessation of therapy.
- A small number of cases of retinal changes have been reported as occurring in patients who received only hydroxychloroquine. These usually consisted of alteration in retinal pigmentation which was detected on periodic ophthalmologic examination; visual field defects were also present in some instances. A case of delayed retinopathy has been reported with loss of vision starting one year after administration of hydroxychloroquine had been discontinued.
Dermatologic Reactions
Bleaching of hair, alopecia, pruritus, skin and mucosal pigmentation, photosensitivity, and skin eruptions (urticarial, morbilliform, Iichenoid, maculopapular, purpuric, erythema annulare centrifugum, Stevens-Johnson syndrome, acute generalized exanthematous pustulosis, and exfoliative dermatitis).
Hematologic Reactions
Various blood dyscrasias such as aplastic anemia, agranulocytosis, leukopenia, thrombocytopenia (hemolysis in individuals with glucose-6-phosphate dehydrogenase [G6-PD] deficiency).
Gastrointestinal Reactions
Anorexia, nausea, vomiting, diarrhea, and abdominal cramps. Isolated cases of abnormal liver function and fulminant hepatic failure.
Miscellaneous Reactions
Weight loss, lassitude, exacerbation or precipitation of porphyria and nonlight-sensitive psoriasis.
- Cardiomyopathy has been rarely reported with high daily doses of hydroxychloroquine.
|postmarketing=
There is limited information regarding Postmarketing Experience of Hydroxychloroquine in the drug label.
|drugInteractions=
- Drug
- Description
|useInPregnancyFDA=
- Pregnancy Category
|useInPregnancyAUS=
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Hydroxychloroquine in women who are pregnant.
|useInLaborDelivery= There is no FDA guidance on use of Hydroxychloroquine during labor and delivery.
|useInNursing= There is no FDA guidance on the use of Hydroxychloroquine with respect to nursing mothers.
|useInPed= There is no FDA guidance on the use of Hydroxychloroquine with respect to pediatric patients.
|useInGeri= There is no FDA guidance on the use of Hydroxychloroquine with respect to geriatric patients.
|useInGender= There is no FDA guidance on the use of Hydroxychloroquine with respect to specific gender populations.
|useInRace= There is no FDA guidance on the use of Hydroxychloroquine with respect to specific racial populations.
|useInRenalImpair= There is no FDA guidance on the use of Hydroxychloroquine in patients with renal impairment.
|useInHepaticImpair= There is no FDA guidance on the use of Hydroxychloroquine in patients with hepatic impairment.
|useInReproPotential= There is no FDA guidance on the use of Hydroxychloroquine in women of reproductive potentials and males.
|useInImmunocomp= There is no FDA guidance one the use of Hydroxychloroquine in patients who are immunocompromised.
|administration=
- Oral
|monitoring=
There is limited information regarding Monitoring of Hydroxychloroquine in the drug label.
|IVCompat=
There is limited information regarding IV Compatibility of Hydroxychloroquine in the drug label.
|overdose=
Acute Overdose
Signs and Symptoms
- The 4-aminoquinoline compounds are very rapidly and completely absorbed after ingestion, and in accidental overdosage, or rarely with lower doses in hypersensitive patients, toxic symptoms may occur within 30 minutes. These consist of headache, drowsiness, visual disturbances, cardiovascular collapse, and convulsions, followed by sudden and early respiratory and cardiac arrest. The electrocardiogram may reveal atrial standstill, nodal rhythm, prolonged intraventricular conduction time, and progressive bradycardia leading to ventricular fibrillation and/or arrest. Treatment is symptomatic and must be prompt with immediate evacuation of the stomach by emesis (at home, before transportation to the hospital) or gastric lavage until the stomach is completely emptied. If finely powdered, activated charcoal is introduced by the stomach tube, after lavage, and within 30 minutes after ingestion of the tablets, it may inhibit further intestinal absorption of the drug. To be effective, the dose of activated charcoal should be at least five times the estimated dose of hydroxychloroquine ingested. Convulsions, if present, should be controlled before attempting gastric lavage. If due to cerebral stimulation, cautious administration of an ultrashort-acting barbiturate may be tried but, if due to anoxia, it should be corrected by oxygen administration, artificial respiration or, in shock with hypotension, by vasopressor therapy. Because of the importance of supporting respiration, tracheal intubation or tracheostomy, followed by gastric lavage, may also be necessary. Exchange transfusions have been used to reduce the level of 4-aminoquinoline drug in the blood.
Management
- A patient who survives the acute phase and is asymptomatic should be closely observed for at least six hours. Fluids may be forced, and sufficient ammonium chloride (8 g daily in divided doses for adults) may be administered for a few days to acidify the urine to help promote urinary excretion in cases of both overdosage and sensitivity.
Chronic Overdose
There is limited information regarding Chronic Overdose of Hydroxychloroquine in the drug label.
|drugBox=
|mechAction=
- The drug possesses antimalarial actions and also exerts a beneficial effect in lupus erythematosus (chronic discoid or systemic) and acute or chronic rheumatoid arthritis. The precise mechanism of action is not known.
- Malaria
- Like chloroquine phosphate, hydroxychloroquine sulfate is highly active against the erythrocytic forms of P. vivax and malariae and most strains of P. falciparum (but not the gametocytes of P. falciparum).
- (Hydroxychloroquine sulfate does not prevent relapses in patients with vivax or malariae malaria because it is not effective against exo-erythrocytic forms of the parasite, nor will it prevent vivax or malariae infection when administered as a prophylactic. It is highly effective as a suppressive agent in patients with vivax or malariae malaria, in terminating acute attacks, and significantly lengthening the interval between treatment and relapse. In patients with falciparum malaria, it abolishes the acute attack and effects complete cure of the infection, unless due to a resistant strain of P. falciparum.
|structure=
- Hydroxychloroquine sulfate is a colorless crystalline solid, soluble in water to at least 20 percent; chemically the drug is (±)-2-[[4-[(7-Chloro-4-quinolyl)amino]pentyl]-ethylamino]ethanol sulfate (1:1) (salt). It has the following structural formula:
- Each tablet, for oral administration, contains 200 mg of hydroxychloroquine sulfate. In addition, each tablet contains the following inactive ingredients: colloidal silicon dioxide, dextrates, hypromellose, magnesium stearate, maltodextrin, microcrystalline cellulose, polydextrose, polyethylene glycol, sodium starch glycolate, starch (corn), titanium dioxide, and triacetin.
|PD=
There is limited information regarding Pharmacodynamics of Hydroxychloroquine in the drug label.
|PK=
There is limited information regarding Pharmacokinetics of Hydroxychloroquine in the drug label.
|nonClinToxic=
There is limited information regarding Nonclinical Toxicology of Hydroxychloroquine in the drug label.
|clinicalStudies=
There is limited information regarding Clinical Studies of Hydroxychloroquine in the drug label.
|howSupplied=
|fdaPatientInfo=
There is limited information regarding Patient Counseling Information of Hydroxychloroquine in the drug label.
|alcohol=
- Alcohol-Hydroxychloroquine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
|brandNames=
- ®[1]
|lookAlike=
- A® — B®[2]
|drugShortage=
}}
{{#subobject:
|Page Name=Hydroxychloroquine |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Hydroxychloroquine |Label Name=Hydroxychloroquine11.png
}}
{{#subobject:
|Label Page=Hydroxychloroquine |Label Name=Hydroxychloroquine11.png
}}
- ↑ Empty citation (help)
- ↑ "http://www.ismp.org". External link in
|title=(help)