Human serum albumin
| Albumin | |||
|---|---|---|---|
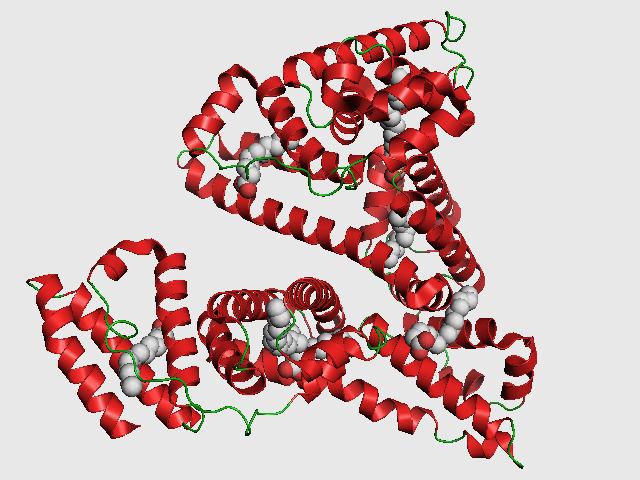 PDB rendering based on 1e7h. | |||
| Identifiers | |||
| Symbols | ALB ; DKFZp779N1935; PRO0883; PRO0903; PRO1341 | ||
| External IDs | Template:OMIM5 Template:MGI HomoloGene: 405 | ||
| RNA expression pattern | |||
 | |||
| More reference expression data | |||
| Orthologs | |||
| Template:GNF Ortholog box | |||
| Species | Human | Mouse | |
| Entrez | n/a | n/a | |
| Ensembl | n/a | n/a | |
| UniProt | n/a | n/a | |
| RefSeq (mRNA) | n/a | n/a | |
| RefSeq (protein) | n/a | n/a | |
| Location (UCSC) | n/a | n/a | |
| PubMed search | n/a | n/a | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Human serum albumin is the most abundant protein in human blood plasma. It is produced in the liver. Albumin comprises about half of the blood serum protein. It is soluble and monomeric.
The gene for albumin is located on chromosome 4 and mutations in this gene can result in various anomalous proteins. The human albumin gene is 16,961 nucleotides long from the putative 'cap' site to the first poly(A) addition site. It is split into 15 exons which are symmetrically placed within the 3 domains that are thought to have arisen by triplication of a single primordial domain.
Albumin is synthesized in the liver as preproalbumin which has an N-terminal peptide that is removed before the nascent protein is released from the rough endoplasmic reticulum. The product, proalbumin, is in turn cleaved in the Golgi vesicles to produce the secreted albumin.
The reference range for albumin concentrations in blood is 30 to 50 g/L. It has a serum half-life of approximately 20 days. It has a molecular mass of 67 kDa.
Functions of albumin
- Maintains oncotic pressure
- Transports thyroid hormones
- Transports other hormones, particularly fat soluble ones
- Transports fatty acids ("free" fatty acids) to the liver
- Transports unconjugated bilirubin
- Transports many drugs, and serum albumin levels can affect the half-life of drugs.
- Competitively binds calcium ions (Ca2+)
- Buffers pH
Pathology
Hypoalbuminemia
Low blood albumin levels (hypoalbuminemia) can be caused by:
- liver disease / Cirrhosis of the liver (most commonly)
- Decreased production (as in starvation/malnutrition/malabsorption)
- Excess excretion by the kidneys (as in nephrotic syndrome)
- Excess loss in bowel (protein losing enteropathy e.g. Menetrier's disease)
- Burns (Plasma loss in the absence of skin barrier)
- Redistribution (hemodilution [as in Pregnancy], increased vascular permeability or decreased lymphatic clearance)
- Acute disease states (referred to as a negative acute phase protein)
- Mutation causing analbuminemia (very rare)
Hyperalbuminemia
Typically is a sign of severe dehydration.
Glycation (Glycosylation) of Serum Albumin
It has been known for a long time that human blood proteins like hemoglobin [1] and serum albumin [2][3] may undergo a slow non-enzymatic glycation, mainly by formation of a Schiff base between ε-amino groups of lysine (and sometimes arginine) residues and glucose molecules in blood (Millard reaction). This reaction can be inhibited in the presence of antioxidant agents [4]. Although this reaction may happen normally [5] , elevated glycoalbumin is observed in diabetes mellitus [6].
Glycation has the potential to alter the biological structure and function of the serum albumin protein [7][8][9][10]. Moreover, the glycation finally can result in the formation of Advanced Glycosylation End Products (AGE), which result in abnormal biological effects. Accumulation of AGEs leads to tissue damage via alteration of the structures and functions of tissue proteins, stimulation of cellular responses, through receptors specific for AGE-proteins, and via generation of reactive oxygen intermediates. AGEs also react with DNA, thus causing mutations and DNA transposition. Thermal processing of proteins and carbohydrates brings major changes in allergenicity. AGEs are antigenic and represent many of the important neoantigens found in cooked or stored foods [11]. They also interfere with the normal product of nitric oxide in cells [12].
Although there are several lysine and arginine residues in the serum albumin structure, very few of them can take part in the glycation reaction [13][14]. It is not clear exactly why only these residues are glycated in serum albumin [15].
Testing for albumin loss via the kidneys
In the healthy kidney, albumin's size and negative electric charge exclude it from excretion in the glomerulus. This is not always the case, as in some diseases including diabetic nephropathy, a major complication of uncontrolled diabetes where proteins can cross the glomerulus. The lost albumin can be detected by a simple urine test [2]. Depending on the amount of albumin lost, a patient may have normal renal function, microalbuminuria, or albuminuria.
Amino Acid Sequence
The approximate sequence of human serum albumin is:
MKWVTFISLL FLFSSAYSRG VFRRDAHKSE VAHRFKDLGE ENFKALVLIA FAQYLQQCPF EDHVKLVNEV TEFAKTCVAD ESAENCDKSL HTLFGDKLCT VATLRETYGE MADCCAKQEP ERNECFLQHK DDNPNLPRLV RPEVDVMCTA FHDNEETFLK KYLYEIARRH PYFYAPELLF FAKRYKAAFT ECCQAADKAA CLLPKLDELR DEGKASSAKQ RLKCASLQKF GERAFKAWAV ARLSQRFPKA EFAEVSKLVT DLTKVHTECC HGDLLECADD RADLAKYICE NQDSISSKLK ECCEKPLLEK SHCIAEVEND EMPADLPSLA ADFVESKDVC KNYAEAKDVF LGMFLYEYAR RHPDYSVVLL LRLAKTYETT LEKCCAAADP HECYAKVFDE FKPLVEEPQN LIKQNCELFE QLGEYKFQNA LLVRYTKKVP QVSTPTLVEV SRNLGKVGSK CCKHPEAKRM PCAEDYLSVV LNQLCVLHEK TPVSDRVTKC CTESLVNRRP CFSALEVDET YVPKEFNAET FTFHADICTL SEKERQIKKQ TALVELVKHK PKATKEQLKA VMDDFAAFVE KCCKADDKET CFAEEGKKLV AASQAALGL
Where the italicized first 24 amino acids are signal and propeptide portions not observed in the transcribed, translated and transported protein but present in the gene. There are 609 amino acids in this sequence with only 585 amino acids in the final product observed in the blood.
See also
References
- ↑ Rajbar S (1968). "An abnormal hemoglobin in red cells of diabetics". Clin Chim Acta. 22 (2): 296–8. PMID 5687098.
- ↑ Day J, Thorpe S, Baynes J (1979). "Nonenzymatically glucosylated albumin. In vitro preparation and isolation from normal human serum". J Biol Chem. 254 (3): 595–7. PMID 762083.
- ↑ Iberg N, Flückiger R (1986). "Nonenzymatic glycosylation of albumin in vivo. Identification of multiple glycosylated sites". J Biol Chem. 261 (29): 13542–5. PMID 3759977.
- ↑ Jakus V, Hrnciarová M, Cársky J, Krahulec B, Rietbrock N (1999). "Inhibition of nonenzymatic protein glycation and lipid peroxidation by drugs with antioxidant activity". Life Sci. 65 (18–19): 1991–3. PMID 10576452.
- ↑ Day J, Thorpe S, Baynes J (1979). "Nonenzymatically glucosylated albumin. In vitro preparation and isolation from normal human serum". J Biol Chem. 254 (3): 595–7. PMID 762083.
- ↑ Iberg N, Flückiger R (1986). "Nonenzymatic glycosylation of albumin in vivo. Identification of multiple glycosylated sites". J Biol Chem. 261 (29): 13542–5. PMID 3759977.
- ↑ Mohamadi-Nejad A, Moosavi-Movahedi A, Hakimelahi G, Sheibani N (2002). "Thermodynamic analysis of human serum albumin interactions with glucose: insights into the diabetic range of glucose concentration". Int J Biochem Cell Biol. 34 (9): 1115–24. PMID 12009306.
- ↑ Shaklai N, Garlick R, Bunn H (1984). "Nonenzymatic glycosylation of human serum albumin alters its conformation and function". J Biol Chem. 259 (6): 3812–7. PMID 6706980.
- ↑ Mendez D, Jensen R, McElroy L, Pena J, Esquerra R (2005). "The effect of non-enzymatic glycation on the unfolding of human serum albumin". Arch Biochem Biophys. 444 (2): 92–9. PMID 16309624.
- ↑ Mohamadi-Nejad A.; et al. (2002). "The thermal analysisnext term of nonezymatic previous termglycosylation of human serum albumin:next term differential scanning calorimetry and circular dichroism studies". Thermochimica Acta. 389 (1–2): 141–151. doi:10.1016/S0040-6031(02)00006-0.
- ↑ Kańska U, Boratyński J (2002). "Thermal glycation of proteins by D-glucose and D-fructose". Arch Immunol Ther Exp (Warsz). 50 (1): 61–6. PMID 11916310.
- ↑ Rojas A, Romay S, González D, Herrera B, Delgado R, Otero K (2000). "Regulation of endothelial nitric oxide synthase expression by albumin-derived advanced glycosylation end products". Circ Res. 86 (3): E50–4. PMID 10679490.
- ↑ Iberg N, Flückiger R (1986). "Nonenzymatic glycosylation of albumin in vivo. Identification of multiple glycosylated sites". J Biol Chem. 261 (29): 13542–5. PMID 3759977.
- ↑ Garlick R, Mazer J (1983). "The principal site of nonenzymatic glycosylation of human serum albumin in vivo". J Biol Chem. 258 (10): 6142–6. PMID 6853480.
- ↑ Marashi S. A., Safarian S., Moosavi-Movahedi A.A. (2005). "Why major nonenzymatic glycation sites of human serum albumin are preferred to other residues?". Med Hypotheses. 64 (4): 881. PMID 15694713.