Hospital-acquired pneumonia
|
Hospital-acquired pneumonia Microchapters |
|
Differentiating Hospital-Acquired Pneumonia from other Diseases |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hospital-acquired pneumonia On the Web |
|
American Roentgen Ray Society Images of Hospital-acquired pneumonia |
|
Directions to Hospitals Treating Hospital-acquired pneumonia |
|
Risk calculators and risk factors for Hospital-acquired pneumonia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Historical Perspective
Pathophysiology
Causes
Differentiating Hospital-acquired pneumonia from other Diseases
Epidemiology and Demographics
Risk Factors
Natural History, Complications and Prognosis
Diagnosis
Diagnostic criteria
History and Symptoms
Physical Examination
Laboratory Findings
Chest X Ray
CT
Treatment
Medical Therapy
Prevention
Clinical Features
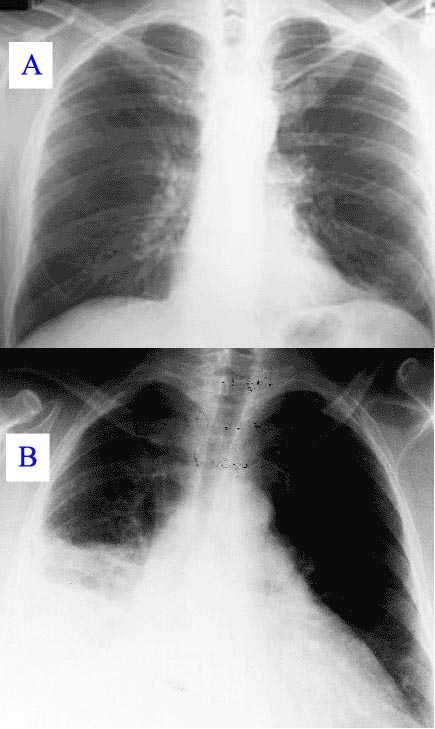
New or progressive infiltrate on the chest X-Ray with one of the following:[1]
- Fever > 37.8 °C (100 °F)
- Purulent sputum
- Leucocytosis > 10.000 cells/μl
Diagnosis
In hospitalised patient who develop respiratory symptoms and fever one should consider the diagnosis. The likelyhood increases when upon investigation symptoms are found of respiratory insufficiency, purulent secretions, newly developed infiltrate on the chest X-Ray, and increasing leucocyte count. If pneumonia is suspected material from sputum or tracheal aspirates are sent to the microbiology department for cultures. In case of pleural effusion thoracentesis is performed for examination of pleural fluid. In suspected ventilator-associated pneumonia it has been suggested that bronchoscopy(BAL) is necessary because of the known risks surrounding clinical diagnoses.[2][1]
Diagnostic criteria of hospital acquired pneumonia
Community acquired pneumonia should be distinguished from healthcare-associated pneumonia as these diseases have different causative organism, prognosis, diagnostic and treatment guidelines. According to the Infectious Diseases Society of America and the American Thoracic Society healthcare-associated pneumonia includes any patient who meet the below criteria [3]
- Hospitalized in an acute care hospital for 2 or more days within 90 days of the infection;
- Resided in a nursing home or long-term care facility;
- Received recent intravenous antibiotic therapy, chemotherapy, or wound care within the past 30 days of the current infection;
- Attended a hospital or hemodialysis clinic
Differential diagnosis
Treatment
Usually initial therapy is empirical.[1] If sufficient reason to suspect influenza one might consider amantadine or rimantadine. In case of legionellosis erythromicin or fluoroquinolone.[2]
A third generation cephalosporin (ceftazidime) + carbapenems (imipenem) + beta lactam & beta lactamase inhibitors (piperacillin/tazobactum)
References
- ↑ 1.0 1.1 1.2
- ↑ 2.0 2.1
- ↑ Attridge RT, Frei CR (2011). "Health care-associated pneumonia: an evidence-based review". The American Journal of Medicine. 124 (8): 689–97. doi:10.1016/j.amjmed.2011.01.023. PMID 21663884. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help)