Hodgkin's lymphoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 11: | Line 11: | ||
OMIM = | | OMIM = | | ||
MedlinePlus = 000580 | | MedlinePlus = 000580 | | ||
DiseasesDB = 5973 | | DiseasesDB = 5973 | | ||
}} | }} | ||
| Line 119: | Line 117: | ||
==References== | ==References== | ||
{{reflist|2}} | |||
==External links== | ==External links== | ||
| Line 165: | Line 161: | ||
[[sv:Hodgkins lymfom]] | [[sv:Hodgkins lymfom]] | ||
[[Category:Disease state]] | |||
[[Category:Hematology]] | [[Category:Hematology]] | ||
[[Category:Types of cancer]] | [[Category:Types of cancer]] | ||
[[Category:Rare diseases]] | [[Category:Rare diseases]] | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Mature chapter]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Revision as of 23:07, 28 July 2011
For patient information click here
Template:DiseaseDisorder infobox
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Hodgkin's lymphoma, also known as Hodgkin's disease, is a type of lymphoma first described by Thomas Hodgkin in 1832. Hodgkin's lymphoma is characterized clinically by the orderly spread of disease from one lymph node group to another and by the development of systemic symptoms with advanced disease. Pathologically, the disease is characterized by the presence of Reed-Sternberg cells. Hodgkin's lymphoma was one of the first cancers to be cured by radiation. Later it was one of the first to be cured by combination chemotherapy. The cure rate is about 93%, making it one of the most curable forms of cancer.
Epidemiology
Unlike some other lymphomas, whose incidence increases with age, Hodgkin's lymphoma has a bimodal incidence curve; that is, it occurs most frequently in two separate age groups, the first being young adulthood (age 15–35) and the second being in those over 55 years old although these peaks may vary slightly with nationality.[1] Overall, it is more common in men, except for the nodular sclerosis variant (see below), which is more common in women.
The annual incidence of Hodgkin's lymphoma is about 1/25,000 people, and the disease accounts for slightly less than 1% of all cancers worldwide.
The incidence of Hodgkin's lymphoma is increased in patients with HIV infection.[2] In contrast to many other lymphomas associated with HIV infection it occurs most commonly in patients with higher CD4 T cell counts.
Symptoms
Swollen but painless lymph nodes are the most common sign of Hodgkin's lymphoma, often occurring in the neck. The lymph nodes of the chest are often affected and these may be noticed on a chest x-ray.
Splenomegaly, or enlargement of the spleen, occurs in about 30% of people with Hodgkin's lymphoma. The enlargement, however, is seldom massive. The liver may also be enlarged due to liver involvement in the disease in about 5% of cases.
About one-third of people with Hodgkin's disease may also notice some systemic symptoms, such as low-grade fever, night sweats, weight loss, itchy skin (pruritus), or fatigue. Classically, involved nodes are painful after alcohol consumption, though this phenomenon is rare. Patients may also present with a cyclic high-grade fever known as Pel-Ebstein fever, although there is debate as to whether or not this truly exists. [3] Systemic symptoms such as fever and weight loss are known as B symptoms.
Diagnosis
Hodgkin's lymphoma must be distinguished from non-cancerous causes of lymph node swelling (such as various infections) and from other types of cancer. Definitive diagnosis is by lymph node biopsy (removal of a piece of lymph node tissue for pathological examination). Blood tests are also performed to assess function of major organs and to assess safety for chemotherapy. Positron emission tomography (PET) is used to detect small deposits that do not show on CT scanning. In some cases a Gallium Scan may be used instead of a PET scan.
Pathology
Macroscopy
Affected lymph nodes (most often, laterocervical lymph nodes) are enlarged, but their shape is preserved because the capsule is not invaded. Usually, the cut surface is white-grey and uniform; in some histological subtypes (e.g. nodular sclerosis) may appear a nodular aspect
Microscopy
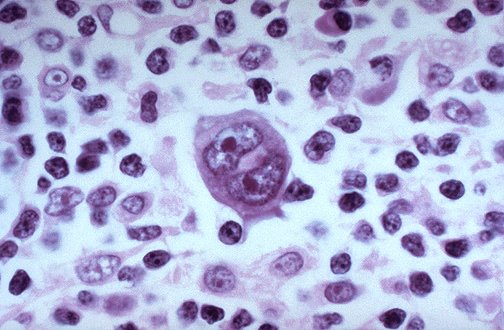
Microscopic examination of the lymph node biopsy reveals complete or partial effacement of the lymph node architecture by scattered large malignant cells known as Reed-Sternberg cells (typical and variants) admixed within a reactive cell infiltrate composed of variable proportions of lymphocytes, histiocytes, eosinophils, and plasma cells. The Reed-Sternberg cells are identified as large often bi-nucleated cells with prominent nucleoli and an unusual CD45-, CD30+, CD15+/- immunophenotype. In approximately 50% of cases, the Reed-Sternberg cells are infected by the Epstein-Barr virus.
Characteristics of classic Reed-Sternberg cells include large size (20–50 micrometres), abundant, amphophilic, finely granular/homogeneous cytoplasm; two mirror-image nuclei (owl eyes) each with an eosinophilic nucleolus and a thick nuclear membrane (chromatin is distributed at the cell periphery).
Variants:
- Hodgkin's cell (atypical mononuclear RSC) is a variant of RS cell, which has the same characteristics, but is mononucleated.
- Lacunar RSC is large, with a single hyperlobated nucleus, multiple, small nucleoli and eosinophilic cytoplasm which is retracted around the nucleus, creating an empty space ("lacunae").
- Pleomorphic RSC has multiple irregular nuclei.
- "Popcorn" RSC (lympho-histiocytic variant) is a small cell, with a very lobulated nucleus, small nucleoli.
- "Mummy" RSC has a compact nucleus, no nucleolus and basophilic cytoplasm. [5]
Hodgkin's lymphoma can be sub-classified by histological type. The cell histology in Hodgkin's lymphoma is not as important as it is in non-Hodgkin's lymphoma: the treatment and prognosis in Hodgkin's lymphoma depend on the stage of disease rather than the histotype.
Types
Classical
Classical Hodgkin's lymphoma (excluding nodular lymphocyte predominant Hodgkin's) can be subclassified into 4 pathologic subtypes based upon Reed-Sternberg cell morphology and the composition of the reactive cell infiltrate seen in the lymph node biopsy specimen. (Template:ICDO)
Classic Hodgkin's Lymphoma (CHL) subtypes:
- Nodular sclerosing CHL is the most common subtype and is composed of large tumor nodules with lacunar RS cells subtype composed of numerous classic often pleomorphic RS cells with only few reactive lymphocytes which may easily be confused with diffuse large cell lymphoma. (C81.3, Template:ICDO)
- Mixed-cellularity subtype is a common subtype and is composed of numerous classic RS cells admixed with numerous inflammatory cells including lymphocytes, histiocytes, eosinophils, and plasma cells. (C81.2, Template:ICDO)
- Lymphocyte-rich and
- lymphocyte depleted are rare subtypes.
Other
Nodular lymphocyte predominant Hodgkin's lymphoma (NLPHL) is no longer classified as a form of classic Hodgkin's lymphoma. This is due to the fact that the RSC variants (popcorn cells) that characterize this form of the disease invariably express B lymphocyte markers such as CD20 (thus making NLPHL an unusual form of B cell lymphoma), and that (unlike classic HL) NLPHL may progress to diffuse large B cell lymphoma. There are small but clear differences in prognosis between the various forms.
Lymphocyte predominant HL is an uncommon subtype composed of vague nodules of numerous reactive lymphocytes admixed with large popcorn-shaped RSC. Unlike classic RSC, the non-classic popcorn-shaped RS cells of NLPHL are CD15 and CD30 negative while positive for the B cell marker CD20. (C81.0, Template:ICDO)
Staging
After Hodgkin's lymphoma is diagnosed, a patient will be staged: that is, they will undergo a series of tests and procedures which will determine what areas of the body are affected. These procedures will include documentation of their histology, a physical examination, blood tests, chest X-ray radiographs, computed tomography (CT) scans or magnetic resonance imaging (MRI) scans of the chest, abdomen and pelvis, and a bone marrow biopsy. Positron emission tomography (PET) scan is now used instead of the gallium scan for staging. In the past, a lymphangiogram or surgical laparotomy (which involves opening the abdominal cavity and visually inspecting for tumors) were performed. Lymphangiograms or laparotomies are very rarely performed, having been supplanted by improvements in imaging with the CT scan and PET scan.
On the basis of this staging, the patient will be classified according to a staging classification (the Ann Arbor staging classification scheme is a common one):
- Stage I is involvement of a single lymph node region (I) or single extralymphatic site (Ie);
- Stage II is involvement of two or more lymph node regions on the same side of the diaphragm (II) or of one lymph node region and a contiguous extralymphatic site (IIe);
- Stage III is involvement of lymph node regions on both sides of the diaphragm, which may include the spleen (IIIs) and/or limited contiguous extralymphatic organ or site (IIIe, IIIes);
- Stage IV is disseminated involvement of one or more extralymphatic organs.
The absence of systemic symptoms is signified by adding 'A' to the stage; the presence of systemic symptoms is signified by adding 'B' to the stage.
Prognosis
In 1998, an international effort[6] identified seven prognostic factors that accurately predict the success rate of conventional treatment in patients with locally extensive or advanced stage Hodgkin's lymphoma. Freedom from progression (FFP) at 5 years was directly related to the number of factors present in a patient. The 5-year FFP for patients with zero factors is 84%. Each additional factor lowers the 5-year FFP rate by 7%, such that the 5-year FFP for a patient with 5 or more factors is 42%.
The adverse prognostic factors identified in the international study are:
- Age >= 45 years
- Stage IV disease
- Hemoglobin < 10.5 g/dl
- Lymphocyte count < 600/µl or < 8%
- Male
- Albumin < 4.0 g/dl
- White blood count >= 15,000/µl
Other studies have reported the following to be the most important adverse prognostic factors: mixed-cellularity or lymphocyte-depleted histologies, male sex, large number of involved nodal sites, advanced stage, age of 40 years or more, the presence of B symptoms, high erythrocyte sedimentation rate, and bulky disease (widening of the mediastinum by more than one third, or the presence of a nodal mass measuring more than 10 cm in any dimension.)
Treatment
Patients with early stage disease (IA or IIA) are effectively treated with radiation therapy or chemotherapy. The choice of treatment depends on the age, sex, bulk and the histological subtype of the disease. Patients with later disease (III, IVA, or IVB) are treated with combination chemotherapy alone. Patients of any stage with a large mass in the chest are usually treated with combined chemotherapy and radiation therapy.
Currently, the ABVD chemotherapy regimen is the gold standard for treatment of Hodgkin's disease. The abbreviation stands for the four drugs Adriamycin, bleomycin, vinblastine, and dacarbazine. Developed in Italy in the 1970s, the ABVD treatment typically takes between six and eight months, although longer treatments may be required. Another form of treatment is the newer Stanford V regimen, which is typically only half as long as the ABVD but which involves a more intensive chemotherapy schedule and incorporates radiation therapy. However, in a randomized controlled study, Stanford V was inferior.[7]
Another form of treatment, mainly in Europe for stages > II is BEACOPP. The cure rate with the BEACOPP esc. regimen is approximately 10-15% higher than with standard ABVD in advanced stages. Although this was shown in a landmark paper in The New England Journal of Medicine (Diehl et al.), the US physicians still favor ABVD. Probably because some physicians think that BEACOPP induces more secondary leukemia. However, this seems negligible compared to the higher cure rates. Also, BEACOPP is more expensive because of the G-CSF-support that is required. Currently, the German Hodgkin Study group tests 8x BEACOPP esc vs. 6x BEACOPP esc vs. 8x BEACOPP-14 baseline (HD15-trial).
With appropriate treatment, over 93% of Hodgkin's lymphoma cases are curable.
The high cure rates and long survival of many patients with Hodgkin's lymphoma has led to a high concern with late adverse effects of treatment, including cardiovascular disease and second malignancies such as acute leukemias, lymphomas, and solid tumors within the radiation therapy field. Most patients with early stage disease are now treated with abbreviated chemotherapy and involved-field radiation therapy rather than with radiation therapy alone. Clinical research strategies are exploring reduction of the duration of chemotherapy and dose and volume of radiation therapy in an attempt to reduce late morbidity and mortality of treatment while maintaining high cure rates. Hospitals are also treating those who respond quickly to chemo-therapy with no radiation.
See also
References
- ↑ Mauch, Peter (1999). Hodgkin's Disease. Lippincott Williams & Wilkins. pp. 62–64. ISBN 0-7817-1502-4. Unknown parameter
|coauthors=ignored (help) - ↑ Biggar RJ, Jaffe ES, Goedert JJ, Chaturvedi A, Pfeiffer R, Engels EA (2006). "Hodgkin lymphoma and immunodeficiency in persons with HIV/AIDS". Blood. 108 (12): 3786–91. doi:10.1182/blood-2006-05-024109. PMID 16917006.
- ↑ Asher, Richard (July 6, 1995). "Making Sense". The New England Journal of Medicine. 333. Text " pages 66-67 " ignored (help); Check date values in:
|date=(help) - ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ [1]
- ↑ Hasenclever (1998-11-19). "A Prognostic Score for Advanced Hodgkin's Disease". New England Journal of Medicine. 339 (21). Unknown parameter
|coauthour=ignored (help); Check date values in:|date=(help) - ↑ Gobbi PG, Levis A, Chisesi T; et al. (2005). "ABVD versus modified stanford V versus MOPPEBVCAD with optional and limited radiotherapy in intermediate- and advanced-stage Hodgkin's lymphoma: final results of a multicenter randomized trial by the Intergruppo Italiano Linfomi". J. Clin. Oncol. 23 (36): 9198–207. doi:10.1200/JCO.2005.02.907. PMID 16172458.
External links
- Leukaemia CARE
- Hodgkin's Lymphoma Home Page at the American National Cancer Institute
- Lymphoma Association
- Australian Hodgkin's Lymphoma Network
- Timeline of discovery and treatment of Hodgkin's Lymphoma
- Lymphomas in Children and Adolescents The Centre for Cancer and Blood Disorders at Sydney Children’s Hospital provides information on cancers in children and adolescents, including Hodgkin and Non-Hodgkins Lymphomas.
- Hodgkin's Lymphoma
- Hodgkin Disease from The Merck Manual
- Photos at Atlas of Pathology
- Hodgkin's trials at Stanford University
- The Leukemia & Lymphoma Society
- Journal Of A 6 Year Battle with Hodgkins written by Alese Coco (March 10 1984 - May 7 2007).
- Anti-Tr antibody
- Message board for those who have Hodgkin's or in remission
- Lymphoma Support Ireland - Information & Patient Stories Online
- The Hodgkin's Disease List A support group for those afflicted with Hodgkin's Disease
cs:Hodgkinova nemoc
de:Morbus Hodgkin
it:Linfoma di Hodgkin
he:לימפומת הודג'קין
la:Morbus Hodgkin
nl:Hodgkinlymfoom
simple:Hodgkin's lymphoma
sr:Хоџкинова болест
fi:Hodgkinin tauti
sv:Hodgkins lymfom