Herpes zoster physical examination: Difference between revisions
Dima Nimri (talk | contribs) |
Dima Nimri (talk | contribs) (→Rash) |
||
| (5 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
The characteristic physical examination finding of herpes zoster is the [[maculopapular]] rash. The rash in typically unilateral and its distribution is confined to one or two adjacent [[dermatomes]]. As the rash crusts and heals in 7-10 days, a post-inflammatory hyperpigmentation of the skin may result. Other findings, such as cranial and peripheral nerves involvement depend on the location of the [[dorsal root ganglia]] involved. | |||
== Physical Examination == | == Physical Examination == | ||
Physical examination findings of herpes zoster depend on the location of the rash, as well as the stage of the disease: | Physical examination findings of herpes zoster depend on the location of the rash, as well as the stage of the disease: | ||
===Rash=== | |||
The rash of herpes zoster virus is typically unilateral and does not cross the midline. It follows the distribution of one or two adjacent dermatomes. The rash can involve any area of the body, but the most common sites are the face ([[ophthalmic]] division of [[trigeminal nerve]]), neck ([[cervical]] [[dorsal root ganglia]]) or chest ([[thoracic]] [[dorsal root ganglia]]). The rash is initially an erythematous, [[maculopapular]] rash, but over the next 7-10 days, it progresses to pustules and ulceration, with crusts, scabbing or both. Post-inflammatory hyperpigmentation may develop along the affected dermatome(s) as part of the healing process. In the immunocompromised individuals, the rash may be complicated by skin necrosis and scarring.<ref name="pmid23785227">{{cite journal |vauthors=Cohen KR, Salbu RL, Frank J, Israel I |title=Presentation and management of herpes zoster (shingles) in the geriatric population |journal=P T |volume=38 |issue=4 |pages=217–27 |year=2013 |pmid=23785227 |pmc=3684190 |doi= |url=}}</ref><ref name="pmid10375341">{{cite journal |vauthors=Cohen JI, Brunell PA, Straus SE, Krause PR |title=Recent advances in varicella-zoster virus infection |journal=Ann. Intern. Med. |volume=130 |issue=11 |pages=922–32 |year=1999 |pmid=10375341 |doi= |url=}}</ref> | |||
===[[Herpes zoster ophthalmicus]]=== | |||
When the rash involves the [[ophthalmic]] division of the [[trigeminal]] nerve, the same characteristic rash will be present in addition to several [[occular]] and head and neck findings which may or may not accompany the rash. These include<ref name="pmid23785227">{{cite journal |vauthors=Cohen KR, Salbu RL, Frank J, Israel I |title=Presentation and management of herpes zoster (shingles) in the geriatric population |journal=P T |volume=38 |issue=4 |pages=217–27 |year=2013 |pmid=23785227 |pmc=3684190 |doi= |url=}}</ref><ref name="pmid18657721">{{cite journal |vauthors=Mueller NH, Gilden DH, Cohrs RJ, Mahalingam R, Nagel MA |title=Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency |journal=Neurol Clin |volume=26 |issue=3 |pages=675–97, viii |year=2008 |pmid=18657721 |pmc=2754837 |doi=10.1016/j.ncl.2008.03.011 |url=}}</ref><ref name="pmid16009918">{{cite journal |vauthors=Karmon Y, Gadoth N |title=Delayed oculomotor nerve palsy after bilateral cervical zoster in an immunocompetent patient |journal=Neurology |volume=65 |issue=1 |pages=170 |year=2005 |pmid=16009918 |doi=10.1212/01.wnl.0000167287.02490.76 |url=}}</ref><ref name="pmid12449270">{{cite journal |vauthors=Shaikh S, Ta CN |title=Evaluation and management of herpes zoster ophthalmicus |journal=Am Fam Physician |volume=66 |issue=9 |pages=1723–30 |year=2002 |pmid=12449270 |doi= |url=}}</ref>: | |||
*Hutchinson's sign: a rash on the tip of the nose is a strong predictor of eye involvement | |||
*[[Blepharoconjunctivitis]]: edema and inflammation of the outer eyelids | |||
*[[Keratitis]]: presents with signs of corneal inflammation, which presents with eye pain, redness and [[photophobia]] | |||
*[[Uveitis]]: presents with eye redness and elevated intraocular pressure | |||
*Cranial nerve palsies: herpes zoster virus may involves cranial nerves III, VI and less commonly, IV. Involvement of these cranial nerves may present with pain on eye movement ([[ophthalmoplegia]]), as well as pupillary dilatation with a sluggish reaction to light when cranial nerve III is involved.<ref name="pmid18657721">{{cite journal |vauthors=Mueller NH, Gilden DH, Cohrs RJ, Mahalingam R, Nagel MA |title=Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency |journal=Neurol Clin |volume=26 |issue=3 |pages=675–97, viii |year=2008 |pmid=18657721 |pmc=2754837 |doi=10.1016/j.ncl.2008.03.011 |url=}}</ref><ref name="pmid16009918">{{cite journal |vauthors=Karmon Y, Gadoth N |title=Delayed oculomotor nerve palsy after bilateral cervical zoster in an immunocompetent patient |journal=Neurology |volume=65 |issue=1 |pages=170 |year=2005 |pmid=16009918 |doi=10.1212/01.wnl.0000167287.02490.76 |url=}}</ref> | |||
===[[Ramsay Hunt Syndrome]]=== | |||
Rarely, herpes zoster may present with a [[maculopapular]] rash in the external auditory canal (zoster opticus) or the tympanic membrane. [[Ramsay Hunt Syndrome]] refers to zoster rash in the external auditory canal, the [[tympanic membrane]], the ipsilateral anterior two-thirds of the tongue or hard palate, associated with ipsilateral weakness or paralysis of the facial muscles, due to involvement of cranial nerve VII. Syndrome may be associated with signs of hearing loss, involuntary eye movements and nystagmus.<ref name="pmid23785227">{{cite journal |vauthors=Cohen KR, Salbu RL, Frank J, Israel I |title=Presentation and management of herpes zoster (shingles) in the geriatric population |journal=P T |volume=38 |issue=4 |pages=217–27 |year=2013 |pmid=23785227 |pmc=3684190 |doi= |url=}}</ref><ref name="pmid18657721">{{cite journal |vauthors=Mueller NH, Gilden DH, Cohrs RJ, Mahalingam R, Nagel MA |title=Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency |journal=Neurol Clin |volume=26 |issue=3 |pages=675–97, viii |year=2008 |pmid=18657721 |pmc=2754837 |doi=10.1016/j.ncl.2008.03.011 |url=}}</ref><ref name="pmid11459884">{{cite journal |vauthors=Sweeney CJ, Gilden DH |title=Ramsay Hunt syndrome |journal=J. Neurol. Neurosurg. Psychiatr. |volume=71 |issue=2 |pages=149–54 |year=2001 |pmid=11459884 |pmc=1737523 |doi= |url=}}</ref> | |||
===Other neurological manifestations=== | |||
*[[Cervical]] dermatomal distribution: rash may be followed by a [[lower motor neuron]] ([[LMN]]) weakness in the arm or diaphragmatic weakness<ref name="pmid18657721">{{cite journal |vauthors=Mueller NH, Gilden DH, Cohrs RJ, Mahalingam R, Nagel MA |title=Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency |journal=Neurol Clin |volume=26 |issue=3 |pages=675–97, viii |year=2008 |pmid=18657721 |pmc=2754837 |doi=10.1016/j.ncl.2008.03.011 |url=}}</ref><ref name="pmid8891477">{{cite journal |vauthors=Merchut MP, Gruener G |title=Segmental zoster paresis of limbs |journal=Electromyogr Clin Neurophysiol |volume=36 |issue=6 |pages=369–75 |year=1996 |pmid=8891477 |doi= |url=}}</ref> | |||
*[[Thoracic]] dermatomal distribution: may be associated with abdominal muscles weakness, which may result in abdominal [[herniation]]<ref name="pmid18657721">{{cite journal |vauthors=Mueller NH, Gilden DH, Cohrs RJ, Mahalingam R, Nagel MA |title=Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency |journal=Neurol Clin |volume=26 |issue=3 |pages=675–97, viii |year=2008 |pmid=18657721 |pmc=2754837 |doi=10.1016/j.ncl.2008.03.011 |url=}}</ref> | |||
===Gallery=== | ===Gallery=== | ||
Latest revision as of 16:44, 24 October 2016
|
Herpes zoster Microchapters |
|
Diagnosis |
|---|
|
History and Symptoms |
|
Treatment |
|
Case Studies |
|
Herpes zoster physical examination On the Web |
|
American Roentgen Ray Society Images of Herpes zoster physical examination |
|
Risk calculators and risk factors for Herpes zoster physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; L. Katie Morrison, MD; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2], Jesus Rosario Hernandez, M.D. [3], Dima Nimri, M.D. [4].
Overview
The characteristic physical examination finding of herpes zoster is the maculopapular rash. The rash in typically unilateral and its distribution is confined to one or two adjacent dermatomes. As the rash crusts and heals in 7-10 days, a post-inflammatory hyperpigmentation of the skin may result. Other findings, such as cranial and peripheral nerves involvement depend on the location of the dorsal root ganglia involved.
Physical Examination
Physical examination findings of herpes zoster depend on the location of the rash, as well as the stage of the disease:
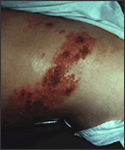
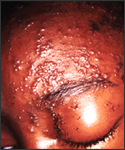
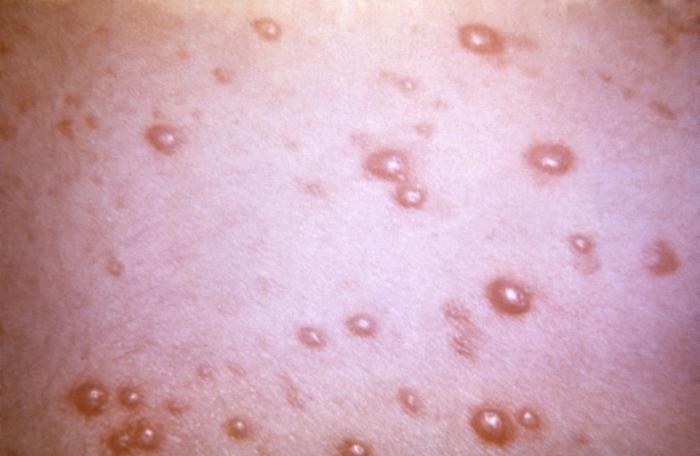
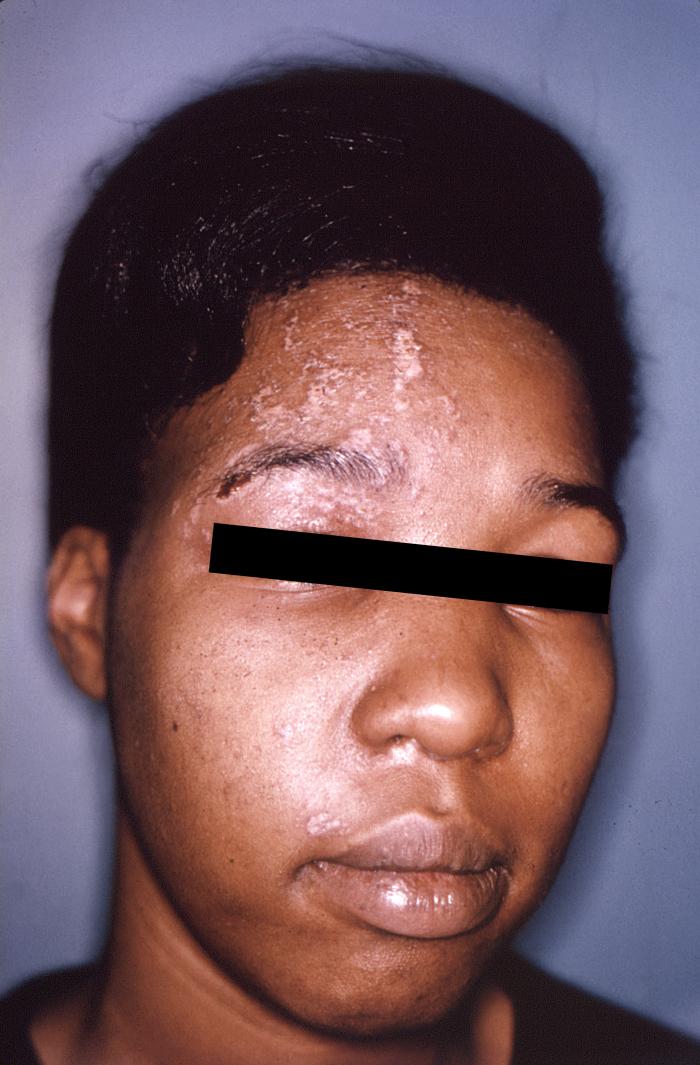
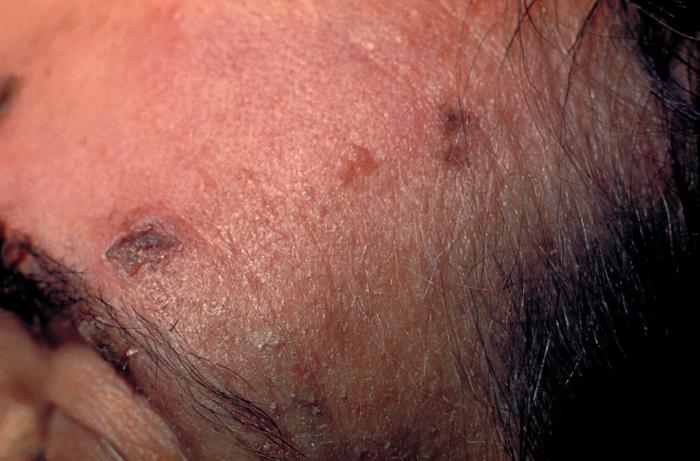
Rash
The rash of herpes zoster virus is typically unilateral and does not cross the midline. It follows the distribution of one or two adjacent dermatomes. The rash can involve any area of the body, but the most common sites are the face (ophthalmic division of trigeminal nerve), neck (cervical dorsal root ganglia) or chest (thoracic dorsal root ganglia). The rash is initially an erythematous, maculopapular rash, but over the next 7-10 days, it progresses to pustules and ulceration, with crusts, scabbing or both. Post-inflammatory hyperpigmentation may develop along the affected dermatome(s) as part of the healing process. In the immunocompromised individuals, the rash may be complicated by skin necrosis and scarring.[1][2]
Herpes zoster ophthalmicus
When the rash involves the ophthalmic division of the trigeminal nerve, the same characteristic rash will be present in addition to several occular and head and neck findings which may or may not accompany the rash. These include[1][3][4][5]:
- Hutchinson's sign: a rash on the tip of the nose is a strong predictor of eye involvement
- Blepharoconjunctivitis: edema and inflammation of the outer eyelids
- Keratitis: presents with signs of corneal inflammation, which presents with eye pain, redness and photophobia
- Uveitis: presents with eye redness and elevated intraocular pressure
- Cranial nerve palsies: herpes zoster virus may involves cranial nerves III, VI and less commonly, IV. Involvement of these cranial nerves may present with pain on eye movement (ophthalmoplegia), as well as pupillary dilatation with a sluggish reaction to light when cranial nerve III is involved.[3][4]
Ramsay Hunt Syndrome
Rarely, herpes zoster may present with a maculopapular rash in the external auditory canal (zoster opticus) or the tympanic membrane. Ramsay Hunt Syndrome refers to zoster rash in the external auditory canal, the tympanic membrane, the ipsilateral anterior two-thirds of the tongue or hard palate, associated with ipsilateral weakness or paralysis of the facial muscles, due to involvement of cranial nerve VII. Syndrome may be associated with signs of hearing loss, involuntary eye movements and nystagmus.[1][3][6]
Other neurological manifestations
- Cervical dermatomal distribution: rash may be followed by a lower motor neuron (LMN) weakness in the arm or diaphragmatic weakness[3][7]
- Thoracic dermatomal distribution: may be associated with abdominal muscles weakness, which may result in abdominal herniation[3]
Gallery
Skin
(Images shown below courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, CA)
-
Herpes Zoster: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Herpes Zoster: Dermatomally distributed vesicles in patient with HZV infection.
-
Herpes Zoster: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Shingles on waist
-
Dermatomal involvement of rash
-
Dermatomal involvement of skin rash
-
Herpes zoster on the chest
-
-
Varicella zoster
-
Herpes Zoster.
(Courtesy of Josh Fierer, M.D. and Charlie Goldberg, M.D.) -
Herpes Zoster C3 Distribution: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Herpes Zoster C3 Distribution: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Shingles on face
-
Shingles on face
-
Child with shingles who had a history of leukemia
-
The pathologic changes seen on the surface of the right unilateral side of this elderly male patient’s tongue and chin, represent a herpes outbreak due to the Varicella zoster virus (VZV) pathogen.
-
The pustulo-vesicular rash on this African-American woman’s face, represents a herpes outbreak due to the Varicella zoster virus (VZV) pathogen.
-
This 1968 image depicted a number of varicella, or chickenpox lesions on a patient’s back, which were displaying the characteristic “cropping” distribution, or manifesting themselves in clusters, each in a different developmental stage.
-
This skin disorder was found to be herpes zoster, not syphilitic in nature as was initially suspected.
-
A case of shingles that demonstrates the typical dermatomal distribution, in this case C8/T1
Head
Trunk
Extremities
Neck
Genitourinary System
Skin
(Images shown below courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, CA)
-
Herpes Zoster: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Herpes Zoster: Dermatomally distributed vesicles in patient with HZV infection.
-
Herpes Zoster: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Shingles on waist
-
Dermatomal involvement of rash
-
Dermatomal involvement of skin rash
-
Herpes zoster on the chest
-
-
Varicella zoster
-
Herpes Zoster.
(Courtesy of Josh Fierer, M.D. and Charlie Goldberg, M.D.) -
Herpes Zoster C3 Distribution: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Herpes Zoster C3 Distribution: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Shingles on face
-
Shingles on face
-
Child with shingles who had a history of leukemia
-
The pathologic changes seen on the surface of the right unilateral side of this elderly male patient’s tongue and chin, represent a herpes outbreak due to the Varicella zoster virus (VZV) pathogen.
-
The pustulo-vesicular rash on this African-American woman’s face, represents a herpes outbreak due to the Varicella zoster virus (VZV) pathogen.
-
This 1968 image depicted a number of varicella, or chickenpox lesions on a patient’s back, which were displaying the characteristic “cropping” distribution, or manifesting themselves in clusters, each in a different developmental stage.
-
This skin disorder was found to be herpes zoster, not syphilitic in nature as was initially suspected.
-
A case of shingles that demonstrates the typical dermatomal distribution, in this case C8/T1
Gallery
-
Skin disorder was found to be herpes zoster. From Public Health Image Library (PHIL). [8]
-
Plantar foot rash was suspected to be smallpox related, but was later determined to be caused by herpes zoster virus. From Public Health Image Library (PHIL). [8]
References
- ↑ 1.0 1.1 1.2 Cohen KR, Salbu RL, Frank J, Israel I (2013). "Presentation and management of herpes zoster (shingles) in the geriatric population". P T. 38 (4): 217–27. PMC 3684190. PMID 23785227.
- ↑ Cohen JI, Brunell PA, Straus SE, Krause PR (1999). "Recent advances in varicella-zoster virus infection". Ann. Intern. Med. 130 (11): 922–32. PMID 10375341.
- ↑ 3.0 3.1 3.2 3.3 3.4 Mueller NH, Gilden DH, Cohrs RJ, Mahalingam R, Nagel MA (2008). "Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency". Neurol Clin. 26 (3): 675–97, viii. doi:10.1016/j.ncl.2008.03.011. PMC 2754837. PMID 18657721.
- ↑ 4.0 4.1 Karmon Y, Gadoth N (2005). "Delayed oculomotor nerve palsy after bilateral cervical zoster in an immunocompetent patient". Neurology. 65 (1): 170. doi:10.1212/01.wnl.0000167287.02490.76. PMID 16009918.
- ↑ Shaikh S, Ta CN (2002). "Evaluation and management of herpes zoster ophthalmicus". Am Fam Physician. 66 (9): 1723–30. PMID 12449270.
- ↑ Sweeney CJ, Gilden DH (2001). "Ramsay Hunt syndrome". J. Neurol. Neurosurg. Psychiatr. 71 (2): 149–54. PMC 1737523. PMID 11459884.
- ↑ Merchut MP, Gruener G (1996). "Segmental zoster paresis of limbs". Electromyogr Clin Neurophysiol. 36 (6): 369–75. PMID 8891477.
- ↑ 8.0 8.1 "Public Health Image Library (PHIL)".




































![Skin disorder was found to be herpes zoster. From Public Health Image Library (PHIL). [8]](/images/d/d6/Chickenpox31.jpeg)
![Plantar foot rash was suspected to be smallpox related, but was later determined to be caused by herpes zoster virus. From Public Health Image Library (PHIL). [8]](/images/5/5a/Chickenpox30.jpeg)