Herpes simplex orofacial infection: Difference between revisions
No edit summary |
Sam Norris (talk | contribs) No edit summary |
||
| Line 645: | Line 645: | ||
[[Category:Otolaryngology]] | [[Category:Otolaryngology]] | ||
[[Category:Urology]] | [[Category:Urology]] | ||
[[Category: | [[Category:Up-to-date]] | ||
Latest revision as of 19:11, 4 October 2021
| Herpesviral vesicular dermatitis | |
 | |
|---|---|
| Herpes lesion on upper lip and face |
|
Herpes simplex Microchapters |
|
Patient Information |
|
Classification |
|
Herpes simplex orofacial infection On the Web |
|
Risk calculators and risk factors for Herpes simplex orofacial infection |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Anahita Deylamsalehi, M.D.[2] ; Cafer Zorkun, M.D., Ph.D. [3]
Overview
Infection by HSV-1 is the most common cause of herpes that affects the face and mouth (orofacial herpes), although within the recent years an increase in oral HSV-2 infections has been reported. Studies demonstrated different rate of herpes simplex orofacial infection prevalence in different populations, nevertheless lifetime prevalences of herpes simplex orofacial infection has been estimated 42.1% and 32.4%, in women and men, respectively. There are some evidences that report higher rate of herpes simplex orofacial infection in low socioeconomic status. A majority of primary HSV-1 infections occur during childhood. Early HSV infection could be asymptomatic without any obvious skin lesions. Transmission commonly occurs when infection source comes in contact with the mucosa or abraded skin. However there are other rout of transmission such as infants born to infected mothers who are also at risk of catching the HSV-1 during the delivery. The estimated duration of primary HSV infection has been estimated between 2-20 days after contact with the source of infection. Skin involvement usually appear as grouped ulcers or vesicles on an erythematous base. Subsequently skin vesicles may ulcerate and then become crusted. Primary HSV infection in adolescents frequently manifests as severe pharyngitis with lesions developing on the cheek and gums. Some individuals develop difficulty in swallowing. Once a primary oral HSV-1 infection has resolved, the HSV enters the nerves surrounding the primary lesion, migrates to the cell body of the neuron, and becomes latent in the trigeminal ganglion. In some patients, the virus reactivates to cause recurrent infection, which is more common with HSV-1 than HSV-2 oral infection. Even though trigeminal ganglion is the most common location for HSV-1 infection, inferior and superior cervical ganglia could also become infected with this serotype of herpes simplex. Prodromal symptoms often precede a recurrence, which typically begins with reddening of the skin around the infected site. Pain, itching and paresthesia are some of the other prodromal symptoms in herpes simplex infection. Duration of the prodromal symptoms can range between few hours to several days before lesions develop. Some factors such as concurrent viral infection, trauma, menstural period, fatigue, stress and sun exposure could trigger recurrent herpes simplex lesions. It has been estimated that patients with HSV-1 orofacial infection could experience recurrent infections 1-6 times in a year. Each episode of orofacial infection is less sever and shorter, compared to previous episodes of orofacial infections. There are numerous differential diagnosis such as oral candidiasis, aphthous ulcers, squamous cell carcinoma, leukoplakia, behcet's disease, crohn's disease and burning mouth syndrome. Some conditions such as leukemia, bell's palsy, chronic atopic dermatitis and Human immunodeficiency virus infection have been known as associated conditions in orofacial herpes. Orofacial herpes simplex infection is usually diagnosed clinically, nevertheless PCR test, immunodot glycoprotein G-specific (IgG) test, skin biopsy, virus culture and direct fluorescent anti body (DFA) studies are some of the available laboratory investigations to better diagnose orofacial infection due to herpes simplex. Unfortunately there is no approved treatment to completely eradicate the herpes simplex virus from body. Nevertheless antiviral treatments have been successful in lowering the severity and duration of skin lesions. The available antiviral drugs that can be used for herpes simplex infection include acyclovir, valaciclovir, famciclovir and penciclovir. Acyclovir is effective in decreasing the viral shedding period in infected patients (median of 2.5 days when patients received acyclovir, compared to 17 days). It also has been reported to be efficient in augmenting pain resolution and healing of the skin lesions.
Epidemiology
- Based on a study, lifetime prevalences of herpes simplex orofacial infection are 42.1% and 32.4%, in women and men, respectively. Moreover HSV1 prevalence was estimated 50.3%.[1]
- Another study reported herpes simplex infection rate approximately 70-80% in low socioeconomic status and 40%-60% in high socioeconomic status individuals. [2]
- Prevalence of HSV-1 estimated as 57.7% in US population. [3]
- Based on a study done on college students demonstrated that 25.6 % of first year college students had history of recurrent orofacial HSV-1 infection compared to 28 % in fourth-year students.
- A study done in France estimated annual prevalence of orofacial herpes simplex infection as 14.8% (only 23% of these population were aware of their infection). Based on this study female population has higher chance of infection, compared to male populations.[4]
Clinical Presentations
- Early HSV infection could be asymptomatic without any obvious symptoms (Also called asymptomatic seroconversion).[5]
- A majority of primary HSV-1 infections occur during childhood and if the virus comes into contact with the mucosa or abraded skin, it can cause acute herpetic gingivostomatitis (inflammation of the cheek's mucosa and gums) within 5–10 days. Some other symptoms may also develop, including fever and sore throat, refuse to eat or drink and painful ulcers may appear.[6]
- Prodromal symptoms often precede a recurrence, which typically begins with reddening of the skin around the infected site, with eventual ulceration to form fluid-filled blisters that affect the lip (labial) tissue and the area between the lip and skin (vermillion border).[6] [7]
- The following list includes some of the prodromal symptoms in herpes simplex infection:[8]
- Itching
- Pain
- Paresthesia (may be described as tingling)
- Duration of the prodromal symptoms can range between few hours to several days before lesions develop.
- Most of the time orofacial infection just involves lips and oral mucosa and is often called herpes simplex labialis.
- Skin involvement usually appear as grouped ulcers or vesicles on an erythematous base. Subsequently skin vesicles may ulcerate (severely painful at this stage) and then become crusted.[9]
- Presence of cervical or submandibular lymphadenopathy is possible during the orofacial HSV-1 infection.
- The estimated duration of primary HSV infection has been estimated between 2-20 days after contact with the source of infection.
- Primary HSV infection in adolescents frequently manifests as severe pharyngitis with lesions developing on the cheek and gums. Some individuals develop difficulty in swallowing (dysphagia) and swollen lymph nodes (lymphadenopathy).[6]
- Primary HSV infections in adults often presents as pharyngitis similar to that observed in glandular fever (infectious mononucleosis), but gingivostomatitis is less likely. The symptoms of primary HSV infection generally resolve within two weeks.[6]
- Immunodeficient patients can develop sever and atypical manifestations such as linear erosions in skin creases which has a similar appearance to knife cuts (Knife-Cut Sign). [10]

- Ocular infection due to HSV-2 can present as acute retinal necrosis syndrome.
Disease Progression And Recurrence
- Transmission of HSV-1 usually occurs via direct contact with skin lesions or body fluids of the involved patient (aerosol and fomite spread are rare). In orofacial infection the virus get inoculated onto oropharynx and conjunctiva or through small cracks in the skin.[11] [12]
- Some occupations such as dentists, hospital, nursery or respiratory care unit personnel are at risk of HSV-1 spread via patient's oral secretion. The aforementioned occupations are also at risk of herpes simplex infection due to hospital outbreaks.
- Outbreaks are also reported in some athletes, such as wrestlers.[13]
- Infants born to infected mothers are also at risk of catching the HSV-1 during the delivery.[14]
- HSV-1 infection can be transmitted through sexual activity especially in men who have sex with men.[15]
- Incubation period of primary infection is very short, approximately 5 days. [15]
- Based on reports, viral shedding last for 60 hours (when measured by PCR) and 48 hours (when measured by culture).[16]
- Once a primary oral HSV-1 infection has resolved, the HSV enters the nerves surrounding the primary lesion, migrates to the cell body of the neuron, and becomes latent in the trigeminal ganglion. In some patients, the virus reactivates to cause recurrent infection; which is more common with HSV-1 than HSV-2 oral infection.[6] [17]
- Even though trigeminal ganglion is the most common location for HSV-1 infection, inferior and superior cervical ganglia could also become infected with this serotype of herpes simplex.[18]
- After initial infection with one type of herpes simplex virus antibody development occurs which prevent another form of infection with the same type. Based on this, a patient with history of orofacial HSV-1 infection is immune against herpetic whitlow, ocular infection or genital herpes simplex caused by HSV-1. Antibody production occurs 6 months after the initial infection with HSV-1.[19]
- Even though infection with HSV-1 will not protect patients from HSV-2 infection, it will decrease the severity of HSV-2 infection.[20]
- Most of the time recurrent episodes of HSV-1 orofacial infection just involves lips and oral mucosa which is called herpes simplex labialis. Rare occasions of reinfections occur inside the mouth (intraoral HSV stomatitis), affecting the gums, alveolar ridge, hard palate, and the back of the tongue. This may be accompanied by herpes labialis.[6] [21][22]
- It seems that some factors are responsible for recurrent herpes simplex infection due to decreasing the cell mediated immunity (either antigen dependent or no antigen dependent). the following list contains some of these factors:[23][24][25][26][27][4]
- Other viral infections with fever
- Fatigue
- Menstural period
- Stress
- Local trauma
- Ultraviolet light
- Local injury due to high temprature or frostbite
- Sun exposure
- A study reported a protein named protein VP16 as an involved factor in infection recurrency.
- It has been estimated that patients with HSV-1 orofacial infection could experience recurrent infections 1-6 times in a year. Each episode of orofacial infection is less sever and shorter, compared to previous episodes of orofacial infections. [8]
- Chance of recurrent orofacial involvement has been estimated 0.12 monthly.[28]
- Oral herpes is spread by direct contact with an active sore in an infected person, for instance, by kissing. However, the virus can be transmitted through the skin in the absence of a lesion.
- Oral herpes and cold sores can sometimes be confused with canker sores.
- Healing time has been estimated 10 to 14 days, based on a study done on herpes simplex infections.[8]
Differential diagnosis
Herpes simplex orofacial infection must be differentiated from other diseases causing oral lesions such as leukoplakia and herpes simplex virus infection.[29]
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
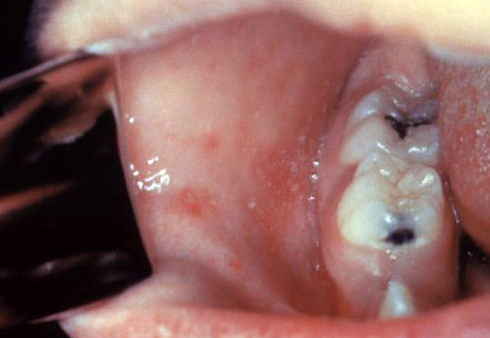
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |  | |||||
| Aphthous ulcers |
|
|
|
 | ||
| Squamous cell carcinoma |
|
 | ||||
| Leukoplakia |
|
|
|
|
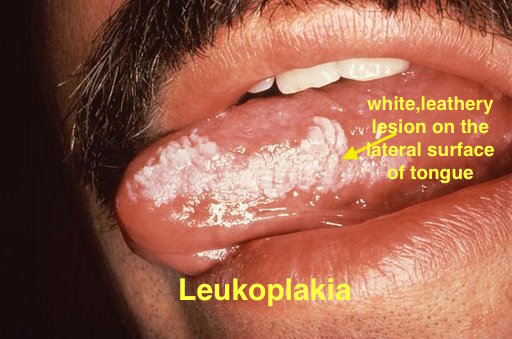 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
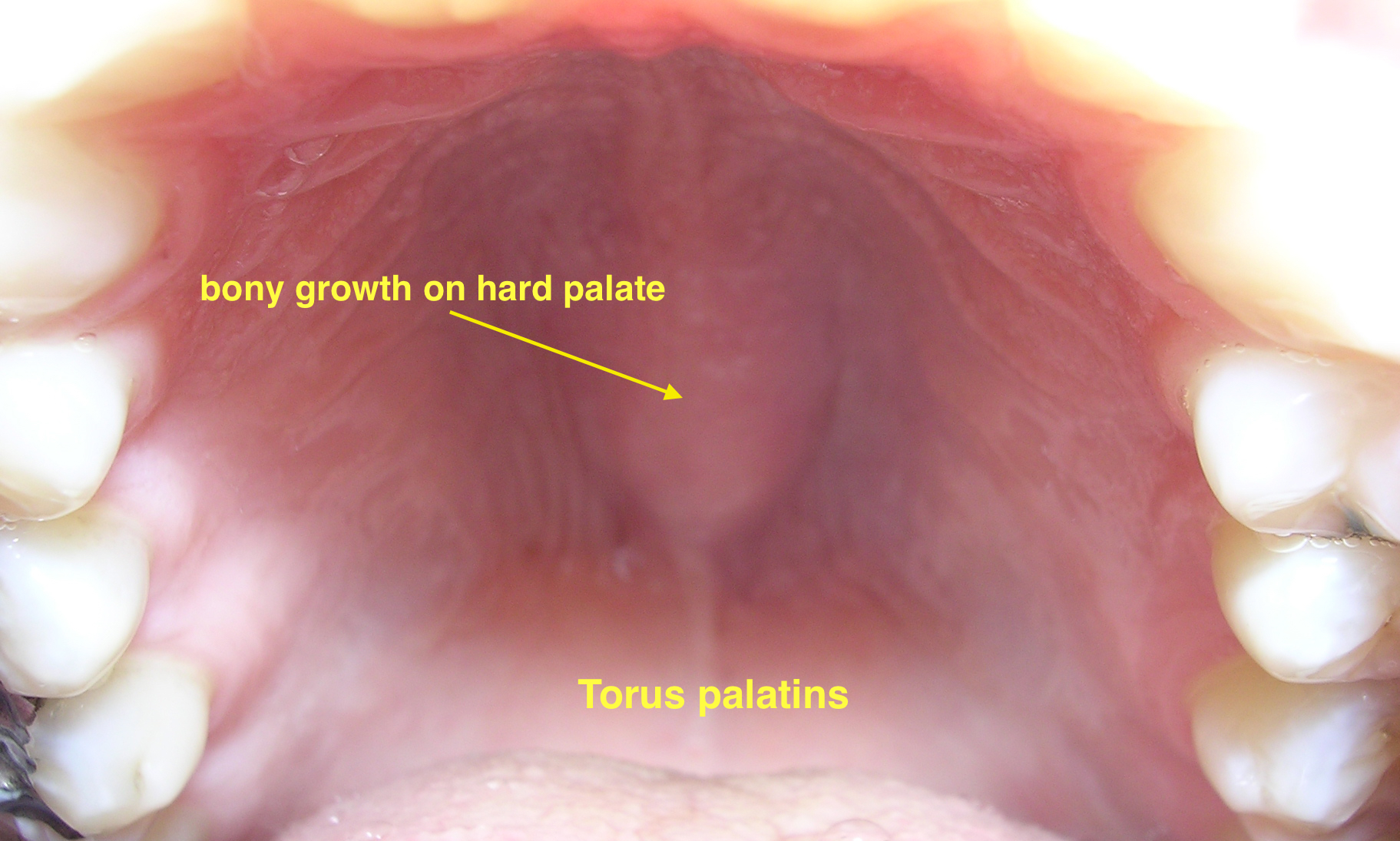 | ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
 | |||
| Crohn's disease |
|
|
||||
| Agranulocytosis |
|
|
||||
| Syphilis[32] |
|
|
|
 | ||
| Coxsackie virus |
|
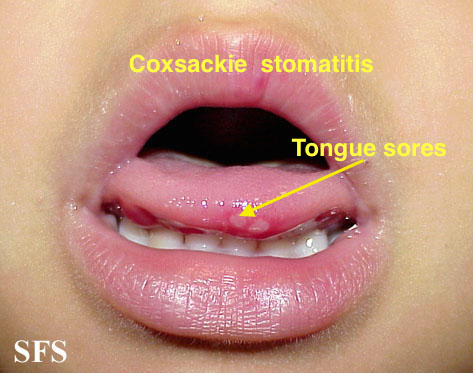
| ||||
| Chicken pox |
|
|
|
 | ||
| Measles |
|
|
|
|
 | |
Associated Conditions
- Leukemia:[35][36]
- Herpes simplex orofacial infection has been reported in 40% of patients with acute leukemia.
- Chronic atopic dermatitis:
- Chronic atopic dermatitis is associated with a form of herpes simplex infection in the eczematous areas (eczema herpeticum).
- It seems that atopic dermatitis in this patients further augments the herpes simplex infection spread within the eczematous skin.
- Bell's palsy:[37]
- Although the explicit cause of bell's palsy is not fully understood, but it could be related to reactivation of HSV-1 infection.
- Human immunodeficiency virus (HIV) infection
Prognosis
- Many patients with herpes simplex infection experience recurrent lesions within the first year after infection.[38]
- Symptoms in recurrent infection can range from minor burning or just an itch to painful facial lesions that may cause debilitation.
- Based on some reports genetical factors may play a role in prognosis of orofacial herpes simplex infection.
Diagnosis
- Orofacial herpes simplex infection is usually diagnosed clinically. Skin and oral involvement usually present as multiple superficial round ulcers on face or mouth with or without acute gingivitis.[39]
- Although most orofacial infections of herpes simplex is due to HSV-1, nevertheless HSV-2 could be also responsible in some cases. Hence differentiating the two serotypes could be necessary in some occasions.
- PCR test which detects herpes simplex antibodies and immunodot glycoprotein G-specific (IgG) test are two specific tests (more than 98%) to differentiate these two different serotypes. [40][16]
- Beside PCR test there are some other laboratory tests include skin biopsy, virus culture and direct fluorescent anti body (DFA) studies.[39]
- If it is possible tissue culture for diagnosis should be taken from vesicles. Highest measure of herpes simplex virus has been found in the first 24 to 48 hours of vesicles appearance. [41]
- Compared to tissue culture, direct fluorescent antibody testing is capable of detecting 80 % of HSV infections.[42]
- Tzanck test require expert personnel to perform the test. It is reported positive if multinucleated giant cells are seen. Tzanck test could not be used to differente HSV-1 from HSV-2, nevertheless it's sensitivity has been estimated 40-77 % for herpetic gingivostomatitis.[43]
Treatment
Unfortunately, there is no approved treatment to completely eradicate the herpes simplex virus from the body. Nevertheless, antiviral treatments have been successful in lowering the severity and duration of skin lesions. Soft, smooth, and cold foods are helpful in lowering the symptoms severity during meals.
Antiviral drugs
- The available antiviral drugs that can be used for herpes simplex infection include acyclovir, valaciclovir, famciclovir and penciclovir.[44][45][46]
- Based on a double-blind, placebo controlled, randomized trial done on patients with recurrent herpes simplex orofacial infection showed efficacy of 5% acyclovir cream containing propylene glycol in reducing the period of vesiculation (P = 0.016), healing time (P = 0.022) and itching duration.[47] [35]
- Another study done on 703 patients with herpes simplex keratitis demonstrated the effectiveness of acyclovir therapy for 12 months in lowering the chance of recurrent herpes simplex orofacial infection, including the ocular infection. [48]
- Data from different studies suggest the use of acyclovir and valaciclovir in herpes labialis. These two medications are also effective in cancer patients who are infected with herpes simplex infection.[45][49][50][45]
- Based on a study done on 701 randomly selected patients, 1500 mg single dose of famciclovir reduce healing period by 2 days, compared to placebo. The following table is a summary of median healing time in 3 different treatments that have been studied.[51]
| Famciclovir - Single dose | Famciclovir - Single day | Placebo | |
|---|---|---|---|
| Median Healing Time (days) | 4.4 | 4 | 6.2 |
There is no significant difference in famciclovir single dose or famciclovir single day treatement, based on the mentioned study.
- Acyclovir is effective in decreasing the viral shedding period in infected patients (median of 2.5 days when patients recieved acyclovir, compared to 17 days). It also has been reported to be efficient in augmenting pain resolution and healing of the skin lesions.
- In another study total daily dose of 800 mg acyclovir was able to lower the recurrent skin lesions by 53%. Moreover the investigations showed that this dose of acyclovir is related to 71% reduction in tissue culture-positive recurrences, compared to control groups.[46]
- Acyclovir treatment shows less effectiveness in treatment of primary herpetic gingivostomatitis in adults. [52][45]
- Topical use of acyclovir, docosanol and penciclovir has been reported as an effective treatment in herpes labialis. However their efficacy is less than oral antiviral medications.[49][53][54][55]
- An effective treatment for primary herpetic gingivostomatitis in children is oral suspension of acyclovir. It will shorten the duration of infection significantly, if started within the first 3 days.[56]
- Oral treatment with acyclovir has been related with shorter duration of viral shedding in children which can decrease the chance of transmission. The aforementioned treatment has been effective in lowering the severity of oralfacial lesions and improving eating and drinking difficulties.[56]
Analgesics
- Analgesics such as paracetamol (acetaminophen) or ibuprofen can be used in order to control pain and fever (if present).
- Oral analgesics is recommended in children who are experiencing pain and discomfort.
Topical Anesthetics
- Medications such as lidocaine, prilocaine, tetracaine and benzocaine can be prescribe in order to reduce some symptoms such as pain and itching.[57]
- Topical anesthetics are able to decrease symptoms in children in order to improve eating and drinking difficulties due to oral lesions.
Topical Corticosteroids
- Topical corticosteroids (such as clobetasol 0.05% gel) combined with antiviral medications has been reported to be effective in improving the healing process of skin lesions. [58]
Future or Investigational Therapies
- There have been some investigations of a vaccine to prevent orofacial herpes simplex infection. Attacking messenger RNA (mRNA) of essential HSV-1 genes (such as UL20 gene) is how one of the investigated vaccines works. The aforementioned vaccine has been studied on rabbits and showed lower risk of ocular infection due to HSV-1 in them. [59]
- Another idea which requires more study to be approved suggests a medication (such as antagomir) to force all copies of HSV-1 virus to become active at a same time (from the latent status). Since there would be no latent virus in body, antiviral treatments could be successful in destroying the whole virus population.
- Another possible treatment try to target microRNA in order to prevent viruses from become latent.
- A study done on mice reported the possible effectiveness of phosphonoacetic acid in preventing skin lesion development. Based on this study phosphonoacetic acid prevented viruses from become latent when this ointment has been applied three times a day topically.
- Oral or topical use of a new antiviral agent named 2'-Nor-2'-deoxyguanosine (2'NDG) on mice demonstrated reduced severity in orofacial lesions. Minimum effective dose has been estimated as 0.2 mg/kg per day in one study. [60]
Prevention
- Antiviral treatment lower the risk of symptom development in a seropositive patient by 50%, based on a study.
- A 4 month period of 500mg per day valacyclovir oral intake has been reported to be effective in prevention of recurrent herpes labialis in a double-blind, placebo-controlled study.[61]
- Use of condom is also effective in prevention of HSV-1 infection.[62]
- Combination of antiviral treatment and condom use can reduce the chance of transmission by 75% annually.
- Risk of transmission from mother to infant is between 30% to 60% when mother become infected around delivery. Conversly transmission risk decreases to 3% if mother has recurrent infections.[14] [63]
- Suppressive treatment with acyclovir is safe during pregnancy and has been recommended in last months of pregnancy. In contrast valaciclovir and famciclovir use has not been proved to be safe during pregnancy.[64]
References
- ↑ Malvy D, Ezzedine K, Lançon F, Halioua B, Rezvani A, Bertrais S; et al. (2007). "Epidemiology of orofacial herpes simplex virus infections in the general population in France: results of the HERPIMAX study". J Eur Acad Dermatol Venereol. 21 (10): 1398–403. doi:10.1111/j.1468-3083.2007.02302.x. PMID 17958848.
- ↑ Chayavichitsilp P, Buckwalter JV, Krakowski AC, Friedlander SF (2009). "Herpes simplex". Pediatr Rev. 30 (4): 119–29, quiz 130. doi:10.1542/pir.30-4-119. PMID 19339385.
- ↑ Xu F, Sternberg MR, Kottiri BJ, McQuillan GM, Lee FK, Nahmias AJ; et al. (2006). "Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States". JAMA. 296 (8): 964–73. doi:10.1001/jama.296.8.964. PMID 16926356.
- ↑ 4.0 4.1 Lorette G, Crochard A, Mimaud V, Wolkenstein P, Stalder JF, El Hasnaoui A (2006). "A survey on the prevalence of orofacial herpes in France: the INSTANT Study". J Am Acad Dermatol. 55 (2): 225–32. doi:10.1016/j.jaad.2005.10.014. PMID 16844503.
- ↑ Stanberry LR, Kern ER, Richards JT, Abbott TM, Overall JC (1982). "Genital herpes in guinea pigs: pathogenesis of the primary infection and description of recurrent disease". J Infect Dis. 146 (3): 397–404. doi:10.1093/infdis/146.3.397. PMID 6286797.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Bruce AJ, Rogers RS (2004) Oral manifestations of sexually transmitted diseases. Clin Dermatol 22 (6):520-7. DOI:10.1016/j.clindermatol.2004.07.005 PMID: 15596324
- ↑ Herpes Online: Exploring the "H" Community, pages 1-4 American Social Health Association 1996 Access date: 2007-03-29
- ↑ 8.0 8.1 8.2 Cernik C, Gallina K, Brodell RT (2008). "The treatment of herpes simplex infections: an evidence-based review". Arch Intern Med. 168 (11): 1137–44. doi:10.1001/archinte.168.11.1137. PMID 18541820.
- ↑ Patel AR, Romanelli P, Roberts B, Kirsner RS (2007). "Treatment of herpes simplex virus infection: rationale for occlusion". Adv Skin Wound Care. 20 (7): 408–12. doi:10.1097/01.ASW.0000280199.58260.62. PMID 17620742.
- ↑ 10.0 10.1 Cohen PR (2015). "The "Knife-Cut Sign" Revisited: A Distinctive Presentation of Linear Erosive Herpes Simplex Virus Infection in Immunocompromised Patients". J Clin Aesthet Dermatol. 8 (10): 38–42. PMC 4633212. PMID 26557219.
- ↑ Sen P, Barton SE (2007). "Genital herpes and its management". BMJ. 334 (7602): 1048–52. doi:10.1136/bmj.39189.504306.55. PMC 1871807. PMID 17510153.
- ↑ Perl TM, Haugen TH, Pfaller MA, Hollis R, Lakeman AD, Whitley RJ; et al. (1992). "Transmission of herpes simplex virus type 1 infection in an intensive care unit". Ann Intern Med. 117 (7): 584–6. doi:10.7326/0003-4819-117-7-584. PMID 1524332.
- ↑ Belongia EA, Goodman JL, Holland EJ, Andres CW, Homann SR, Mahanti RL; et al. (1991). "An outbreak of herpes gladiatorum at a high-school wrestling camp". N Engl J Med. 325 (13): 906–10. doi:10.1056/NEJM199109263251302. PMID 1652687.
- ↑ 14.0 14.1 Brown ZA, Selke S, Zeh J, Kopelman J, Maslow A, Ashley RL; et al. (1997). "The acquisition of herpes simplex virus during pregnancy". N Engl J Med. 337 (8): 509–15. doi:10.1056/NEJM199708213370801. PMID 9262493.
- ↑ 15.0 15.1 Quinn TC, Corey L, Chaffee RG, Schuffler MD, Brancato FP, Holmes KK (1981). "The etiology of anorectal infections in homosexual men". Am J Med. 71 (3): 395–406. doi:10.1016/0002-9343(81)90167-4. PMID 7025620.
- ↑ 16.0 16.1 Boivin G, Goyette N, Sergerie Y, Keays S, Booth T (2006). "Longitudinal evaluation of herpes simplex virus DNA load during episodes of herpes labialis". J Clin Virol. 37 (4): 248–51. doi:10.1016/j.jcv.2006.09.006. PMID 17046320.
- ↑ Herpes Online: Exploring the "H" Community, pages 1-4 American Social Health Association 1996 Access date: 2007-03-29
- ↑ Cushing H (1983). "Landmark article April 28, 1900: A method of total extirpation of the Gasserian ganglion for trigeminal neuralgia. By a route through the temporal fossa and beneath the middle meningeal artery. By Harvey Cushing". JAMA. 250 (4): 519–28. doi:10.1001/jama.250.4.519. PMID 6345823.
- ↑ Reuven NB, Staire AE, Myers RS, Weller SK (2003). "The herpes simplex virus type 1 alkaline nuclease and single-stranded DNA binding protein mediate strand exchange in vitro". J Virol. 77 (13): 7425–33. doi:10.1128/jvi.77.13.7425-7433.2003. PMC 164775. PMID 12805441.
- ↑ Handsfield HH (2000). "Public Health Strategies to Prevent Genital Herpes: Where Do We Stand?". Curr Infect Dis Rep. 2 (1): 25–30. doi:10.1007/s11908-000-0084-y. PMID 11095834.
- ↑ Herpes Online: Exploring the "H" Community, pages 1-4 American Social Health Association 1996 Access date: 2007-03-29
- ↑ Gilbert S, Corey L, Cunningham A, Malkin JE, Stanberry L, Whitley R; et al. (2007). "An update on short-course intermittent and prevention therapies for herpes labialis". Herpes. 14 Suppl 1: 13A–18A. PMID 17877887.
- ↑ Vestey JP, Norval M, Howie S, Maingay J, Neill WA (1989). "Variation in lymphoproliferative responses during recrudescent orofacial herpes simplex virus infections". Clin Exp Immunol. 77 (3): 384–90. PMC 1542042. PMID 2553308.
- ↑ Oakley C, Epstein JB, Sherlock CH (1997). "Reactivation of oral herpes simplex virus: implications for clinical management of herpes simplex virus recurrence during radiotherapy". Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 84 (3): 272–8. doi:10.1016/s1079-2104(97)90342-5. PMID 9377190.
- ↑ Myśliwska J, Trzonkowski P, Bryl E, Lukaszuk K, Myśliwski A (2000). "Lower interleukin-2 and higher serum tumor necrosis factor-a levels are associated with perimenstrual, recurrent, facial Herpes simplex infection in young women". Eur Cytokine Netw. 11 (3): 397–406. PMID 11022124.
- ↑ Flores R, Lu B, Beibei L, Nielson C, Abrahamsen M, Wolf K; et al. (2008). "Correlates of human papillomavirus viral load with infection site in asymptomatic men". Cancer Epidemiol Biomarkers Prev. 17 (12): 3573–6. doi:10.1158/1055-9965.EPI-08-0467. PMID 19064573.
- ↑ Perna JJ, Mannix ML, Rooney JF, Notkins AL, Straus SE (1987). "Reactivation of latent herpes simplex virus infection by ultraviolet light: a human model". J Am Acad Dermatol. 17 (3): 473–8. doi:10.1016/s0190-9622(87)70232-1. PMID 2821086.
- ↑ Lafferty WE, Coombs RW, Benedetti J, Critchlow C, Corey L (1987). "Recurrences after oral and genital herpes simplex virus infection. Influence of site of infection and viral type". N Engl J Med. 316 (23): 1444–9. doi:10.1056/NEJM198706043162304. PMID 3033506.
- ↑ Scully C (1989). "Orofacial herpes simplex virus infections: current concepts in the epidemiology, pathogenesis, and treatment, and disorders in which the virus may be implicated". Oral Surg Oral Med Oral Pathol. 68 (6): 701–10. doi:10.1016/0030-4220(89)90159-x. PMID 2556674.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.
- ↑ 35.0 35.1 Barrett AP (1986). "A long-term prospective clinical study of orofacial herpes simplex virus infection in acute leukemia". Oral Surg Oral Med Oral Pathol. 61 (2): 149–52. doi:10.1016/0030-4220(86)90177-5. PMID 3515270.
- ↑ Barrett AP (1988). "Chronic indolent orofacial herpes simplex virus infection in chronic leukemia: a report of three cases". Oral Surg Oral Med Oral Pathol. 66 (3): 387–90. doi:10.1016/0030-4220(88)90251-4. PMID 3050711.
- ↑ Prud'hon S, Kubis N (2019). "[Bell's palsy]". Rev Med Interne. 40 (1): 28–37. doi:10.1016/j.revmed.2018.03.011. PMID 29610004.
- ↑ Brown ZA, Gardella C, Wald A, Morrow RA, Corey L (2005). "Genital herpes complicating pregnancy". Obstet Gynecol. 106 (4): 845–56. doi:10.1097/01.AOG.0000180779.35572.3a. PMID 16199646.
- ↑ 39.0 39.1 Fatahzadeh M, Schwartz RA (2007). "Human herpes simplex virus infections: epidemiology, pathogenesis, symptomatology, diagnosis, and management". J Am Acad Dermatol. 57 (5): 737–63, quiz 764-6. doi:10.1016/j.jaad.2007.06.027. PMID 17939933.
- ↑ Ashley RL, Militoni J, Lee F, Nahmias A, Corey L (1988). "Comparison of Western blot (immunoblot) and glycoprotein G-specific immunodot enzyme assay for detecting antibodies to herpes simplex virus types 1 and 2 in human sera". J Clin Microbiol. 26 (4): 662–7. doi:10.1128/JCM.26.4.662-667.1988. PMC 266403. PMID 2835389.
- ↑ Spruance SL, Overall JC, Kern ER, Krueger GG, Pliam V, Miller W (1977). "The natural history of recurrent herpes simplex labialis: implications for antiviral therapy". N Engl J Med. 297 (2): 69–75. doi:10.1056/NEJM197707142970201. PMID 194157.
- ↑ Chan EL, Brandt K, Horsman GB (2001). "Comparison of Chemicon SimulFluor direct fluorescent antibody staining with cell culture and shell vial direct immunoperoxidase staining for detection of herpes simplex virus and with cytospin direct immunofluorescence staining for detection of varicella-zoster virus". Clin Diagn Lab Immunol. 8 (5): 909–12. doi:10.1128/CDLI.8.5.909-912.2001. PMC 96170. PMID 11527802.
- ↑ Chauvin PJ, Ajar AH (2002). "Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management". J Can Dent Assoc. 68 (4): 247–51. PMID 12626280.
- ↑ Bartlett BL, Tyring SK, Fife K, Gnann JW, Hadala JT, Kianifard F; et al. (2008). "Famciclovir treatment options for patients with frequent outbreaks of recurrent genital herpes: the RELIEF trial". J Clin Virol. 43 (2): 190–5. doi:10.1016/j.jcv.2008.06.004. PMID 18621575.
- ↑ 45.0 45.1 45.2 45.3 Glenny AM, Fernandez Mauleffinch LM, Pavitt S, Walsh T (2009). "Interventions for the prevention and treatment of herpes simplex virus in patients being treated for cancer". Cochrane Database Syst Rev (1): CD006706. doi:10.1002/14651858.CD006706.pub2. PMID 19160295.
- ↑ 46.0 46.1 Rooney JF, Straus SE, Mannix ML, Wohlenberg CR, Alling DW, Dumois JA; et al. (1993). "Oral acyclovir to suppress frequently recurrent herpes labialis. A double-blind, placebo-controlled trial". Ann Intern Med. 118 (4): 268–72. doi:10.7326/0003-4819-118-4-199302150-00004. PMID 8380540.
- ↑ Van Vloten WA, Swart RN, Pot F (1983). "Topical acyclovir therapy in patients with recurrent orofacial herpes simplex infections". J Antimicrob Chemother. 12 Suppl B: 89–93. doi:10.1093/jac/12.suppl_b.89. PMID 6355055.
- ↑ "Acyclovir for the prevention of recurrent herpes simplex virus eye disease. Herpetic Eye Disease Study Group". N Engl J Med. 339 (5): 300–6. 1998. doi:10.1056/NEJM199807303390503. PMID 9696640.
- ↑ 49.0 49.1 Chon T, Nguyen L, Elliott TC (2007). "Clinical inquiries. What are the best treatments for herpes labialis?". J Fam Pract. 56 (7): 576–8. PMID 17605952.
- ↑ Wald A, Carrell D, Remington M, Kexel E, Zeh J, Corey L (2002). "Two-day regimen of acyclovir for treatment of recurrent genital herpes simplex virus type 2 infection". Clin Infect Dis. 34 (7): 944–8. doi:10.1086/339325. PMID 11880960.
- ↑ Spruance SL, Bodsworth N, Resnick H, Conant M, Oeuvray C, Gao J; et al. (2006). "Single-dose, patient-initiated famciclovir: a randomized, double-blind, placebo-controlled trial for episodic treatment of herpes labialis". J Am Acad Dermatol. 55 (1): 47–53. doi:10.1016/j.jaad.2006.02.031. PMID 16781291.
- ↑ Nasser M, Fedorowicz Z, Khoshnevisan MH, Shahiri Tabarestani M (2008). "Acyclovir for treating primary herpetic gingivostomatitis". Cochrane Database Syst Rev (4): CD006700. doi:10.1002/14651858.CD006700.pub2. PMID 18843726.
- ↑ Spruance SL, Rea TL, Thoming C, Tucker R, Saltzman R, Boon R (1997). "Penciclovir cream for the treatment of herpes simplex labialis. A randomized, multicenter, double-blind, placebo-controlled trial. Topical Penciclovir Collaborative Study Group". JAMA. 277 (17): 1374–9. PMID 9134943.
- ↑ Sacks SL, Thisted RA, Jones TM, Barbarash RA, Mikolich DJ, Ruoff GE; et al. (2001). "Clinical efficacy of topical docosanol 10% cream for herpes simplex labialis: A multicenter, randomized, placebo-controlled trial". J Am Acad Dermatol. 45 (2): 222–30. doi:10.1067/mjd.2001.116215. PMID 11464183.
- ↑ Spruance SL, Nett R, Marbury T, Wolff R, Johnson J, Spaulding T (2002). "Acyclovir cream for treatment of herpes simplex labialis: results of two randomized, double-blind, vehicle-controlled, multicenter clinical trials". Antimicrob Agents Chemother. 46 (7): 2238–43. doi:10.1128/AAC.46.7.2238-2243.2002. PMC 127288. PMID 12069980.
- ↑ 56.0 56.1 Amir J, Harel L, Smetana Z, Varsano I (1997). "Treatment of herpes simplex gingivostomatitis with aciclovir in children: a randomised double blind placebo controlled study". BMJ. 314 (7097): 1800–3. doi:10.1136/bmj.314.7097.1800. PMC 2126953. PMID 9224082.
- ↑ "Local anesthetic creams". BMJ. 297 (6661): 1468. 1988. PMC 1835116. PMID 3147021.
- ↑ Hull C, McKeough M, Sebastian K, Kriesel J, Spruance S (2009). "Valacyclovir and topical clobetasol gel for the episodic treatment of herpes labialis: a patient-initiated, double-blind, placebo-controlled pilot trial". J Eur Acad Dermatol Venereol. 23 (3): 263–7. doi:10.1111/j.1468-3083.2008.03047.x. PMID 19143902.
- ↑ Miyatake S, Iyer A, Martuza RL, Rabkin SD (1997). "Transcriptional targeting of herpes simplex virus for cell-specific replication". J Virol. 71 (7): 5124–32. doi:10.1128/JVI.71.7.5124-5132.1997. PMC 191747. PMID 9188579.
- ↑ Davies ME, Bondi JV, Field AK (1984). "Efficacy of 2'-nor-2'-deoxyguanosine treatment for orofacial herpes simplex virus type 1 skin infections in mice". Antimicrob Agents Chemother. 25 (2): 238–41. doi:10.1128/aac.25.2.238. PMC 185481. PMID 6608919.
- ↑ Baker D, Eisen D (2003). "Valacyclovir for prevention of recurrent herpes labialis: 2 double-blind, placebo-controlled studies". Cutis. 71 (3): 239–42. PMID 12661753.
- ↑ Wald A, Langenberg AG, Krantz E, Douglas JM, Handsfield HH, DiCarlo RP; et al. (2005). "The relationship between condom use and herpes simplex virus acquisition". Ann Intern Med. 143 (10): 707–13. doi:10.7326/0003-4819-143-10-200511150-00007. PMID 16287791.
- ↑ Brown ZA, Benedetti J, Ashley R, Burchett S, Selke S, Berry S; et al. (1991). "Neonatal herpes simplex virus infection in relation to asymptomatic maternal infection at the time of labor". N Engl J Med. 324 (18): 1247–52. doi:10.1056/NEJM199105023241804. PMID 1849612.
- ↑ Parra-Sánchez M (2019). "Genital ulcers caused by herpes simplex virus". Enferm Infecc Microbiol Clin (Engl Ed). 37 (4): 260–264. doi:10.1016/j.eimc.2018.10.020. PMID 30580877.