Hepatotoxicity
| Alternative names |
|---|
| Toxic liver disease Toxin induced liver disease |
| Subordinate terms |
| Toxic hepatitis Toxin induced hepatitis |
|
Hepatotoxicity Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hepatotoxicity On the Web |
|
American Roentgen Ray Society Images of Hepatotoxicity |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Toxic liver disease;
Toxin induced liver disease; Drug induced liver disease; Drug induced liver damage; Hepatogenous poisoning
Overview
Hepatotoxicity (from hepatic toxicity) implies chemical-driven liver damage. The liver plays a central role in transforming and clearing chemicals and is susceptible to the toxicity from these agents. Certain medicinal agents when taken in overdoses and sometime even when introduced within therapeutic ranges may injure the organ. Other chemical agents such as those used in laboratories and industries, natural chemicals (e.g. microcystins) and herbal remedies can also induce hepatotoxicity. Chemicals that cause liver injury are called hepatotoxins.
More than 900 drugs have been implicated in causing liver injury[1] and it is the most common reason for a drug to be withdrawn from the market. Chemicals often cause subclinical injury to liver which manifests only as abnormal liver enzyme tests. Drug induced liver injury is responsible for 5% of all hospital admissions and 50% of all acute liver failures.[2][3]
Drug metabolism in liver
The human body identifies almost all drugs as foreign substances (i.e. xenobiotics) and subjects them to various chemical processes (i.e. metabolism) to make them suitable for elimination. This involves chemical transformations to (a) reduce fat solubility and (b) to change biological activity. Although almost all tissue in the body have some ability to metabolize chemicals, smooth endoplasmic reticulum in liver is the principal "metabolic clearing house" for both endogenous chemicals (e.g., cholesterol, steroid hormones, fatty acids, and proteins), and exogenous substances (e.g. drugs).[4] The central role played by liver in the clearance and transformation of chemicals also makes it susceptible to drug induced injury.
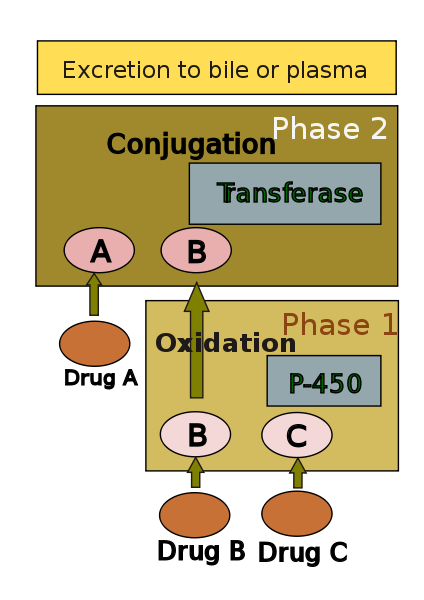
Drug metabolism is usually divided into two phases: phase 1 and phase 2. Phase 1 reaction is thought to prepare a drug for phase 2. However many compounds can be metabolised by phase 2 directly. Phase 1 reaction involves oxidation, reduction, hydrolysis, hydration and many other rare chemical reactions. These processes tend to increase water solubility of the drug and can generate metabolites which are more chemically active and potentially toxic. Most of phase 2 reactions take place in cytosol and involve conjugation with endogenous compounds via transferase enzymes. Chemically active phase 1 products are rendered relatively inert and suitable for elimination by this step.
A group of enzymes located in the endoplasmic reticulum, known as cytochrome P-450, is the most important family of metabolizing enzymes in the liver. Cytochrome P-450 is the terminal oxidase component of an electron transport chain. It is not a single enzyme, rather consists of a family of closely related 50 isoforms, six of them metabolize 90% of drugs.[5][6] There is a tremendous diversity of individual P-450 gene products and this heterogeneity allows the liver to perform oxidation on a vast array of chemicals (including almost all drugs) in phase 1. Three important characteristics of the P450 system have roles in drug induced toxicity:
- 1. Genetic diversity:
Each of the P-450 proteins is unique and accounts to some extent for the variation in drug metabolism between individuals. Genetic variations (polymorphism) in CYP450 metabolism should be considered when patients exhibit unusual sensitivity or resistance to drug effects at normal doses. Such polymorphism is also responsible for variable drug response among patients of differing ethnic backgrounds.
| Potent inducers | Potent inhibitors | Substrates |
|---|---|---|
| Rifampicin, Carbamazepine, Phenobarbital, Phenytoin, (St John's wort), |
Amiodarone, cimetidine, ciprofloxacin, fluconazole, fluoxetine, erythromycin, isoniazid, diltiazem |
Caffeine, clozapine, omeprazole, losartan, theophylline |
- 2. Change in enzyme activity:
Many substances can influence P-450 enzyme mechanism. Drugs interact with the enzyme family in several ways.[9] Drugs that modify Cytochrome P-450 enzyme are referred to as either inhibitors or inducers. Enzyme inhibitors block the metabolic activity of one or several P-450 enzymes. This effect usually occurs immediately. On the other hand inducers increase P-450 activity by increasing its synthesis. Depending on inducing drug's half life, there is usually a delay before enzyme activity increases.[6]
- 3. Competitive inhibition:
Some drugs may share the same P-450 specificity and thus competitively block their bio transformation. This may lead to accumulation of drugs metabolised by the enzyme. This type of drug interaction may also reduce the rate of generation of toxic substrate.
Mechanism of liver damage
| Factors influencing drug induced hepatotoxicity[10] |
|---|
|
Drugs continue to be taken off the market due to late discovery of hepatotoxicity. Due to its unique metabolism and close relationship with the gastrointestinal tract, the liver is susceptible to injury from drugs and other substances. 75% of blood coming to the liver arrives directly from gastrointestinal organs and then spleen via portal veins which bring drugs and xenobiotics in concentrated form. Several mechanisms are responsible for either inducing hepatic injury or worsening the damage process. Many chemicals damage mitochondria, an intracellular organelle that produce energy. Its dysfunction releases excessive amount of oxidants which in turn injures hepatic cells. Activation of some enzymes in the cytochrome P-450 system such as CYP2E1 also lead to oxidative stress.[11] Injury to hepatocyte and bile duct cells lead to accumulation of bile acid inside liver. This promotes further liver damage.[12] Non-parenchymal cells such as Kupffer cells, fat storing stellate cells and leukocytes (i.e. neutrophil and monocyte) also have role in the mechanism.
Adverse drug Reactions
Adverse drug reactions are classified as type A (intrinsic or pharmacological) or type B (idiosyncratic).[13]Type A drug reaction accounts for 80% of all toxicities.[14]
Drugs or toxins that have a pharmacological (type A) hepatotoxicity are those that have predictable dose-response curves (higher concentrations cause more liver damage) and well characterized mechanisms of toxicity such as directly damaging liver tissue or blocking a metabolic process. As in the case of Acetaminophen overdose, this type of injury occurs shortly after some threshold for toxicity is reached.
Idiosyncratic (type B) injury occurs without warning; when agents cause non-predictable hepatotoxicity in susceptible individuals which is not related to dose and has variable latency period.[15] This type of injury does not have a clear dose-response or temporal relationship, and most often do not have predictive models. Idiosyncratic hepatotoxicity has led to the withdrawal of several drugs from market even after rigorous clinical testing as part of the FDA approval process; Troglitazone (Rezulin) and trovafloxacin (Trovan) are two prime examples of idiosyncratic hepatotoxins.
Patterns of injury
| Type of injury: | Hepatocellular | Cholestatic | Mixed |
|---|---|---|---|
| ALT | ≥ Twofold rise | Normal | ≥ Twofold rise |
| ALP | Normal | ≥ Twofold rise | ≥ Twofold rise |
| ALT: ALP ratio | High, ≥5 | Low, ≤2 | 2-5 |
| Examples[16] | Acetaminophen Allopurinol Amiodarone HAART NSAID |
Anabolic steroid Chlorpromazine Clopidogrel Erythromycin Hormonal contraception |
Amitryptyline, Enalapril Carbamazepine Sulphonamide Phenytoin |
Chemicals produce a wide variety of clinical and pathological hepatic injury. Biochemical markers (i.e. alanine transferase, alkaline phosphatase and bilirubin) are often used to indicate liver damage. Liver injury is defined as rise in either (a) ALT level more than three times of upper limit of normal (ULN), (b) ALP level more than twice ULN, or (c) total bilirubin level more than twice ULN when associated with increased ALT or ALP.[17][16] Liver damage is further characterized into hepatocellular (predominantly initial Alanine transferase elevation) and cholestatic (initial alkaline phosphatase rise) types. However they are not mutually exclusive and mixed type of injuries are often encountered.
Specific histo-pathological patterns of liver injury from drug induced damage are discussed below.
Zonal Necrosis
This is the most common type of drug induced liver cell necrosis where the injury is largely confined to a particular zone of the liver lobule. It may manifest as very high level of ALT and severe disturbance of liver function leading to acute liver failure.
In this pattern hepatocellular necrosis is associated with infiltration of inflammatory cells. There can be three types of drug induced hepatitis. (A) viral hepatitis type picture is the commonest, where histological features are similar to acute viral hepatitis. (B) in the focal or non specific hepatitis scattered foci of cell necrosis may accompany lymphocytic infiltrate. (C) chronic hepatitis type is very similar to autoimmune hepatitis clinically, serologically as well as histologically.
- Causes:
- (a) Viral hepatitis like: Halothane, Isoniazid, Phenytoin
- (b) Focal hepatitis: Aspirin
- (c) Chronic hepatitis: Methyldopa, Diclofenac
Liver injury leads to impairment of bile flow and clinical picture is predominated by itching and jaundice. Histology may show inflammation (cholestatic hepatitis) or it can be bland without any parenchymal inflammation. In rare occasions it can produce features similar to primary biliary cirrhosis due to progressive destruction of small bile ducts (Vanishing duct syndrome).
- Causes:
- (a) Bland: Oral contraceptive pills, anabolic steroid, Androgens
- (b) Inflammatory: Allopurinol, Co-amoxiclav, Carbamazepine
- (c) Ductal: Chlorpromazine, flucloxacillin
Hepatotoxicity may manifest as triglyceride accumulation which leads to either small droplet (microvesicular) or large droplet (macrovesicular) fatty liver. There is a separate type of steatosis where phospholipid accumulation leads to a pattern similar to the diseases with inherited phospholipid metabolism defects (e.g. Tay-Sachs disease)
- Causes:
- (a) Microvesicular: Aspirin (Reye's syndrome), Ketoprofen, Tetracycline
- (b) Macrovesicular: Acetamenophen, methotrexate
- (c) Phospholipidosis: Amiodarone, Total parenteral nutrition
Drug induced hepatic granulomas are usually associated with granulomas in other tissues and patients typically have features of systemic vasculitis and hypersensitivity. More than 50 drugs have been implicated.
- Causes:
- Allopurinol, Phenytoin, Isoniazid, Quinine, Penicillin, Quinidine
Vascular lesions
They result from injury to the vascular endothelium.
- Causes:
- Venoocclusive disease: Chemotherapeutic agents, bush tea
- Peliosis hepatis: anabolic steroid
- Hepatic vein thrombosis: Oral contraceptives
Neoplasms have been described with prolonged exposure to some medications or toxins. Hepatocellular carcinoma, angiosarcoma and liver adenomas are the ones usually reported.
Clinical assessment

This remains a major challenge in clinical practice due to lack of reliable markers.[18] Many other conditions lead to similar clinical as well as pathological picture. To diagnose hepatotoxicity, a causal relationship between the use of the toxin or drug and subsequent liver damage has to be established, but might be difficult, especially when idiosyncratic reaction is suspected.[19] Simultaneous use of multiple drugs may add to the complexity. As in acetaminophen toxicity, well established dose dependent pharmacological hepatotoxicity is easier to spot. Several clinical scales such as CIOMS/RUCAM scale and Maria and Victorino criteria have been proposed to establish causal relationship between offending drug and liver damage. CIOMS/RUCAM scale involves a scoring system which categorizes the suspicion into "definite or highly probable" (score > 8), “probable” (score 6-8), “possible” (score 3-5), “unlikely” (score 1-2) and “excluded” (score ≤ 0). In clinical practice physicians put more emphasis on the presence or absence of similarity between the biochemical profile of the patient and known biochemical profile of the suspected toxicity ( e.g. cholestatic damage in amoxycillin-clauvonic acid ).[18]
Treatment and prognosis
In most cases liver function will return to normality if offending drug is stopped early. However in acetamenophen toxicity initial insult can be fatal. In most instances supportive treatment is all that is required. However in fulminant hepatic failure from drug induced hepatotoxicity may require liver transplantation. In the past glucocorticoides in allergic features and ursodeoxycholic acid in cholestatic pictures had been used, but there is no good evidence to support their effectiveness.
An elevation in serum bilirubin level of more that 2 times ULN with associated transaminase rise is an ominous sign. This indicates severe hepatotoxicity and is likely to lead to mortality in 10% to 15% of patients, especially if the offending drug is not stopped (Hy's Law).[20][21] This is due to the fact that it requires significant damage to the liver to impair bilirubin excretion, hence minor impairment (in the absence of biliary obstruction or Gilbert syndrome) would not lead to jaundice. Other poor predictors of outcome are old age, female sex, high AST.[22][23]
Drugs withdrawn for hepatotoxicity
Troglitazone, bromfenac, trovafloxacin, ebrotidine, nimesulide, nefazodone and ximelagatran.[18][24]
Specific drug or toxin
Acetaminophen

Acetaminophen (paracetamol, also known by the brand name Tylenol and Panadol) is usually well tolerated in prescribed dose but overdose is the most common cause of drug induced liver disease and acute liver failure worldwide,[10] which is one of the most painful experiences patients report. Reports of death from accute hepatotoxicity have been reported to be as low as 2.5 grams over a 24 hour period. Damage to the liver is not due to the drug itself but to a toxic metabolite (N-acetyl-p-benzoquinone imine NAPQI, or NABQI) which is produced by cytochrome P450 enzymes in the liver.[25] In normal circumstances this metabolite is detoxified by conjugating with glutathione in phase 2 reaction. In overdose large amount of NAPQI is generated which overwhelm the detoxification process and lead to damage to liver cells. Nitric oxide also plays role in inducing toxicity.[26] The risk of liver injury is influenced by several factors including the dose ingested, concurrent alcohol or other drug intake, interval between ingestion and antidote etc. The dose toxic to liver is quite variable and is lower in chronic alcoholics. Measurement of blood level is important in assessing prognosis, higher level predicting worse prognosis. Administration of Acetylcysteine, a precursor of glutathione, can limit the severity of the liver damage by capturing the toxic NAPQI. Those who develop acute liver failure can still recover spontaneously, but may require transplantation if poor prognostic signs such as encephalopathy or coagulopathy is present (see King's College Criteria).
Nonsteroidal anti-inflammatory drugs
Although individual analgesics rarely induce liver damage, due to their widespread use NSAIDs have emerged as a major group of drugs exhibiting hepatotoxicity. Both dose dependent and idiosyncratic reactions have been documented.[27] Aspirin and phenylbutazone are associated with intrinsic hepatotoxicity; idiosyncratic reaction has been associated with ibuprofen, sulindac, phenylbutazone, piroxicam, diclofenac and indomethacin.
Glucocorticoids
Glucocorticoids are so named due to their effect on carbohydrate mechanism. they promote glycogen storage in liver. Enlarged liver is a rare side effect of long term steroid use in children.[28] The classical effect of prolonged use both in adult and paediatric population is steatosis.[29]
Isoniazid
Isoniazide (INH) is one of the most commonly used drug for tuberculosis; it is associated with mild elevation of liver enzymes in up to 20% of patients and severe hepatotoxicity in 1-2% of patients.[30]
Natural products
Example: Amanita mushroom, particularly the destroying angels, aflatoxins
Industrial toxin
Example: Arsenic, Carbon tetraChloride, Vinyl Chloride
Herbal and alternative remedies
Ackee fruit, Bajiaolian, Camphor, Copaltra, Cycasin, Kava, Pyrrolizidine alkaloids, Horse chestnut leaf, Valerian, Comfrey (often used in herbal tea)[31]
- Chinese herbal remedies:
- Jin Bu Huan, Ma-huang, Sho-wu-pian
-
Fly agaric (Amanita muscaria) is one of the natural products toxic to the liver
-
Horse chestnut leaf
-
Ackee fruit
-
Saint John's wort Induces Cytochrome P-450 enzyme
See also
References
- ↑ Friedman, Scott E.; Grendell, James H.; McQuaid, Kenneth R. (2003). Current diagnosis & treatment in gastroenterology. New York: Lang Medical Books/McGraw-Hill. pp. p664–679. ISBN 0-8385-1551-7.
- ↑ McNally, Peter F. GI/Liver Secrets: with STUDENT CONSULT Access. Saint Louis: C.V. Mosby. ISBN 1-56053-618-7.
- ↑ Ostapowicz G, Fontana RJ, Schiødt FV; et al. (2002). "Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States". Ann. Intern. Med. 137 (12): 947–54. PMID 12484709.
- ↑ Donald Blumenthal; Laurence Brunton; Keith Parker; Lazo, John S.; Iain Buxton. Goodman and Gilman's Pharmacological Basis of Therapeutics Digital Edition. McGraw-Hill Professional. ISBN 0-07-146804-8.
- ↑ Skett, Paul; Gibson, G. Gordon (2001). Introduction to drug metabolism. Cheltenham, UK: Nelson Thornes Publishers. ISBN 0-7487-6011-3.
- ↑ 6.0 6.1 6.2 Lynch T, Price A (2007). "The effect of cytochrome P450 metabolism on drug response, interactions, and adverse effects". American family physician. 76 (3): 391–6. PMID 17708140.
- ↑ Jessica R. Oesterheld; Kelly L. Cozza; Armstrong, Scott. Concise Guide to Drug Interaction Principles for Medical Practice: Cytochrome P450s, Ugts, P-Glycoproteins. Washington, DC: American Psychiatric Association. pp. 167–396. ISBN 1-58562-111-0.
- ↑ "P450 Table". Retrieved 2007-09-29.
- ↑ Michalets EL (1998). "Update: clinically significant cytochrome P-450 drug interactions". Pharmacotherapy. 18 (1): 84–112. PMID 9469685.
- ↑ 10.0 10.1 Keeffe, Emmet B; Friedman, Lawrence M. (2004). Handbook of liver diseases. Edinburgh: Churchill Livingstone. pp. 104–123. ISBN 0-443-06633-7.
|access-date=requires|url=(help) - ↑ Jaeschke H, Gores GJ, Cederbaum AI, Hinson JA, Pessayre D, Lemasters JJ (2002). "Mechanisms of hepatotoxicity". Toxicol. Sci. 65 (2): 166–76. doi:10.1093/toxsci/65.2.166. PMID 11812920.
- ↑ Patel T, Roberts LR, Jones BA, Gores GJ (1998). "Dysregulation of apoptosis as a mechanism of liver disease: an overview". Semin. Liver Dis. 18 (2): 105–14. PMID 9606808.
- ↑ Davies, D. (1985). Textbook of adverse drug reactions. Oxford [Oxfordshire]: Oxford University Press. pp. 18–45. ISBN 0-19-261479-7. OCLC 12558288.
- ↑ Pirmohamed M, Breckenridge AM, Kitteringham NR, Park BK (1998). "Adverse drug reactions". BMJ. 316 (7140): 1295–8. PMID 9554902.
- ↑ Zimmerman HJ (1978). "Drug-induced liver disease". Drugs. 16 (1): 25–45. doi:10.2165/00003495-197816010-00002. PMID 352664.
- ↑ 16.0 16.1 Mumoli N, Cei M, Cosimi A (2006). "Drug-related hepatotoxicity". N. Engl. J. Med. 354 (20): 2191–3, author reply 2191-3. PMID 16710915.
- ↑ Bénichou C (1990). "Criteria of drug-induced liver disorders. Report of an international consensus meeting". J. Hepatol. 11 (2): 272–6. PMID 2254635.
- ↑ 18.0 18.1 18.2 Andrade RJ, Robles M, Fernández-Castañer A, López-Ortega S, López-Vega MC, Lucena MI (2007). "Assessment of drug-induced hepatotoxicity in clinical practice: a challenge for gastroenterologists". World J. Gastroenterol. 13 (3): 329–40. PMID 17230599.
- ↑ Arundel C, Lewis JH (2007). "Drug-induced liver disease in 2006". Curr. Opin. Gastroenterol. 23 (3): 244–54. doi:10.1097/MOG.0b013e3280b17dfb. PMID 17414839.
- ↑ Reuben A (2004). "Hy's law". Hepatology. 39 (2): 574–8. doi:10.1002/hep.20081. PMID 14768020.
- ↑ Arora N, Goldhaber SZ (2006). "Anticoagulants and transaminase elevation". Circulation. 113 (15): e698–702. doi:10.1161/CIRCULATIONAHA.105.603100. PMID 16618822.
- ↑ Andrade RJ, Lucena MI, Kaplowitz N; et al. (2006). "Outcome of acute idiosyncratic drug-induced liver injury: Long-term follow-up in a hepatotoxicity registry". Hepatology. 44 (6): 1581–8. doi:10.1002/hep.21424. PMID 17133470.
- ↑ Björnsson E, Olsson R (2005). "Outcome and prognostic markers in severe drug-induced liver disease". Hepatology. 42 (2): 481–9. doi:10.1002/hep.20800. PMID 16025496.
- ↑ Shah RR (1999). "Drug-induced hepatotoxicity: pharmacokinetic perspectives and strategies for risk reduction". Adverse drug reactions and toxicological reviews. 18 (4): 181–233. PMID 10687025.
- ↑ Wallace JL (2004). "Acetaminophen hepatotoxicity: NO to the rescue". Br. J. Pharmacol. 143 (1): 1–2. doi:10.1038/sj.bjp.0705781. PMID 15345657.
- ↑ James LP, Mayeux PR, Hinson JA (2003). "Acetaminophen-induced hepatotoxicity". Drug Metab. Dispos. 31 (12): 1499–506. doi:10.1124/dmd.31.12.1499. PMID 14625346.
- ↑ Manov I, Motanis H, Frumin I, Iancu TC (2006). "Hepatotoxicity of anti-inflammatory and analgesic drugs: ultrastructural aspects". Acta Pharmacol. Sin. 27 (3): 259–72. doi:10.1111/j.1745-7254.2006.00278.x. PMID 16490160.
- ↑ Iancu TC, Shiloh H, Dembo L (1986). "Hepatomegaly following short-term high-dose steroid therapy". J. Pediatr. Gastroenterol. Nutr. 5 (1): 41–6. PMID 3944744.
- ↑
Alpers DH, Sabesin SM (1982). Diseases of the liver. Philadelphia: JB Lippincott. pp. 813–45. Unknown parameter
|coauthors=ignored (help) - ↑ Sarich TC, Adams SP, Petricca G, Wright JM (1999). "Inhibition of isoniazid-induced hepatotoxicity in rabbits by pretreatment with an amidase inhibitor". J. Pharmacol. Exp. Ther. 289 (2): 695–702. PMID 10215642.
- ↑ Pak E, Esrason KT, Wu VH (2004). "Hepatotoxicity of herbal remedies: an emerging dilemma". Progress in transplantation (Aliso Viejo, Calif.). 14 (2): 91–6. PMID 15264453.



