|
|
| (48 intermediate revisions by 11 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| | {| class="infobox" style="float:right;" |
| | |- |
| | | [[File:Siren.gif|30px|link= Congestive heart failure resident survival guide]]|| <br> || <br> |
| | | [[Acute decompensated heart failure resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] |
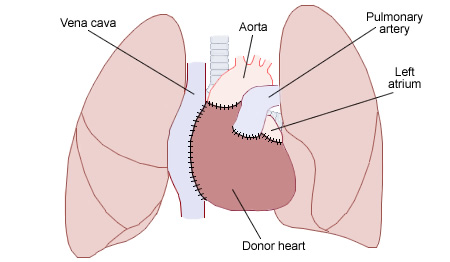
| | |} |
| [[Image:Heart transplant.jpg|thumb|right|200px|(Diagram illustrating the placement of a donor [[heart]] in an '''orthotopic procedure'''. Notice how the back of the patient's [[left atrium]] and [[great vessels]] are left in place).]] | | [[Image:Heart transplant.jpg|thumb|right|200px|(Diagram illustrating the placement of a donor [[heart]] in an '''orthotopic procedure'''. Notice how the back of the patient's [[left atrium]] and [[great vessels]] are left in place).]] |
| {{SI}} | | {{Heart transplantation}} |
| | | '''For patient information, click [[Heart transplantation (patient information)|here]] |
| '''Editors-in-Chief:''' [[C. Michael Gibson, M.S., M.D.]]; Juan A. Sanchez MD MPA [mailto:Juan.Sanchez@stmh.org], Chairman, The Stanley J. Dudrick Department of Surgery, Saint Mary's Hospital, Waterbury, CT | |
| __NOTOC__
| |
| '''Associate Editor-In-Chief:''' {{CZ}}
| |
| | |
| {{Editor Join}}
| |
| ==Overview==
| |
| | |
| '''Heart transplantation''' or '''cardiac transplantation''', is a surgical [[organ transplant|transplant]] procedure performed on patients with end-stage [[heart failure]] or severe [[coronary artery disease]]. The most common procedure is to take a working [[heart]] from a recently deceased organ donor ([[allograft]]) and implant it into the patient. The patient's own heart may either be removed ([[heart transplantation#Orthotopic procedure|orthotopic procedure]]) or, less commonly, left in to support the donor heart ([[heart transplantation#Heterotopic procedure|heterotopic procedure]]). It is also possible to take a heart from another species ([[xenograft]]), or implant a man-made [[artificial heart|artificial one]], although the outcome of these two procedures has been less successful in comparison to the far more commonly performed [[allograft]]s.
| |
| | |
| ==History==
| |
| | |
| The first heart transplanted into a human occurred in 1964 at the University of Mississippi Medical Center in Jackson, Mississippi when a team led by Dr. James Hardy transplanted a chimpanzee heart into a dying patient. The heart beat 90 minutes before stopping. Dr. James Hardy had performed the first human [[lung transplant]] the previous year. <ref>http://www.umc.edu/hardy/</ref>
| |
| | |
| The first human to human heart transplant was performed by Professor [[Christiaan Barnard]] at Groote Schuur Hospital in December 1967. The patient was a Louis Washkansky of Cape Town, South Africa, who lived for 18 days after the procedure before dying of [[pneumonia]]. The donor was Denise Darvall, who was rendered [[Brain death|brain dead]] in a car accident.
| |
| | |
| The first successful United States heart transplant was done at St. Lukes hospital in Houston Texas by Denton Cooley, M. D. in June 1968. The donor was a teenage suicide victim (who had had an aortic coarctation repaired as a young child, also by Dr. Cooley) and the recipient, Mr. Thomas, had terminal severe [[cardiomyopathy]]. He survived 8 months before dying of rejection of the transplanted heart.
| |
| | |
| A series of five subsequent heart transplants was done that month by Dr. Cooley followed by a number of transplants in Houston that year before the program was canceled leaving only Norman Shumway at Stanford University at San Francisco doing heart transplants and research on the rejection phenomenon.
| |
| | |
| 1970 - Recipient selection criteria standardized
| |
| | |
| 1973 - Surveillance [[endocardial biopsy]]
| |
| | |
| 1977 - Distant donor heart procurement
| |
| | |
| 1980 - Cyclosporine A
| |
| | |
| ==Statistics==
| |
| Reporting of transplant statistics to the Registry of the International Society for Heart and Lung Transplantation (ISHLT) is required in the US, but not other countries. According to ISHLT:
| |
| *5000 heart transplants are performed per year worldwide
| |
| *10-20 heart transplants per year are performed at each center
| |
| *50-59 years is the average age of heart transplant recipients
| |
| *10:1 is the ratio of awaiting recipients to donors
| |
| *207 hospitals performed heart transplants in 207
| |
| *51% of heart transplants are performed for non-ischemic [[cardiomyopathy]] and 38% are performed for ischemic heart disease <ref>Taylor, DO, Stehlik, J, Edwards, LB, et al. Registry of the international society for heart and lung transplantation: twenty-sixth official adult heart transplant report-2009. J Heart Lung Transplant 2009; 28:1007.</ref>
| |
| | |
| ==Indications==
| |
| In order for a patient to be recommended for a heart transplant they will generally have advanced, irreversible [[heart failure]] with a severely limited [[life expectancy]].<ref name="pmid11397947">{{cite journal |author=Steinman TI, Becker BN, Frost AE, Olthoff KM, Smart FW, Suki WN, Wilkinson AH |title=Guidelines for the referral and management of patients eligible for solid organ transplantation |journal=[[Transplantation]] |volume=71 |issue=9 |pages=1189–204 |year=2001 |month=May |pmid=11397947 |doi= |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0041-1337&volume=71&issue=9&spage=1189 |issn=}}</ref><ref>Mehra, MR, Kobashigawa, J, Starling, R, et al. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates--2006. J Heart Lung Transplant 2006; 25:1024.</ref> It is important to note that the life expectancy of [[heart failure]] has improved over the past two decades due to improvements in both medical therapy ([[ACE Inhibition]], [[beta-blockers]], [[aldosterone antagonists]] and device therapy such as [[automatic implantable cardiac defibrillator]]s [[AICD]]s and [[cardiac resynchronization]]. Thus, patients should not be considered for cardiac transplantation unless they have failed aggressive medical and device therapy <ref>Mehra, MR, Kobashigawa, J, Starling, R, et al. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates--2006. J Heart Lung Transplant 2006; 25:1024.</ref>.
| |
| | |
| ===Systolic [[heart failure]] with a left ventricular ejection fraction < 35%===
| |
| Due to either:
| |
| :*Ischemic [[cardiomyopathy]]
| |
| :*Dilated [[cardiomyopathy]]
| |
| :*[[Valvular heart disease]]
| |
| :*[[Hypertensive heart disease]]
| |
| :*Etiologies which are excluded are [[amyloid]], [[HIV]], and cardiac [[sarcoma]]
| |
| ===Ischemic coronary artery disease with refractory angina===
| |
| Ischemia which is not amenable to [[coronary artery bypass graft surgery]] (CABG) and is refractory to maximally tolerated medical therapy
| |
| ===Intractable life-threatening arrhythmias===
| |
| :*Arrhythmias which are not controlled by an implantable cardioverter-defibrillator
| |
| :*Arrhythmias that are refractory or not amenable to electrophysiologic guided single or combination medical therapy
| |
| :* Patients that are not a candidate for ablative therapy
| |
| | |
| ===Hypertrophic obstructive cardiomyopathy (HOCM)===
| |
| [[Class IV heart failure]] symptoms persist despite maximal therapy, myomectomy, alcohol septal ablation, mitral valve replacement
| |
| | |
| ===Congenital heart disease===
| |
| :*Fixed [[pulmonary hypertension]] must not be present
| |
| | |
| ===Additional Considerations===
| |
| :*The patient should have a stable psychosocial situation
| |
| | |
| ==Contraindications==
| |
| ===Underlying myocardial disease===
| |
| Underlying etiologies of myocardial disease which are contraindications are:
| |
| *[[Amyloid]]
| |
| *[[HIV]]
| |
| *Cardiac [[sarcoma]].
| |
| ===Co-morbid or associated conditions===
| |
| Some patients are less suitable for a heart transplant, especially if they suffer from other circulatory conditions unrelated to the heart. The following conditions in a patient would increase the chances of [[complication (medicine)|complications]] occurring during the operation:
| |
| *[[Kidney]], [[lung]], or [[liver]] disease
| |
| *Insulin-dependent [[diabetes]] with other organ dysfunction
| |
| *Life-threatening diseases unrelated to [[heart failure]] such as cancer that would severely limit life expectancy
| |
| *[[Vascular disease]] of the neck and leg arteries.
| |
| *No ongoing acute infections
| |
| *No recurrent pulmonary infections
| |
| *No alcohol, tobacco or drug abuse
| |
| *Severe lung disease such as [[chronic obstructive pulmonary disease]]
| |
| *Morbid obesity
| |
| *[[ABO]] incompatibility
| |
| | |
| ==Donor Criteria==
| |
| | |
| #[[Brain death]] declared
| |
| #Age <45 (special exceptions)
| |
| #No pre-existent heart disease
| |
| #Few [[coronary artery disease]] risk factors
| |
| #No untreated acute infections
| |
| #No systemic malignancy
| |
| #No cardiac trauma
| |
| #Normal [[ECG]]
| |
| #Normal echocardiogram
| |
| #Negative [[HIV]] and [[Hepatitis]] screen
| |
| | |
| ==Equitable Distribution of Donor Hearts to those Awaiting Transplantation and the Process of Being Listed for a Transplant==
| |
| In order to assure that access to donor hearts is equitably distributed, the United Network for Organ Sharing (UNOS), was created. In general, patients who are hospitalized and require ongoing administration of parenteral [[inotropic]] agents are at highest risk of death, and are placed at the highest priority on the list of potential recipients. The following factors are used in assigning the priority for transplantation:
| |
| *The level of acuity of the patient's condition (sicker patients are higher on the list)
| |
| *The time the patient has waited on the list (patients who have waited longer are higher on the list)
| |
| *Duration of ischemic time anticipated when a donor heart does become available (assessed in increments of 500 miles between donor and recipient hospitals)(patients who are located closer to the donor heart are higher on the list)
| |
| | |
| Some patients may be moved down the list or they may be taken off of the list (delisted). About 5% of patients are delisted because they improve with medical therapy. The prognosis of patients who have been delisted is controversial. The largest study to date of 100 patients indicates that delisted patients may have a slightly poorer long-term prognosis than those patients who are transplanted. <ref name="pmid18455599">{{cite journal |author=Hoercher KJ, Nowicki ER, Blackstone EH, Singh G, Alster JM, Gonzalez-Stawinski GV, Starling RC, Young JB, Smedira NG |title=Prognosis of patients removed from a transplant waiting list for medical improvement: implications for organ allocation and transplantation for status 2 patients |journal=[[The Journal of Thoracic and Cardiovascular Surgery]] |volume=135 |issue=5 |pages=1159–66 |year=2008 |month=May |pmid=18455599 |doi=10.1016/j.jtcvs.2008.01.017 |url=http://linkinghub.elsevier.com/retrieve/pii/S0022-5223(08)00168-2 |issn=}}</ref> While early survival was better among those patients who were delisted, survival after 30 months tended to be better among patients who were transplanted. Among delisted patients, the mean duration of survival was 7.7 years, and 94%, 55% and 28% of patients were event-free at 1, 5, and 10 years respectively. Although data is lacking, it has been hypothesized that survival could be further improved among delisted patients to 45% at 10 years if a [[defibrillator]] or [[AICD]] was implanted.
| |
| | |
| The predictors of death within two months of being placed on a transplant list among status 1 candidates include <ref>Lietz, K, Miller, LW. Improved survival of patients with end-stage heart failure listed for heart transplantation: analysis of organ procurement and transplantation network/U.S. United Network of Organ Sharing data, 1990 to 2005. J Am Coll Cardiol 2007; 50:1282.</ref>:
| |
| #[[Inotropic]] and [[intra-aortic balloon pump]] support
| |
| #[[Pulmonary capillary wedge pressure]] >20 mm Hg
| |
| # UNOS status 1A
| |
| #[[Mechanical ventilation]]
| |
| #Serum [[creatinine]] >1.5 mg/dl
| |
| #Failed cardiac transplant
| |
| #Valvular [[cardiomyopathy]]
| |
| #Age >60 years
| |
| #Caucasian ethnicity
| |
| #Weight ≤70 kg
| |
| #Lack of an [[AICD]] on the day of listing
| |
| | |
| The mortality among children and young adults < 18 years of age who are awaiting transplant was 17% between 1999 and 2006 and is higher than adults. The majority of the deaths occurred in those children who weighed 10-15 Kg.
| |
| | |
| ==Criteria for Cardiac Transplantation==
| |
| While assessment of the indications and contraindications are important first steps in evaluating the appropriateness for cardiac transplantation, the prognosis of a patient with and without transplantation is critical in making the final determination as to whether a patient is suitable for cardiac transplantation. Discussed below are criteria that are used based upon the estimation of the patient's prognosis.
| |
| | |
| ===Functional Capacity and Peak V02 (V02 Max)===
| |
| This objective metric is listed by the ACC/AHA heart failure guidelines as a critical measure in determining when to list someone for transplantation <ref>Gibbons, RJ, Balady, GJ, Bricker, JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation 2002; 106:1883.</ref><ref>Hunt, SA, Abraham, WT, Chin, MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation 2009; 119:e391.</ref>. A normal peak V02 is > 20 ml/kg/min. Older data from 1986 through 1989 identified and peak V02 of 14 ml/kg/min as a threshold for listing a patient <ref name="pmid1999029">{{cite journal |author=Mancini DM, Eisen H, Kussmaul W, Mull R, Edmunds LH, Wilson JR |title=Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure |journal=[[Circulation]] |volume=83 |issue=3 |pages=778–86 |year=1991 |month=March |pmid=1999029 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=1999029}}</ref>. Those patients with a peak V02 > 14 ml/kg/min who were considered too stable for cardiac transplantation had a survival that was similar to that of patients with a peak V02 <u><</u> 14 ml/kg/min who were transplanted. It should be noted that peak V02 is variable, and should be re assessed periodically. It should also be noted that gender, age, comorbidities, and a patient's level of conditioning should be taken into account when interpreting the peak V02. If a patient is consistently in the peak V02 range of 10-12 ml/kg/min, then transplantation should be considered.
| |
| | |
| ===ACC / AHA Transplant Criteria===
| |
| The ACC / AHA criteria are as follows <ref>Hunt, SA, Abraham, WT, Chin, MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation 2009; 119:e391.</ref>:
| |
| ====Absolute Indications====
| |
| *For hemodynamic compromise due to severe [[heart failure]]
| |
| :*Refractory [[cardiogenic shock]]
| |
| :*Documented dependence on intravenous [[inotropic]] support to maintain adequate organ perfusion
| |
| :*[[Peak VO2]] less than 10 mL/kg per min with achievement of anaerobic metabolism
| |
| *Severe symptoms of ischemia that consistently limit routine activity and are not amenable to [[coronary artery bypass surgery]] or percutaneous coronary intervention.
| |
| *Recurrent symptomatic ventricular arrhythmias refractory to all therapeutic modalities
| |
| | |
| ====Relative indications====
| |
| | |
| #Peak V02 of 11 to 14 mL/kg per minute (or 55 percent predicted) and major limitation of the patient's daily activities
| |
| #Recurrent unstable ischemia not amenable to other intervention
| |
| #Recurrent instability of fluid balance/renal function not due to patient noncompliance with medical regimen
| |
| | |
| ===="Insufficient" indications====
| |
| #Low left ventricular ejection fraction
| |
| #History of functional class II or IV symptoms of HF
| |
| #Peak [[VO2]] greater than 15 mL/kg per minute (or greater than 55 percent predicted) without other indications
| |
| | |
| ==Surgical Procedure==
| |
| ===Pre-operative===
| |
| A typical heart transplantation begins with a suitable donor heart being located from a recently deceased or brain dead donor. The transplant patient is contacted by a [[nurse]] coordinator and instructed to attend the hospital in order to be evaluated for the operation and given pre-surgical medication. At the same time, the heart is removed from the donor and inspected by a team of surgeons to see if it is in a suitable condition to be transplanted. Occasionally it will be deemed unsuitable. This can often be a very distressing experience for an already emotionally unstable patient, and they will usually require emotional support before being sent home.
| |
| | |
| ===Operative===
| |
| Once the donor heart has passed its inspection, the patient is taken into the [[operating theatre]] and given a [[general anesthetic]]. Either an '''orthotopic''' or a '''heterotopic''' procedure is followed, depending on the condition of the patient and the donor heart.
| |
| | |
| ====Orthotopic procedure====
| |
| The '''orthotopic procedure''' begins with the surgeons performing a [[median sternotomy]] to expose the [[mediastinum]]. The [[pericardium]] is opened, the [[great vessels]] are dissected and patient is attached to [[cardiopulmonary bypass]]. The failing heart is removed by transecting the great vessels and a portion of the [[left atrium]]. The [[pulmonary vein]]s are not transected; rather a circular portion of the left atrium containing the pulmonary veins is left in place. The donor heart is trimmed to fit onto the patients remaining left atrium and great vessels and [[suture]]d in place. The new heart is restarted, the patient is weaned from cardiopulmonary bypass and the chest cavity is closed.
| |
| | |
| ====Heterotopic procedure====
| |
| In the '''heterotopic procedure''', the patient's own heart is not removed before implanting the donor heart. The new heart is positioned so that the chambers and blood vessels of both hearts can be connected to form what is effectively a 'double heart'. The procedure can give the patients original heart a chance to recover, and if the donor's heart happens to fail (eg. through rejection), it may be removed, allowing the patients original heart to start working again. Heterotopic procedures are only used in cases where the donor heart is not strong enough to function by itself (due to either the patients body being considerably larger than the donor's, the donor having a weak heart, or the patient suffering from [[pulmonary hypertension]]).
| |
|
| |
|
| ===Post-operative===
| | '''Editor(s)-in-Chief:''' [[C. Michael Gibson, M.S., M.D.]]; '''Associate Editor-In-Chief:''' {{CZ}}; {{IF}} |
| The patient is taken into [[Intensive care unit|ICU]] to recover. When they wake up, they will be transferred to a special recovery unit in order to be [[Physical medicine and rehabilitation|rehabilitated]]. How long they remain in hospital post-transplant depends on the patient's general health, how well the new heart is working, and their ability to look after their new heart. Once the patient is released, they will have to return to the hospital for regular check-ups and rehabilitation sessions. They may also require emotional support. The number of visits to the hospital will decrease over time, as the patient adjusts to their transplant. The patient will have to remain on lifetime [[immunosuppressant]] medication to avoid the possibility of [[transplant rejection|rejection]]. Since the [[vagus nerve]] is severed during the operation, the new heart will beat at around 100 bpm until nerve regrowth occurs.
| |
|
| |
|
| =="Living organ" transplant==
| | {{SK}} Cardiac transplantation; Heart grafting |
| Doctors made medical history in February 2006, at Bad Oeynhausen Clinic for Thorax and Cardiovascular Surgery, Germany, when they successfully transplanted a 'beating heart' into a patient.<ref>{{cite news | author= | title=Bad Oeynhausen Clinic for Thorax- and Cardiovascular Surgery Announces First Successful Beating Human Heart Transplant | url=http://www.transmedics.com/wt/page/pr_1140714229 | date=23 February 2006 | publisher=TransMedics | accessdate=2007-05-14}}</ref>
| |
| Normally, [[potassium chloride]] injected donor's heart (in order to stop it beating, before being removed from the body) packed in ice in to preserve it. The ice can usually keep the heart fresh for up to four to six hours, depending on its condition to start with. Rather than cooling the heart, this new procedure involves keeping it at [[body temperature]] and hooking it up to a special machine called an [[Organ care system|Organ Care System]] that allows it to continue beating with warm, oxygenated blood flowing through it. This can maintain the heart in a suitable condition for much longer than the traditional method.
| |
|
| |
|
| ==Immunosuppressive Therapy== | | ==[[Heart transplantation overview|Overview]]== |
|
| |
|
| A. Cyclosporine A
| | ==[[Heart transplantation historical perspective|Historical Perspective]]== |
|
| |
|
| B. Adrenocortical steroids
| | ==[[Heart transplantation classification|Classification]]== |
|
| |
|
| C. Azathioprine
| | ==[[Heart transplantation pathophysiology|Pathophysiology]]== |
|
| |
|
| D. OKT3
| | ==[[Heart transplantation causes|Causes]]== |
|
| |
|
| E. Anti-thymocyte globulin (ATG)
| | ==[[Heart transplantation epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| ==EKG Findings Following Transplantation== | | ==[[Heart transplantation risk factors|Risk Factors]]== |
|
| |
|
| [[Image:Transplant.jpg|400px|thumb|center|12 lead EKG shows accessory atrial activity (better seen in lead II at the end of the first complex in the middle between the second and third complex and after the third complex) due to some of the original sinus node still remains in addition to the donor sinus node after a cardiac transplant. Because of a suture line in the right atrium the ectopic atrial rhythm rarely conducts to the AV node. Right axis deviation and a rSR' which might suggest volume overload RVH also shown.]] | | ==[[Heart transplantation screening|Screening]]== |
|
| |
|
| ==Prognosis== | | ==[[Heart transplantation prognosis|Prognosis]]== |
| After the first 6 months, the mortality rates is approximately 3.5% per year. The prognosis for heart transplant patients following the orthotopic procedure has greatly increased over the past 20 years, and as of Aug. 11, 2006, the survival rates were as follows.<ref>[http://www.americanheart.org/presenter.jhtml?identifier=4588 Heart Transplants: Statistics] ''The [[American Heart Association]]''. Retrieved February 1, 2007.</ref>
| |
|
| |
|
| * 1 year: 86.1% (males), 83.9% (females)
| | ==Diagnosis== |
| * 3 years: 78.3% (males), 74.9% (females)
| | There is no single diagnostic study of choice. A thorough evaluation should be done- including a physical examination and appropriate imaging to select the patients for a heart transplant. The indications and criteria should be fulfilled; the contraindications should be looked out for. |
| * 5 years: 71.2% (males), 66.9% (females)
| |
|
| |
|
| The "half-life" of patient survival has likewise improved as follows <ref>Taylor, DO, Stehlik, J, Edwards, LB, et al. Registry of the international society for heart and lung transplantation: twenty-sixth official adult heart transplant report-2009. J Heart Lung Transplant 2009; 28:1007.</ref>:
| | ====[[Heart transplantation indications|Indications]]==== |
|
| |
|
| *1982-1991: 8.9 years
| | ====[[Heart transplantation contraindications|Contraindications]]==== |
| *1992-2001: 10.5 years
| |
| *2002-2007: 11.0 years
| |
|
| |
|
| As of 2006, Tony Huesman is the world's longest living heart transplant patient, having survived for 28 years with a transplanted heart. Huesman received a heart in 1978 at the age of 20 after [[viral pneumonia]] severely weakened his heart. The operation was performed at Stanford University under American heart transplant pioneer [[Norman Shumway|Dr. Norman Shumway]], who continued to perform the operation in the U.S. after others abandoned it due to poor results. <ref>[http://www.cbsnews.com/stories/2006/09/14/ap/health/mainD8K49NG86.shtml Heart Transplant Patient OK After 28 Yrs] (September 14, 2006) ''CBS News''. Retrieved December 29, 2006.</ref>
| | ====[[Heart transplantation criteria|Criteria for Cardiac Transplantation]]==== |
|
| |
|
| ==Causes of Death after Transplantation== | | ====[[Heart transplantation equitable distribution of donor hearts|Equitable Distribution of Donor Hearts to those Awaiting Transplantation and the Process of Being Listed for a Transplant]]==== |
|
| |
|
| *Rejection
| | ==Treatment== |
| *Infection
| | ====[[Heart transplantation immunosuppressive therapy|Medical Therapy]]==== |
| *Technical problems
| |
| *CNS events
| |
| *Malignancy
| |
|
| |
|
| | ====[[Heart transplantation surgical procedure|Surgery]]==== |
|
| |
|
| | ==Follow-Up== |
| | ====[[Heart transplantation associated arrhythmias|Arrhythmias after transplantation]]==== |
| | ====[[Heart transplantation electrocardiogram and pacing after cardiac transplantation|Electrocardiogram and Pacing After Cardiac Transplantation]]==== |
|
| |
|
| ==ACC / AHA Guidelines- Recommendations for Pacing After Cardiac Transplantation (DO NOT EDIT) <ref name="Epstein"> Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation. 2008; 117: 2820–2840. PMID 18483207 </ref>== | | ==Related Chapters== |
| {{cquote|
| | * [[Congestive heart failure]] |
| ===Class I===
| |
| 1. Permanent [[pacemaker|pacing]] is indicated for persistent inappropriate or symptomatic [[bradycardia]] not expected to resolve and for other Class I indications for permanent [[pacemaker|pacing]]. ''(Level of Evidence: C)''
| |
|
| |
|
| ===Class IIb===
| |
| 1. Permanent [[pacemaker|pacing]] may be considered when relative [[bradycardia]] is prolonged or recurrent, which limits rehabilitation or discharge after postoperative recovery from [[cardiac transplantation]]. ''(Level of Evidence: C)''
| |
|
| |
| 2. Permanent [[pacemaker|pacing]] may be considered for [[syncope]] after [[cardiac transplantation]] even when [[bradyarrhythmia]] has not been documented. ''(Level of Evidence: C)''}}
| |
|
| |
| ==Sources==
| |
| * The ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities <ref name="Epstein"> Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation. 2008; 117: 2820–2840. PMID 18483207 </ref>
| |
|
| |
| ==References==
| |
| {{reflist|2}}
| |
|
| |
| ==Additional Resources==
| |
| * {{cite web | author=Western Cape Government Website, South Africa | title=Chris Barnard Performs World's First Heart Transplant | url=http://www.capegateway.gov.za/eng/pubs/public_info/C/99478# | date=21 February 2005 | publisher=Cape Gateway | accessdate=2007-01-10}}
| |
| * {{cite web | author=Department of Cardiothoracic Surgery | title=Patient's Guide to Heart Transplant Surgery | url=http://www.cts.usc.edu/ht-pg-hearttransplantprocedure.html | date= | publisher=University of Southern California | accessdate=2007-01-10}}
| |
| * {{cite web | author=Nancy Reid | title=Heart transplant: How is it performed? | url=http://health.yahoo.com/ency/healthwise/tx4074abc | date=September 22, 2005 | publisher=Healthwise | accessdate=2007-01-10}}
| |
| * {{cite web | author=Jeffrey Everett | title=Heart Transplant: Indications | url=http://health.allrefer.com/health/heart-transplant-indications.html | date=10/29/2003 | publisher=AllRefer.com | accessdate=2007-01-10}}
| |
| * {{cite web | author= | title=Hartford Hospital Heart Transplant Program | url=http://www.harthosp.org/transplant/heart.htm#indications | date= | publisher=Hartford Hospital, Connecticut, United States | accessdate=2007-01-10}}
| |
|
| |
| ==External links==
| |
| [http://www.heartofcapetown.co.za Official Heart Transplant Museum - Heart Of Cape Town]
| |
| <BR>
| |
|
| |
| {{Cardiac surgery}}
| |
| {{Organ transplantation}}
| |
| {{Electrocardiography}}
| |
| {{SIB}}
| |
| [[Category:Electrophysiology]]
| |
| [[Category:Cardiology]] | | [[Category:Cardiology]] |
| [[Category:Surgical procedures]] | | [[Category:Disease]] |
| [[Category:Surgery]] | | [[Category:Emergency medicine]] |
| | | [[Category:Intensive care medicine]] |
| | [[Category:Medicine]] |
|
| |
|
| [[de:Herztransplantation]] | | [[Category:Up-To-Date]] |
| [[es:Trasplante de corazón]] | | [[Category:Up-To-Date cardiology]] |
| [[fr:Transplantation cardiaque]]
| |
| [[hu:Szívátültetés]]
| |
| [[nl:Harttransplantatie]]
| |
| [[ja:心臓移植]]
| |
| [[ru:Пересадка сердца]]
| |
| [[simple:Heart transplant]]
| |
| [[uk:Трансплантація серця]]
| |
| [[tr:Kalp Nakli]]
| |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |