Halobetasol: Difference between revisions
No edit summary |
m (Protected "Halobetasol": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (2 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
{{DrugProjectFormSinglePage | {{DrugProjectFormSinglePage | ||
|authorTag= | |authorTag={{AV}} | ||
|genericName=halobetasol propionate | |genericName=halobetasol propionate | ||
|aOrAn=a | |aOrAn=a | ||
|drugClass=corticosteroid | |drugClass=[[corticosteroid]] | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication=the inflammatory and pruritic manifestations of corticosteroid-responsive | |indication=the [[inflammatory]] and [[pruritic]] manifestations of [[corticosteroid]]-responsive de[[r]]matoses | ||
|adverseReactions=<!--Black Box Warning--> | |adverseReactions=[[itching]], [[burning sensation|sensation of burning of skin]], [[stinging of skin]] | ||
<!--Black Box Warning--> | |||
|blackBoxWarningTitle=Title | |blackBoxWarningTitle=Title | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;">ConditionName: </span></i> | |blackBoxWarningBody=<i><span style="color:#FF0000;">ConditionName: </span></i> | ||
| Line 15: | Line 16: | ||
<!--FDA-Labeled Indications and Dosage (Adult)--> | <!--FDA-Labeled Indications and Dosage (Adult)--> | ||
|fdaLIADAdult=*Halobetasol propionate cream, 0.05% is a super-high potency corticosteroid indictated for the relief of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses. Treatment beyond two consecutive weeks is not recommended, and the total dosage should not exceed 50 g/week because of the potential for the drug to suppress the hypothalamic-pituitary-adrenal (HPA) axis. | |fdaLIADAdult=*Halobetasol propionate cream, 0.05% is a super-high potency [[corticosteroid]] indictated for the relief of the [[inflammatory]] and [[pruritic]] manifestations of [[corticosteroid]]-responsive [[dermatoses]]. Treatment beyond two consecutive weeks is not recommended, and the total dosage should not exceed 50 g/week because of the potential for the drug to suppress the [[HPA axis|hypothalamic-pituitary-adrenal (HPA) axis]]. | ||
*Use in children under 12 years of age is not recommended. As with other highly active corticosteroid, therapy should be discontinued when control has been achieved. If no improvement is seen within 2 weeks, reassessment of the diagnosis may be necessary. | *Use in children under 12 years of age is not recommended. As with other highly active [[corticosteroid]], therapy should be discontinued when control has been achieved. If no improvement is seen within 2 weeks, reassessment of the diagnosis may be necessary. | ||
=====Dosage===== | =====Dosage===== | ||
*Apply a thin layer of halobetasol propionate cream, 0.05% to the affected skin once or twice daily, as directed by your physician, and rub in gently and completely. | *Apply a thin layer of halobetasol propionate cream, 0.05% to the affected skin once or twice daily, as directed by your physician, and rub in gently and completely. | ||
*Halobetasol propionate cream, 0.05% is a super-high potency topical corticosteroid; therefore, treatment should be limited to two weeks, and amounts greater than 50 g/wk should not be used. As with other corticosteroids, therapy should be discontinued when control is achieved. If no improvement is seen within 2 weeks, reassessment of diagnosis may be necessary. | *Halobetasol propionate cream, 0.05% is a super-high potency topical [[corticosteroid]]; therefore, treatment should be limited to two weeks, and amounts greater than 50 g/wk should not be used. As with other [[corticosteroids]], therapy should be discontinued when control is achieved. If no improvement is seen within 2 weeks, reassessment of diagnosis may be necessary. | ||
*Halobetasol propionate cream, 0.05% should not be used with occlusive dressings. | *Halobetasol propionate cream, 0.05% should not be used with occlusive dressings. | ||
| Line 50: | Line 51: | ||
<!--Warnings--> | <!--Warnings--> | ||
|warnings= | |warnings= | ||
====Precautions==== | ====Precautions==== | ||
| Line 56: | Line 57: | ||
======General====== | ======General====== | ||
*Systemic absorption of topical corticosteroids can produce reversible hypothalamic-pituitary-adrenal (HPA) axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Manifestations of Cushing’s syndrome, hyperglycemia, and glucosuria can also be produced in some patients by systemic absorption of topical corticosteroids while on treatment. | *Systemic absorption of topical [[corticosteroids]] can produce reversible [[HPA axis|hypothalamic-pituitary-adrenal (HPA) axis]] suppression with the potential for [[glucocorticosteroid]] insufficiency after withdrawal of treatment. Manifestations of [[Cushing’s syndrome]], [[hyperglycemia]], and [[glucosuria]] can also be produced in some patients by systemic absorption of topical [[corticosteroids]] while on treatment. | ||
*Patients applying a topical steroid to a large surface area or to areas under occlusion should be evaluated periodically for evidence of HPA axis suppression. This may be done by using the ACTH stimulation, A.M. plasma cortisol, and urinary free-cortisol tests. Patients receiving super potent corticosteroids should not be treated for more than 2 weeks at a time and only small areas should be treated at any one time due to the increased risk of HPA suppression. | *Patients applying a topical [[steroid]] to a large surface area or to areas under occlusion should be evaluated periodically for evidence of [[HPA axis|HPA axis suppression]]. This may be done by using the ACTH stimulation, A.M. plasma [[cortisol]], and urinary free-cortisol tests. Patients receiving super potent [[corticosteroids]] should not be treated for more than 2 weeks at a time and only small areas should be treated at any one time due to the increased risk of HPA suppression. | ||
*Halobetasol propionate cream, 0.05% produced HPA axis suppression when used in divided doses at 7 grams per day for one week in patients with psoriasis. These effects were reversible upon discontinuation of treatment. | *Halobetasol propionate cream, 0.05% produced [[HPA axis|HPA axis suppression]] when used in divided doses at 7 grams per day for one week in patients with [[psoriasis]]. These effects were reversible upon discontinuation of treatment. | ||
*If HPA axis suppression is noted, an attempt should be made to withdraw the drug, to reduce the frequency of application, or to substitute a less potent corticosteroid. Recovery of HPA axis function is generally prompt upon discontinuation of topical corticosteroids. Infrequently, signs and symptoms of glucocorticosteroid insufficiency may occur requiring supplemental systemic corticosteroids. For information on systemic supplementation, see prescribing information for those products. | *If [[HPA axis|HPA axis suppression]] is noted, an attempt should be made to withdraw the drug, to reduce the frequency of application, or to substitute a less potent [[corticosteroid]]. Recovery of HPA axis function is generally prompt upon discontinuation of topical [[corticosteroids]]. Infrequently, signs and symptoms of [[glucocorticosteroid]] insufficiency may occur requiring supplemental systemic [[corticosteroids]]. For information on systemic supplementation, see prescribing information for those products. | ||
*Pediatric patients may be more susceptible to systemic toxicity from equivalent doses due to their larger skin surface to body mass ratios | *Pediatric patients may be more susceptible to systemic toxicity from equivalent doses due to their larger skin surface to body mass ratios . | ||
*If irritation develops, halobetasol propionate cream, 0.05% should be discontinued and appropriate therapy instituted. Allergic contact dermatitis with corticosteroids is usually diagnosed by observing failure to heal rather than noting a clinical exacerbation as with most topical products not containing corticosteroids. Such an observation should be corroborated with appropriate diagnostic patch testing. | *If irritation develops, halobetasol propionate cream, 0.05% should be discontinued and appropriate therapy instituted. Allergic [[contact dermatitis]] with [[corticosteroids]] is usually diagnosed by observing failure to heal rather than noting a clinical exacerbation as with most topical products not containing [[corticosteroids]]. Such an observation should be corroborated with appropriate diagnostic patch testing. | ||
*If concomitant skin infections are present or develop, an appropriate antifungal or antibacterial agent should be used. If a favorable response does not occur promptly, use of halobetasol propionate cream, 0.05% should be discontinued until the infection has been adequately controlled. | *If concomitant skin infections are present or develop, an appropriate [[antifungal]] or [[antibacterial]] agent should be used. If a favorable response does not occur promptly, use of halobetasol propionate cream, 0.05% should be discontinued until the infection has been adequately controlled. | ||
*Halobetasol propionate cream, 0.05% should not be used in the treatment of rosacea or perioral dermatitis, and it should not be used on the face, groin, or in the axillae. | *Halobetasol propionate cream, 0.05% should not be used in the treatment of [[rosacea]] or perioral [[dermatitis]], and it should not be used on the face, groin, or in the [[axillae]]. | ||
<!--Adverse Reactions--> | <!--Adverse Reactions--> | ||
<!--Clinical Trials Experience--> | <!--Clinical Trials Experience--> | ||
|clinicalTrials=*In controlled clinical trials, the most frequent adverse events reported for halobetasol propionate cream, 0.05% included stinging, burning or itching in 4.4% of the patients. Less frequently reported adverse reactions were dry skin, erythema, skin atrophy, leukoderma, vesicles and rash. | |clinicalTrials=*In controlled clinical trials, the most frequent adverse events reported for halobetasol propionate cream, 0.05% included stinging, burning or itching in 4.4% of the patients. Less frequently reported adverse reactions were [[dry skin]], [[erythema]], [[skin atrophy]], [[leukoderma]], vesicles and [[rash]]. | ||
*The following additional local adverse reactions are reported infrequently with topical corticosteroids, and they may occur more frequently with high potency corticosteroids, such as halobetasol propionate cream, 0.05%. These reactions are listed in an approximate decreasing order of occurrence: folliculitis, hypertrichosis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, secondary infection, striae and miliaria. | *The following additional local adverse reactions are reported infrequently with topical [[corticosteroids]], and they may occur more frequently with high potency [[corticosteroids]], such as halobetasol propionate cream, 0.05%. These reactions are listed in an approximate decreasing order of occurrence: [[folliculitis]], [[hypertrichosis]], acneiform eruptions, [[hypopigmentation]], perioral [[dermatitis]], allergic contact [[dermatitis]], secondary infection, striae and [[miliaria]]. | ||
<!--Postmarketing Experience--> | <!--Postmarketing Experience--> | ||
|postmarketing=There is limited information regarding <i>Postmarketing Experience</i> of {{PAGENAME}} in the drug label. | |postmarketing=There is limited information regarding <i>Postmarketing Experience</i> of {{PAGENAME}} in the drug label. | ||
<!--Drug Interactions--> | <!--Drug Interactions--> | ||
|drugInteractions= | |drugInteractions= | ||
<!--Use in Specific Populations--> | <!--Use in Specific Populations--> | ||
|FDAPregCat=C | |FDAPregCat=C | ||
|useInPregnancyFDA=*Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Some corticosteroids have been shown to be teratogenic after dermal application in laboratory animals. | |useInPregnancyFDA=*[[Corticosteroids]] have been shown to be [[teratogenic]] in laboratory animals when administered systemically at relatively low dosage levels. Some [[corticosteroids]] have been shown to be teratogenic after dermal application in laboratory animals. | ||
*Halobetasol propionate has been shown to be teratogenic in SPF rats and chinchilla-type rabbits when given systemically during gestation at doses of 0.04 to 0.1 mg/kg in rats and 0.01 mg/kg in rabbits. These doses are approximately 13, 33 and 3 times, respectively, the human topical dose of halobetasol propionate cream, 0.05%. Halobetasol propionate was embryotoxic in rabbits but not in rats. | *Halobetasol propionate has been shown to be teratogenic in SPF rats and chinchilla-type rabbits when given systemically during gestation at doses of 0.04 to 0.1 mg/kg in rats and 0.01 mg/kg in rabbits. These doses are approximately 13, 33 and 3 times, respectively, the human topical dose of halobetasol propionate cream, 0.05%. Halobetasol propionate was embryotoxic in rabbits but not in rats. | ||
*Cleft palate was observed in both rats and rabbits. Omphalocele was seen in rats, but not in rabbits. | *Cleft palate was observed in both rats and rabbits. [[Omphalocele]] was seen in rats, but not in rabbits. | ||
*There are no adequate and well-controlled studies of teratogenic potential of halobetasol propionate in pregnant women. Halobetasol propionate cream, 0.05% should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. | *There are no adequate and well-controlled studies of teratogenic potential of halobetasol propionate in pregnant women. Halobetasol propionate cream, 0.05% should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. | ||
| Line 101: | Line 98: | ||
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | ||
|useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | |useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | ||
|useInNursing=*Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when halobetasol propionate cream, 0.05% is administered to a nursing woman. | |useInNursing=*Systemically administered [[corticosteroids]] appear in human milk and could suppress growth, interfere with endogenous [[corticosteroid]] production, or cause other untoward effects. It is not known whether topical administration of [[corticosteroids]] could result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when halobetasol propionate cream, 0.05% is administered to a nursing woman. | ||
|useInPed=*Safety and effectiveness of halobetasol propionate cream, 0.05% in pedriatric patients have not been established and use in pediatric patients under 12 is not recommended. Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of HPA suppression and Cushing’s syndrome when they are treated with topical corticosteroids. They are therefore also at greater risk of adrenal insufficiency during or after withdrawal of treatment. Adverse effects including striae have been reported with inappropriate use of topical corticosteroids in infants and children. | |useInPed=*Safety and effectiveness of halobetasol propionate cream, 0.05% in pedriatric patients have not been established and use in pediatric patients under 12 is not recommended. Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of HPA suppression and [[Cushing’s syndrome]] when they are treated with topical [[corticosteroids]]. They are therefore also at greater risk of [[adrenal insufficiency]] during or after withdrawal of treatment. Adverse effects including striae have been reported with inappropriate use of topical [[corticosteroids]] in infants and children. | ||
HPA axis suppression, Cushing’s syndrome, linear growth retardation, delayed weight gain and intracranial hypertension have been reported in children receiving topical corticosteroids. Manifestations of adrenal suppression in children include low plasma cortisol levels and an absence of response to ACTH stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema. | [[HPA axis suppression]], [[Cushing’s syndrome]], linear growth retardation, delayed weight gain and [[intracranial hypertension]] have been reported in children receiving topical [[corticosteroids]]. Manifestations of adrenal suppression in children include low plasma [[cortisol]] levels and an absence of response to [[ACTH]] stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral [[papilledema]]. | ||
|useInGeri=*Of approximately 400 patients treated with halobetasol propionate cream, 0.05% in clinical studies, 25% were 61 years and over and 6% were 71 years and over. No overall differences in safety or effectiveness were observed between these patients and younger patients; and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. | |useInGeri=*Of approximately 400 patients treated with halobetasol propionate cream, 0.05% in clinical studies, 25% were 61 years and over and 6% were 71 years and over. No overall differences in safety or effectiveness were observed between these patients and younger patients; and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. | ||
|useInGender=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | |useInGender=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | ||
|useInRace=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | |useInRace=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | ||
|useInRenalImpair=There is no FDA guidance on the use of {{PAGENAME}} in patients with renal impairment. | |useInRenalImpair=There is no FDA guidance on the use of {{PAGENAME}} in patients with [[renal impairment]]. | ||
|useInHepaticImpair=There is no FDA guidance on the use of {{PAGENAME}} in patients with hepatic impairment. | |useInHepaticImpair=There is no FDA guidance on the use of {{PAGENAME}} in patients with [[hepatic impairment]]. | ||
|useInReproPotential=There is no FDA guidance on the use of {{PAGENAME}} in women of reproductive potentials and males. | |useInReproPotential=There is no FDA guidance on the use of {{PAGENAME}} in women of reproductive potentials and males. | ||
|useInImmunocomp=There is no FDA guidance one the use of {{PAGENAME}} in patients who are immunocompromised. | |useInImmunocomp=There is no FDA guidance one the use of {{PAGENAME}} in patients who are [[immunocompromised]]. | ||
<!--Administration and Monitoring--> | <!--Administration and Monitoring--> | ||
|administration=*Topical | |administration=*Topical | ||
|monitoring=*The following tests may be helpful in evaluating patients for HPA axis suppression: ACTH-stimulation test; A.M. plasma-cortisol test; urinary free-cortisol test. | |monitoring=*The following tests may be helpful in evaluating patients for [[HPA axis|HPA axis suppression]]: [[ACTH-stimulation test]]; A.M. [[plasma-cortisol test]]; [[urinary free-cortisol test]]. | ||
<!--IV Compatibility--> | <!--IV Compatibility--> | ||
| Line 125: | Line 122: | ||
<!--Drug box 2--> | <!--Drug box 2--> | ||
|drugBox={{ | |drugBox={{Drugbox2 | ||
| Verifiedfields = changed | | Verifiedfields = changed | ||
| verifiedrevid = 470619490 | | verifiedrevid = 470619490 | ||
| Line 184: | Line 181: | ||
<!--Structure--> | <!--Structure--> | ||
|structure=* Halobetasol propionate cream, 0.05% contains halobetasol propionate, a synthetic corticosteroid for topical dermatological use. The corticosteroids constitute a class of primarily synthetic steroids used topically as an anti-inflammatory and antipruritic agent. | |structure=* Halobetasol propionate cream, 0.05% contains halobetasol propionate, a synthetic [[corticosteroid]] for topical dermatological use. The [[corticosteroids]] constitute a class of primarily synthetic steroids used topically as an [[anti-inflammatory]] and [[antipruritic]] agent. | ||
*Chemically halobetasol propionate is 21-chloro-6α, 9-difluoro-11β, 17-dihydroxy-16β-methylpregna-1, 4-diene-3-20-dione, 17-propionate, C25H31CIF2O5. It has the following structural formula: | *Chemically halobetasol propionate is 21-chloro-6α, 9-difluoro-11β, 17-dihydroxy-16β-methylpregna-1, 4-diene-3-20-dione, 17-propionate, C25H31CIF2O5. It has the following structural formula: | ||
| Line 202: | Line 199: | ||
*Long-term animal studies have not been performed to evaluate the carcinogenic potential of halobetasol propionate. | *Long-term animal studies have not been performed to evaluate the carcinogenic potential of halobetasol propionate. | ||
*Positive mutagenicity effects were observed in two genotoxicity assays. Halobetasol propionate was positive in a Chinese hamster micronucleus test, and in a mouse lymphoma gene mutation assay in vitro. | *Positive [[mutagenicity]] effects were observed in two [[genotoxicity]] assays. Halobetasol propionate was positive in a Chinese hamster [[micronucleus test]], and in a mouse lymphoma gene mutation assay in vitro. | ||
*Studies in the rat following oral administration at dose levels up to 50 μg/kg/day indicated no impairment of fertility or general reproductive performance. | *Studies in the rat following oral administration at dose levels up to 50 μg/kg/day indicated no impairment of fertility or general reproductive performance. | ||
*In other genotoxicity testing, halobetasol propionate was not found to be genotoxic in the Ames/Salmonella assay, in the sister chromatid exchange test in somatic cells of the Chinese hamster, in chromosome aberration studies of germinal and somatic cells of rodents, and in a mammalian spot test to determine point mutations. | *In other [[genotoxicity]] testing, halobetasol propionate was not found to be genotoxic in the Ames/Salmonella assay, in the sister chromatid exchange test in somatic cells of the Chinese hamster, in chromosome aberration studies of germinal and somatic cells of rodents, and in a mammalian spot test to determine point mutations. | ||
<!--Clinical Studies--> | <!--Clinical Studies--> | ||
|clinicalStudies=There is limited information regarding <i>Clinical Studies</i> of {{PAGENAME}} in the drug label. | |clinicalStudies=There is limited information regarding <i>Clinical Studies</i> of {{PAGENAME}} in the drug label. | ||
| Line 220: | Line 217: | ||
<!--Patient Counseling Information--> | <!--Patient Counseling Information--> | ||
|storage=*Store at 20 - 25°C (68 - 77°F) (See USP Controlled Room Temperature). | |storage=*Store at 20 - 25°C (68 - 77°F) (See USP Controlled Room Temperature). | ||
|fdaPatientInfo=*Patients using topical corticosteroids should receive the following information and instructions:1. The medication is to be used as directed by the physician. It is for external use only. Avoid contact with the eyes. | |fdaPatientInfo=*Patients using topical [[corticosteroids]] should receive the following information and instructions:1. The medication is to be used as directed by the physician. It is for external use only. Avoid contact with the eyes. | ||
*The medication should not be used for any disorder other than that for which it was prescribed. | *The medication should not be used for any disorder other than that for which it was prescribed. | ||
Latest revision as of 16:27, 20 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Halobetasol is a corticosteroid that is FDA approved for the treatment of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses. Common adverse reactions include itching, sensation of burning of skin, stinging of skin.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Halobetasol propionate cream, 0.05% is a super-high potency corticosteroid indictated for the relief of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses. Treatment beyond two consecutive weeks is not recommended, and the total dosage should not exceed 50 g/week because of the potential for the drug to suppress the hypothalamic-pituitary-adrenal (HPA) axis.
- Use in children under 12 years of age is not recommended. As with other highly active corticosteroid, therapy should be discontinued when control has been achieved. If no improvement is seen within 2 weeks, reassessment of the diagnosis may be necessary.
Dosage
- Apply a thin layer of halobetasol propionate cream, 0.05% to the affected skin once or twice daily, as directed by your physician, and rub in gently and completely.
- Halobetasol propionate cream, 0.05% is a super-high potency topical corticosteroid; therefore, treatment should be limited to two weeks, and amounts greater than 50 g/wk should not be used. As with other corticosteroids, therapy should be discontinued when control is achieved. If no improvement is seen within 2 weeks, reassessment of diagnosis may be necessary.
- Halobetasol propionate cream, 0.05% should not be used with occlusive dressings.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Halobetasol in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Halobetasol in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Halobetasol in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Halobetasol in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Halobetasol in pediatric patients.
Contraindications
- Halobetasol propionate cream, 0.05% is contraindicated in those patients with a history of hypersensitivity to any of the components of the preparation.
Warnings
Precautions
General
- Systemic absorption of topical corticosteroids can produce reversible hypothalamic-pituitary-adrenal (HPA) axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Manifestations of Cushing’s syndrome, hyperglycemia, and glucosuria can also be produced in some patients by systemic absorption of topical corticosteroids while on treatment.
- Patients applying a topical steroid to a large surface area or to areas under occlusion should be evaluated periodically for evidence of HPA axis suppression. This may be done by using the ACTH stimulation, A.M. plasma cortisol, and urinary free-cortisol tests. Patients receiving super potent corticosteroids should not be treated for more than 2 weeks at a time and only small areas should be treated at any one time due to the increased risk of HPA suppression.
- Halobetasol propionate cream, 0.05% produced HPA axis suppression when used in divided doses at 7 grams per day for one week in patients with psoriasis. These effects were reversible upon discontinuation of treatment.
- If HPA axis suppression is noted, an attempt should be made to withdraw the drug, to reduce the frequency of application, or to substitute a less potent corticosteroid. Recovery of HPA axis function is generally prompt upon discontinuation of topical corticosteroids. Infrequently, signs and symptoms of glucocorticosteroid insufficiency may occur requiring supplemental systemic corticosteroids. For information on systemic supplementation, see prescribing information for those products.
- Pediatric patients may be more susceptible to systemic toxicity from equivalent doses due to their larger skin surface to body mass ratios .
- If irritation develops, halobetasol propionate cream, 0.05% should be discontinued and appropriate therapy instituted. Allergic contact dermatitis with corticosteroids is usually diagnosed by observing failure to heal rather than noting a clinical exacerbation as with most topical products not containing corticosteroids. Such an observation should be corroborated with appropriate diagnostic patch testing.
- If concomitant skin infections are present or develop, an appropriate antifungal or antibacterial agent should be used. If a favorable response does not occur promptly, use of halobetasol propionate cream, 0.05% should be discontinued until the infection has been adequately controlled.
- Halobetasol propionate cream, 0.05% should not be used in the treatment of rosacea or perioral dermatitis, and it should not be used on the face, groin, or in the axillae.
Adverse Reactions
Clinical Trials Experience
- In controlled clinical trials, the most frequent adverse events reported for halobetasol propionate cream, 0.05% included stinging, burning or itching in 4.4% of the patients. Less frequently reported adverse reactions were dry skin, erythema, skin atrophy, leukoderma, vesicles and rash.
- The following additional local adverse reactions are reported infrequently with topical corticosteroids, and they may occur more frequently with high potency corticosteroids, such as halobetasol propionate cream, 0.05%. These reactions are listed in an approximate decreasing order of occurrence: folliculitis, hypertrichosis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, secondary infection, striae and miliaria.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Halobetasol in the drug label.
Drug Interactions
There is limited information regarding Halobetasol Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
- Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Some corticosteroids have been shown to be teratogenic after dermal application in laboratory animals.
- Halobetasol propionate has been shown to be teratogenic in SPF rats and chinchilla-type rabbits when given systemically during gestation at doses of 0.04 to 0.1 mg/kg in rats and 0.01 mg/kg in rabbits. These doses are approximately 13, 33 and 3 times, respectively, the human topical dose of halobetasol propionate cream, 0.05%. Halobetasol propionate was embryotoxic in rabbits but not in rats.
- Cleft palate was observed in both rats and rabbits. Omphalocele was seen in rats, but not in rabbits.
- There are no adequate and well-controlled studies of teratogenic potential of halobetasol propionate in pregnant women. Halobetasol propionate cream, 0.05% should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Halobetasol in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Halobetasol during labor and delivery.
Nursing Mothers
- Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when halobetasol propionate cream, 0.05% is administered to a nursing woman.
Pediatric Use
- Safety and effectiveness of halobetasol propionate cream, 0.05% in pedriatric patients have not been established and use in pediatric patients under 12 is not recommended. Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of HPA suppression and Cushing’s syndrome when they are treated with topical corticosteroids. They are therefore also at greater risk of adrenal insufficiency during or after withdrawal of treatment. Adverse effects including striae have been reported with inappropriate use of topical corticosteroids in infants and children.
HPA axis suppression, Cushing’s syndrome, linear growth retardation, delayed weight gain and intracranial hypertension have been reported in children receiving topical corticosteroids. Manifestations of adrenal suppression in children include low plasma cortisol levels and an absence of response to ACTH stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema.
Geriatic Use
- Of approximately 400 patients treated with halobetasol propionate cream, 0.05% in clinical studies, 25% were 61 years and over and 6% were 71 years and over. No overall differences in safety or effectiveness were observed between these patients and younger patients; and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Gender
There is no FDA guidance on the use of Halobetasol with respect to specific gender populations.
Race
There is no FDA guidance on the use of Halobetasol with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Halobetasol in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Halobetasol in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Halobetasol in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Halobetasol in patients who are immunocompromised.
Administration and Monitoring
Administration
- Topical
Monitoring
- The following tests may be helpful in evaluating patients for HPA axis suppression: ACTH-stimulation test; A.M. plasma-cortisol test; urinary free-cortisol test.
IV Compatibility
There is limited information regarding IV Compatibility of Halobetasol in the drug label.
Overdosage
- Topically applied halobetasol propionate cream, 0.05% can be absorbed in sufficient amounts to produce systemic effects
Pharmacology
| |
Halobetasol
| |
| Systematic (IUPAC) name | |
| (6α,11β,16β)-21-chloro-6,9-difluoro-11,17-dihydroxy-16-methylpregna-1,4-diene-3,20-dione | |
| Identifiers | |
| CAS number | |
| ATC code | D07 |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 428.897 |
| SMILES | & |
| Synonyms | (6S,8S,9S,10S,11S,13S,14S,16S,17R)-17-(2-Chloroacetyl)-6,9-difluoro-11,17-dihydroxy-10,13,16-trimethyl-6,7,8,11,12,14,15,16-octahydrocyclopenta[a]phenanthren-3-one |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
Structure
- Halobetasol propionate cream, 0.05% contains halobetasol propionate, a synthetic corticosteroid for topical dermatological use. The corticosteroids constitute a class of primarily synthetic steroids used topically as an anti-inflammatory and antipruritic agent.
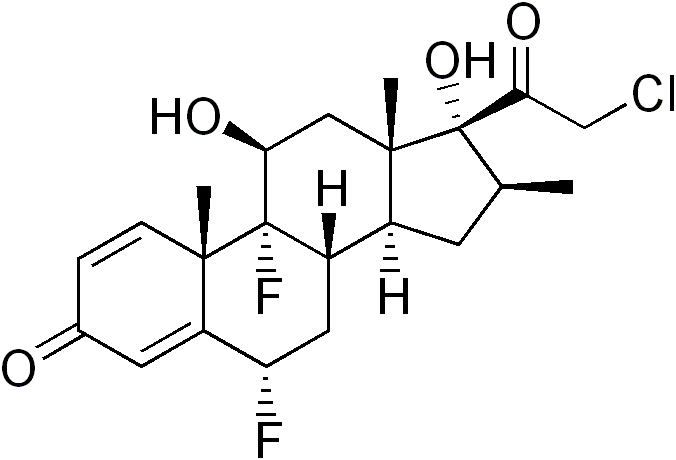
- Chemically halobetasol propionate is 21-chloro-6α, 9-difluoro-11β, 17-dihydroxy-16β-methylpregna-1, 4-diene-3-20-dione, 17-propionate, C25H31CIF2O5. It has the following structural formula:
- Halobetasol propionate has the molecular weight of 485. It is a white crystalline powder insoluble in water.
- Each gram of halobetasol propionate cream, 0.05% contains 0.5 mg of halobetasol propionate in a cream base of cetyl alcohol, diazolidinyl urea, glycerin, isopropyl isostearate, isopropyl palmitate, methylchloroisothiazolinone, (and) methylisothiazolinone, steareth-21 and water.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Halobetasol in the drug label.
Pharmacokinetics
There is limited information regarding Pharmacokinetics of Halobetasol in the drug label.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Long-term animal studies have not been performed to evaluate the carcinogenic potential of halobetasol propionate.
- Positive mutagenicity effects were observed in two genotoxicity assays. Halobetasol propionate was positive in a Chinese hamster micronucleus test, and in a mouse lymphoma gene mutation assay in vitro.
- Studies in the rat following oral administration at dose levels up to 50 μg/kg/day indicated no impairment of fertility or general reproductive performance.
- In other genotoxicity testing, halobetasol propionate was not found to be genotoxic in the Ames/Salmonella assay, in the sister chromatid exchange test in somatic cells of the Chinese hamster, in chromosome aberration studies of germinal and somatic cells of rodents, and in a mammalian spot test to determine point mutations.
Clinical Studies
There is limited information regarding Clinical Studies of Halobetasol in the drug label.
How Supplied
- Halobetasol propionate cream, 0.05% is supplied in the following tube sizes:
- 15 g (NDC 45802-129-35)
- 50 g (NDC 45802-129-32)
Storage
- Store at 20 - 25°C (68 - 77°F) (See USP Controlled Room Temperature).
Images
Drug Images
{{#ask: Page Name::Halobetasol |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Halobetasol |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Patients using topical corticosteroids should receive the following information and instructions:1. The medication is to be used as directed by the physician. It is for external use only. Avoid contact with the eyes.
- The medication should not be used for any disorder other than that for which it was prescribed.
- The treated skin area should not be bandaged, or otherwise covered or wrapped, so as to be occlusive unless directed by the physician.
- Patients should report to their physician any signs of local adverse reactions.
Precautions with Alcohol
- Alcohol-Halobetasol interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Ultravate
- Ultravate X
Look-Alike Drug Names
There is limited information regarding Halobetasol Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Halobetasol |Label Name=Halobetasol02.png
}}
{{#subobject:
|Label Page=Halobetasol |Label Name=Halobetasol03.png
}}
