Gallbladder cancer pathophysiology: Difference between revisions
Farima Kahe (talk | contribs) |
Farima Kahe (talk | contribs) |
||
| Line 38: | Line 38: | ||
== Gross Pathology == | == Gross Pathology == | ||
* On [[gross pathology]], fibrosis and thickening of the gallbladder are characteristic findings of the gallbladder cancer. | * On [[gross pathology]], [[fibrosis]] and thickening of the gallbladder are characteristic findings of the gallbladder cancer. | ||
* Most of the times associated with [[Gallstone|gallstones]] > 3 cm in diameter. | * Most of the times associated with [[Gallstone|gallstones]] > 3 cm in diameter. | ||
Revision as of 16:06, 19 December 2018
|
Gallbladder cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Gallbladder cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Gallbladder cancer pathophysiology |
|
Risk calculators and risk factors for Gallbladder cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Manpreet Kaur, MD [2]
Overview
Gallbladder cancer usually develops in the setting of chronic inflammation of the gallbladder.The most common source of chronic inflammation is cholesterol gallstones. The gallbladder cancer risk increases to 4-5% in the presence gallbladder cancer (GBC) is the result of 2 or more different biological pathways based on morphological, genetic, and molecular evidence. Metaplasia is believed to be one of the pathological reason behind the development of gallbladder carcinoma. Although the definite relationship between metaplasia and dysplasia, is not clearly established yet. On gross pathology, fibrosis and thickening of the gallbladder are characteristic findings of the gallbladder cancer. On microscopic histopathological analysis, outer portion is often better differentiated than deeper portion are characteristic findings of gallbladder cancer.
Pathophysiology
Pathogenesis[1]
- It is understood that GBC is the result of persistent irritation of the gallbladder mucosa over a period of years which predispose to malignant transformation or act as an enhancer for carcinogenic exposure.
- The primary mechanism involves cholelithiasis and resultant cholecystitis and appears to be the driving force in most areas of the arena, whereas GBC is strongly related to gallstone disease, female gender bias, and age over 65.
Theory 1:
- In the setting of a chronically inflamed gallbladder, metaplasia is not unusual.[1]
- Similar to metaplasia of the stomach, gallbladder metaplasia happens in two forms:
- Gastric form
- Intestinal form
- Chronically inflamed gallbladder may additionally express both pyloric gland and intestinal metaplasia.
- Fluke-infested gallbladders more commonly shows intestinal metaplasia and p53 mutations than sporadic gallbladder cancers.[2][3]
- The definite relationship between metaplasia and dysplasia, is not clearly established yet.
- The first concept indicates that dysplasia progresses to carcinoma in situ (CIS) which can become invasive, in the next stages.
- This concept is supported via the finding that over 80% of invasive gallbladder cancers have adjoining areas of CIS and epithelial dysplasia.
- One study validated the presence of metaplasia, dysplasia, and CIS adjoining to cancer in 66%, 81.3%, and 69%, respectively.
- Dysplastic lesions have molecular genetic proof that supports progression towards CIS.
- It is well recognized that gallbladder dysplasia progresses to invasive most cancers normally over a path of 15 to 19 years.
Theory 2[4][5][6][7]
- There are also histologic and molecular differences in GBCs related to anomalous pancreaticobiliary duct junction and in the ones related to gallstones, providing further proof that two different pathogenetic pathways are involved.
- GBC arising in Japan within the setting of an anomalous pancreaticobiliary duct junction is characterized by means of KRAS mutations and relatively late onset of p53 mutations.[4] [5]
- By means of comparison, as a minimum in Chilean patients with cholelithiasis and chronic cholecystitis, KRAS mutations are uncommon, while p53 mutations rise up early at some stage in multistage pathogenesis.[6][7]
Theory 3[8]
- Less than 3% of early gallbladder carcinomas have adenomatous remnants, indicating this mechanism has less importance within the carcinogenic pathway.[8]
- It's hard to predict which of those will go through malignant transformation.
- In contrast to properly-established carcinogenic pathways in colorectal most cancers, it remains debated within the literature whether or not or not adenomas are actual precursors of invasive gallbladder carcinomas.
- Only 1% of cholecystectomy specimens have adenomatous polyps as preneoplastic lesions.
Gross Pathology
- On gross pathology, fibrosis and thickening of the gallbladder are characteristic findings of the gallbladder cancer.
- Most of the times associated with gallstones > 3 cm in diameter.
- Liver spread is usually evident at time of diagnosis.
Microscopic Pathology
- On microscopic histopathological analysis, outer portion is often better differentiated than deeper portion are characteristic findings of gallbladder cancer.
- On microscopic analysis tumor May extend to Rokitansky-Aschoff sinuses.
- Atypical cuboidal cells are one of the microscopical findings of the high grade tumor.
- Infiltrative or exophytic tumor.
- Well formed glands in papillary architecture with wide lumina are noted in microscopical findings.
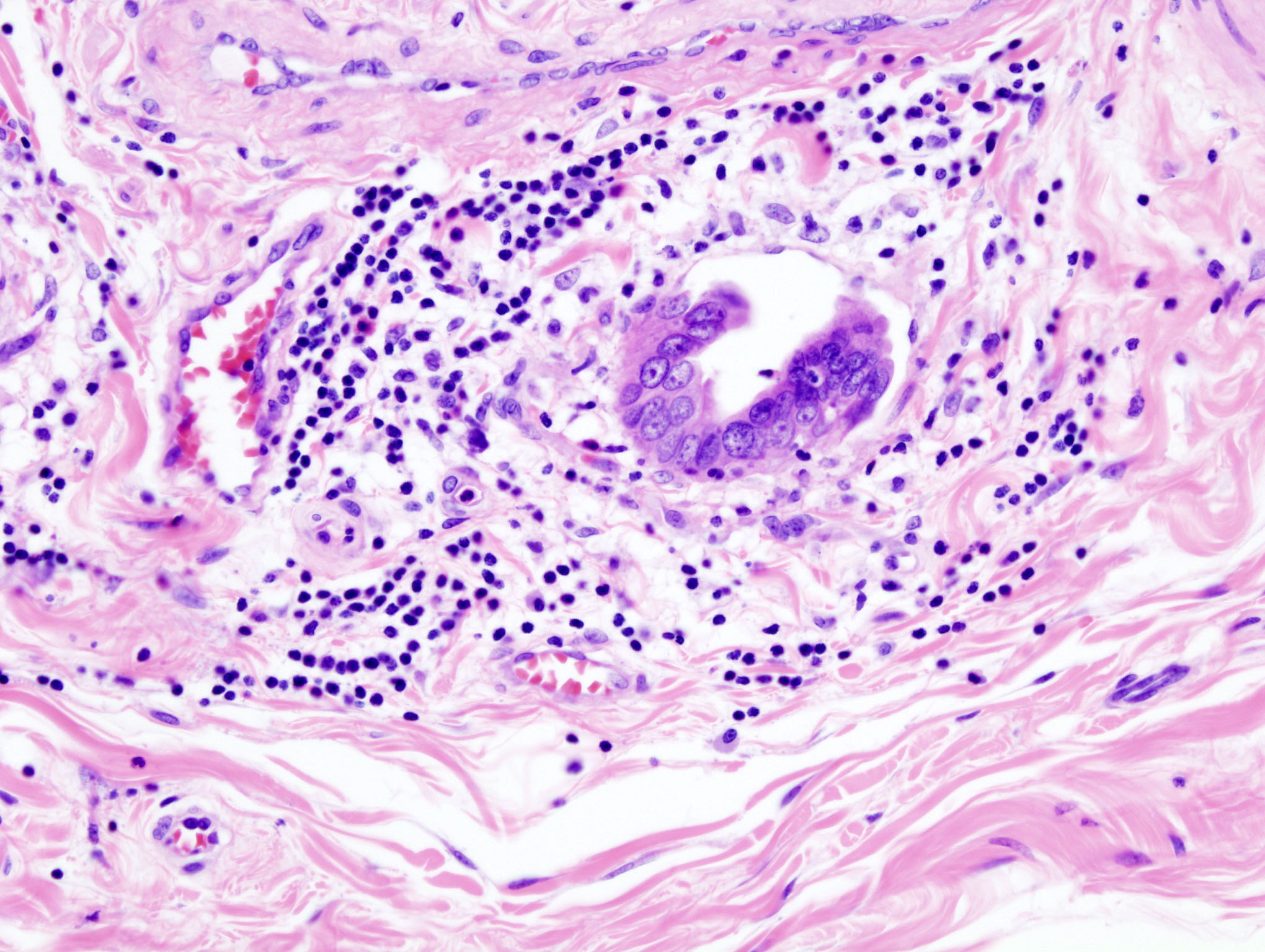
By:CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=507411
References
- ↑ 1.0 1.1 Roa I, de Aretxabala X, Araya JC, Roa J (2006). "Preneoplastic lesions in gallbladder cancer". J Surg Oncol. 93 (8): 615–23. doi:10.1002/jso.20527. PMID 16724345.
- ↑ Wistuba II, Sugio K, Hung J, Kishimoto Y, Virmani AK, Roa I, Albores-Saavedra J, Gazdar AF (1995). "Allele-specific mutations involved in the pathogenesis of endemic gallbladder carcinoma in Chile". Cancer Res. 55 (12): 2511–5. PMID 7780959.
- ↑ Hughes NR, Bhathal PS (2013). "Adenocarcinoma of gallbladder: an immunohistochemical profile and comparison with cholangiocarcinoma". J. Clin. Pathol. 66 (3): 212–7. doi:10.1136/jclinpath-2012-201146. PMID 23268317.
- ↑ 4.0 4.1 Solaini L, Sharma A, Watt J, Iosifidou S, Chin Aleong JA, Kocher HM (2014). "Predictive factors for incidental gallbladder dysplasia and carcinoma". J. Surg. Res. 189 (1): 17–21. doi:10.1016/j.jss.2014.01.064. PMID 24589178.
- ↑ 5.0 5.1 Mano H, Roa I, Araya JC, Ohta T, Yoshida K, Araki K, Kinebuchi H, Ishizu T, Nakadaira H, Endoh K, Yamamoto M, Watanabe H (1996). "Comparison of mutagenic activity of bile between Chilean and Japanese female patients having cholelithiasis". Mutat. Res. 371 (1–2): 73–7. PMID 8950352.
- ↑ 6.0 6.1 Hanada K, Tsuchida A, Iwao T, Eguchi N, Sasaki T, Morinaka K, Matsubara K, Kawasaki Y, Yamamoto S, Kajiyama G (1999). "Gene mutations of K-ras in gallbladder mucosae and gallbladder carcinoma with an anomalous junction of the pancreaticobiliary duct". Am. J. Gastroenterol. 94 (6): 1638–42. doi:10.1111/j.1572-0241.1999.01155.x. PMID 10364037.
- ↑ 7.0 7.1 Hidaka E, Yanagisawa A, Seki M, Takano K, Setoguchi T, Kato Y (2000). "High frequency of K-ras mutations in biliary duct carcinomas of cases with a long common channel in the papilla of Vater". Cancer Res. 60 (3): 522–4. PMID 10676628.
- ↑ 8.0 8.1 Kanthan R, Senger JL, Ahmed S, Kanthan SC (2015). "Gallbladder Cancer in the 21st Century". J Oncol. 2015: 967472. doi:10.1155/2015/967472. PMC 4569807. PMID 26421012.