Gallbladder cancer
For patient information click here
Template:DiseaseDisorder infobox
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Gallbladder cancer is a relatively uncommon cancer. If it is diagnosed early enough, it can be cured by removing the gallbladder. Most often it is found after symptoms such as abdominal pain and jaundice occur, and it has spread to other organs such as the liver.
It is a rare cancer that is still being studied and thought to be related to gallstones building up, which also can lead to calcification of the gallbladder, a condition known as Porcelain gallbladder. Porcelain gallbladder is also rare and most people with porcelain gallbladder also have gallbladder cancer. The connection is uncertain. The outlook is poor for recovery if the cancer is found after symptoms have started to occur.
- The most common type is gallbladder adenocarcinoma
Then there is information on rare types of gallbladder cancer
- Squamous cell cancer of the gallbladder
- Adenosquamous carcinoma of the gallbladder
- Small cell carcinoma of the gallbladder
- Sarcoma of the gallbladder
- Neuroendocrine tumour of the gallbladder
- Lymphoma and melanoma of the gallbladder
Epidemiology
Estimated new cases and deaths from gallbladder (and other biliary) cancer in the United States in 2008:[1]
- New cases: 9,520.
- Deaths: 3,340.
Etiology
Cancer that arises in the gallbladder is uncommon.
Cholelithiasis is an associated finding in the majority of cases, but less than 1% of patients with cholelithiasis develop this cancer.
Cellular Classification
The histologic types of gallbladder cancer include the following.[2] Some histologic types have a better prognosis than others; papillary carcinomas have the best prognosis.
- Carcinoma in situ.
- Adenocarcinoma, not otherwise specified (NOS).
- Papillary carcinoma.
- Adenocarcinoma, intestinal type.
- Mucinous carcinoma.
- Clear cell adenocarcinoma.
- Signet-ring cell carcinoma.
- Adenosquamous carcinoma.
- Squamous cell carcinoma.
- Small cell (oat cell) carcinoma.(Grade 4 by definition)
- Undifferentiated carcinoma.(Grade 4 by definition)
- Carcinoma, NOS.
- Carcinosarcoma.
Risk factors
- Gender: More women than men are affected by gallbladder cancer, mostly commonly between the ages of 50 and 60.
- Obesity increases the risk for gallbladder cancer. It is most common in indigenous peoples of the Americas.
- Primary carcinoma is linked to chronic cholecystitis and cholelithiasis.
- Alcohol: "…alcohol drinking is a risk factor of gallbladder cancer…"[3] [4]
Signs and Symptoms
The most common symptoms caused by gallbladder cancer are jaundice, pain, and fever. General symptoms are as follow;
- Steady pain in the upper right abdomen for around 2 months.
- Diarrhea
- Burping
- Weakness
- Loss of appetite
- Weight loss
- Vomiting
- Infection, leading to peritonitis, gangrene, perforation, and or liver abscess
- Jaundice, due to obstruction
Early symptoms mimic gallbladder inflammation and gallstones, which must be excluded as the cause. Later, the symptoms may be that of biliary obstruction.
Disease Course
Most tumors are adenocarcinomas, with a small percent being squamous cell carcinomas. The cancer commonly spreads to the liver, pancreas, stomach,and duodenum.
Diagnosis
Early diagnosis is not generally possible. People at high risk, such as women or Native Americans with frequent gallstones, are evaluated closely. Endoscopic ultrasound, transabdominal ultrasound, CT scan, MRI, and MR cholangiopancreatography can be used to diagnose.
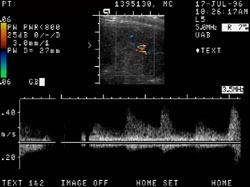
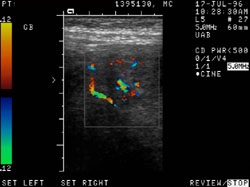
Ultrasonography
-
Gallbladder cancer: 88 year old female with epigastric pain, nausea and vomiting. Soft tissue mass lesion arising from the anterior wall of the gallbladder and extending into the gallbladder lumen.
-
Gallbladder cancer: 88 year old female with epigastric pain, nausea and vomiting. This has the appearance of a neoplasm, most likely a primary carcinoma of the gallbladder.
-
Gallbladder cancer: 88 year old female with epigastric pain, nausea and vomiting. Metastatic lesion or lymphoma are less likely considerations. There is no definite sonographic evidence of extension of the mass outside the gallbladder nor of regional adenopathy.
-
Gallbladder cancer: 88 year old female with epigastric pain, nausea and vomiting. Bilateral renal cysts, with that in the left upper pole categorized as a Bosniak type II cyst.
Stage Information
- TNM Definitions
- AJCC Stage Groupings
The American Joint Committee on Cancer (AJCC) has designated staging by the TNM classification as follows:[5]
TNM Definitions
Primary tumor (T)
- TX: Primary tumor cannot be assessed
- T0: No evidence of primary tumor
- Tis: Carcinoma in situ
- T1: Tumor invades lamina propria or muscle layer
- T1a: Tumor invades lamina propria
- T1b: Tumor invades the muscle layer
- T2: Tumor invades the perimuscular connective tissue; no extension beyond the serosa or into the liver
- T3: Tumor perforates the serosa (visceral peritoneum) and/or directly invades the liver and/or one other adjacent organ or structure, such as the stomach, duodenum, colon, or pancreas, omentum or extrahepatic bile ducts
- T4: Tumor invades main portal vein or hepatic artery or invades multiple extrahepatic organs or structures
Regional lymph nodes (N)
- NX: Regional lymph nodes cannot be assessed
- N0: No regional lymph node metastasis
- N1: Regional lymph node metastasis
Distant metastasis (M)
- MX: Distant metastasis cannot be assessed
- M0: No distant metastasis
- M1: Distant metastasis
AJCC Stage Groupings
Stage 0
- Tis, N0, M0
Stage IA
- T1, N0, M0
Stage IB
- T2, N0, M0
Stage IIA
- T3, N0, M0
Stage IIB
- T1, N1, M0
- T2, N1, M0
- T3, N1, M0
Stage III
- T4, any N, M0
Stage IV
- Any T, any N, M1
Localized (Stage I)
These types of patients have cancer confined to the gallbladder wall that can be completely resected. They represent a minority of cases of gallbladder cancer. Patients with cancers confined to the mucosa have 5-year survival rates of nearly 100%.[6]
Patients with muscular invasion or beyond have a survival of less than 15%. Regional lymphatics and lymph nodes should be removed along with the gallbladder in such patients.
Unresectable (Stage II–IV)
With the exception of some patients with focal stage IIA disease, these types of patients have cancer that cannot be completely resected. They represent the majority of cases of gallbladder cancer. Often the cancer invades directly into adjacent liver or biliary lymph nodes or has disseminated throughout the peritoneal cavity. Spread to distant parts of the body is not uncommon. At this stage, standard therapy is directed at palliation. Because of its rarity, no specific clinical trials exist; however, such patients can be included in trials aimed at improving local control by combining radiation therapy with radiosensitizer drugs.
Localized Gallbladder Cancer
Localized gallbladder cancer is defined by the following TNM classification:
- Tis, T1a or b, selected T2, rare T3; N0; M0
When gallbladder cancer is previously unsuspected and is discovered in the mucosa of the gallbladder at pathologic examination, it is curable in more than 80% of cases. Gallbladder cancer suspected before surgery because of symptoms, however, usually penetrates the muscularis and serosa and is curable in fewer than 5% of patients.
One study reported on patterns of lymph node spread from gallbladder cancer and outcomes of patients with metastases to lymph nodes in 111 consecutive surgical patients in a single institution from 1981 to 1995.[7] [Level of evidence: 3iiiA] The standard surgical procedure was removal of the gallbladder, a wedge resection of the liver, resection of the extrahepatic bile duct, and resection of the regional (N1 and N2) lymph nodes. Kaplan-Meier estimates of the 5-year survival for node negative tumors pathologically staged as T2 to T4 were 42.5% ± 6.5% and for similar node positive tumors, 31% ± 6.2%.
Standard treatment options:
Surgery:
In previously unsuspected gallbladder cancer, discovered in the surgical specimen following a routine gallbladder operation and confined to mucosa or muscle layer (T1), the majority of patients are cured and require no further surgical intervention.[8] [9] Re-exploration to resect liver tissue near the gallbladder bed or extended or formal hepatectomy and lymphadenectomy including N1 and N2 lymph node basins may be associated with delayed recurrences or extended survival in patients with stage I or II gallbladder cancer.[10] [11] Apparently localized cancers that are suspected before or during the operation can be surgically removed with a wedge of liver and lymph nodes and lymphatic tissue in the hepatoduodenal ligament. Long-term disease-free survival will occasionally be achieved. In jaundiced patients (stage III or stage IV), there should be consideration of preoperative percutaneous transhepatic biliary drainage for relief of biliary obstruction.
Implantation of the carcinoma at all port sites (including the camera site) after laparoscopic removal of an unsuspected cancer is a problem. Even for stage I cancers, the port sites must be excised completely.[12]
External-beam radiation therapy (EBRT):
The use of EBRT with or without chemotherapy as a primary treatment has been reported in small groups of patients to produce short-term control. Similar benefits have been reported for radiation therapy with or without chemotherapy administered following resection. [13] [14]
Treatment options under clinical evaluation:
Clinical trials are exploring ways of improving local control with radiation therapy combined with radiosensitizer drugs. When possible, such patients are appropriately considered candidates for these studies.
Unresectable Gallbladder Cancer
Unresectable gallbladder cancer is defined by the following TNM classification:
- Any T, N1, M0
- Any T, N0 or N1, M1
- Most T3, N0, M0
- T4, N0, M0
These patients are not curable. Significant symptomatic benefit can often be achieved with relief of biliary obstruction. A few patients have very slow-growing tumors and may live several years.
Standard treatment options:
Palliative treatment options may include the following:
- The preferred approach to biliary obstruction is percutaneous transhepatic radiologic catheter bypass or endoscopically placed stents.[15]
- Standard external-beam radiation therapy can, on occasion, alleviate biliary obstruction in some patients and may supplement bypass procedures.
- Palliative surgery may relieve bile duct obstruction and is warranted when symptoms produced by biliary blockade (pruritus, hepatic dysfunction, and cholangitis) outweigh other symptoms from the cancer.
- Standard chemotherapy is usually not effective, though occasional patients may be palliated. Clinical trials should be considered as a first option for most patients. [16] [17]
Treatment options under clinical evaluation:
Clinical trials are in progress to improve local control rates by radiation therapy using brachytherapy and/or radiosensitizer drugs or to discover more effective forms of chemotherapy. When possible, patients should be considered for these clinical trials.
Recurrent Gallbladder Cancer
The prognosis for any treated cancer patient with progressing or recurrent gallbladder cancer is poor. The question and selection of further treatment depends on many factors: tumor burden, prior treatment, site of recurrence, and individual patient considerations. Patients may have portal hypertension caused by portal vein compression by the tumor. Transperitoneal and intrahepatic metastases are not uncommon. Clinical trials are appropriate and should be considered when possible.
General Management of Gallbladder Cancers
In patients whose superficial cancer (T1 or confined to the mucosa) is discovered on pathological examination of tissue after gallbladder removal for other reasons, the disease is often cured without further therapy. In patients who present with symptoms, the tumor is rarely diagnosed preoperatively.[18] In such cases, the tumor often cannot be removed completely by surgery and the patient cannot be cured, though palliative measures may be beneficial. For patients with T2 or greater disease, extended resection with partial hepatectomy and portal node dissection may be an option.[19] [20]
Pathological Findings
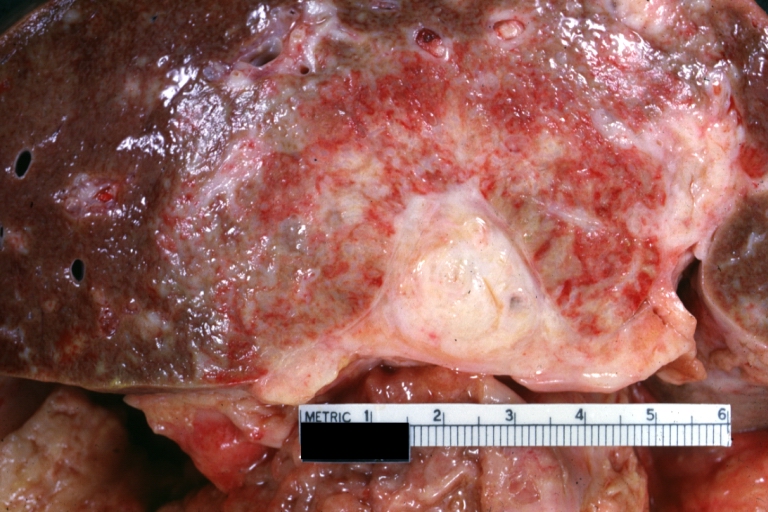
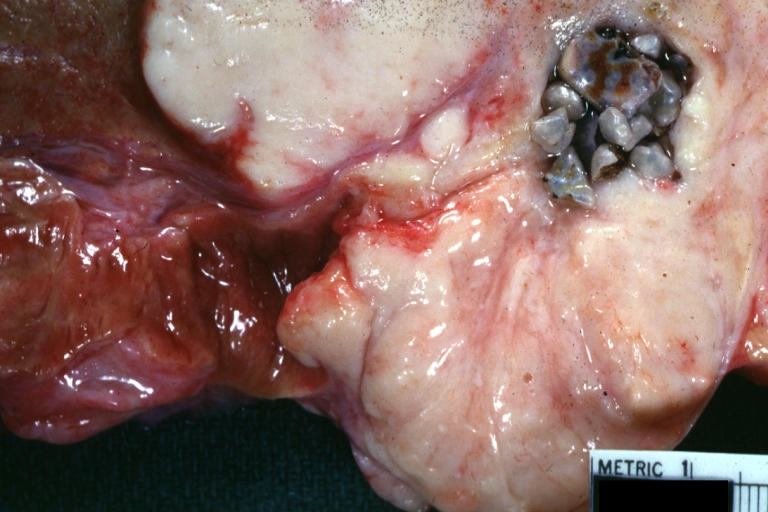
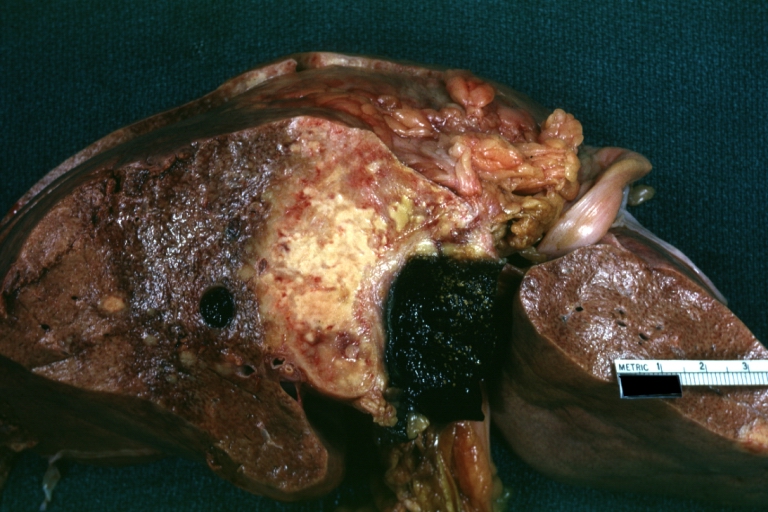
Gross Images
-
Gallbladder carcinoma: Gross, natural color, close-up view of liver and gallbladder slice with typical neoplasm invading liver and surround a cavity with mixed type gallstones
-
Gallbladder carcinoma: Gross, natural color close-up view of gallbladder obliterated by white neoplasm with invasion of liver in a sunburst pattern slice of liver and gallbladder (an outstanding example of this rather rare tumor)
-
Gallbladder carcinoma: Gross, natural color shows stones in middle of tumor localization
-
Gallbladder carcinoma: Gross, natural color slab of liver with gallbladder
-
Gallbladder: Adenocarcinoma, arising from bile ducts
-
Gallbladder carcinoma: Gross, natural color of slice of liver showing attached gallbladder obliterated by tumor and with tumor invading adjacent liver parenchyma like a sunburst (an excellent example)
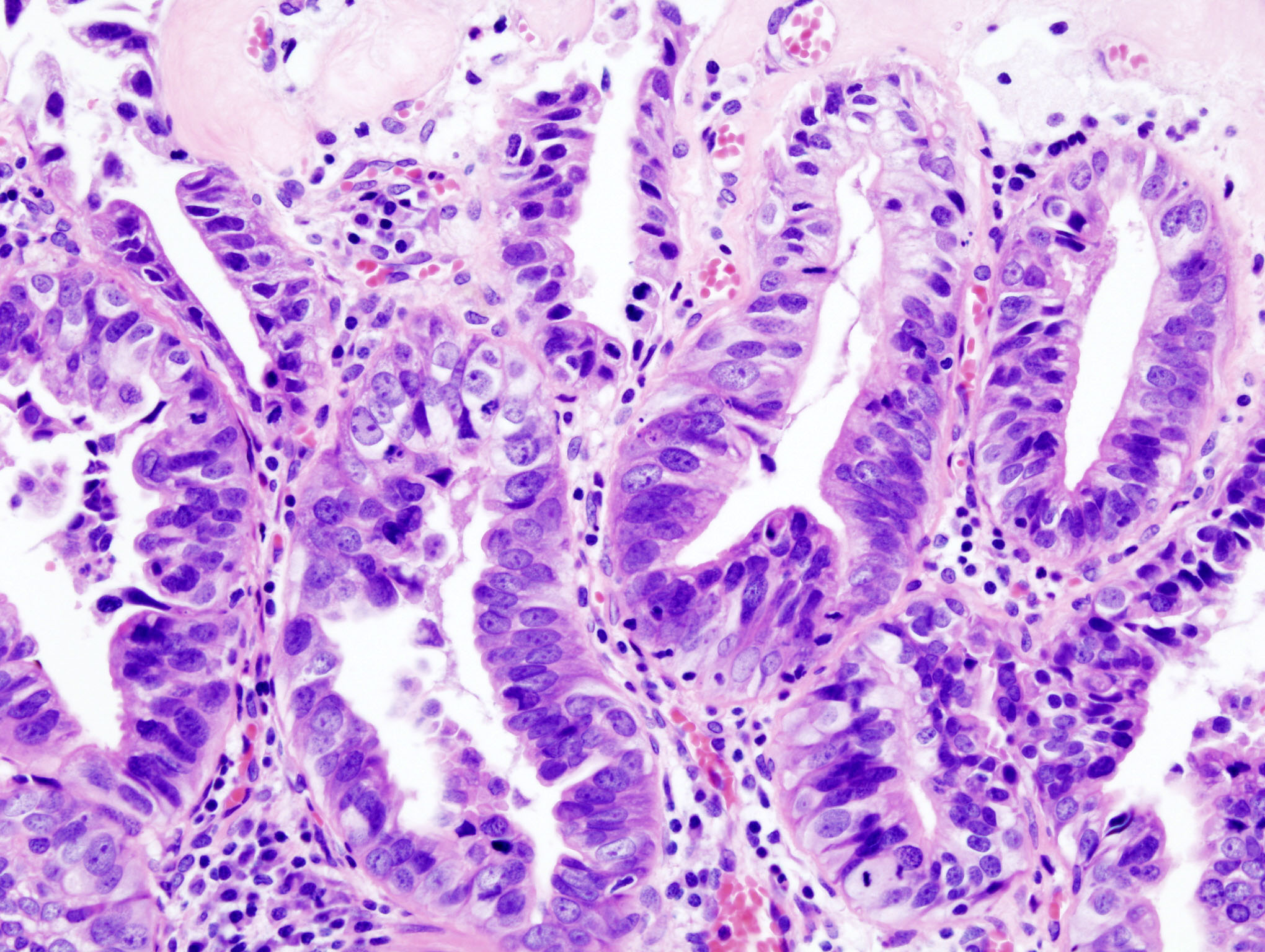
Microscopic Images
-
Gallbladder adenocarcinoma histopathology
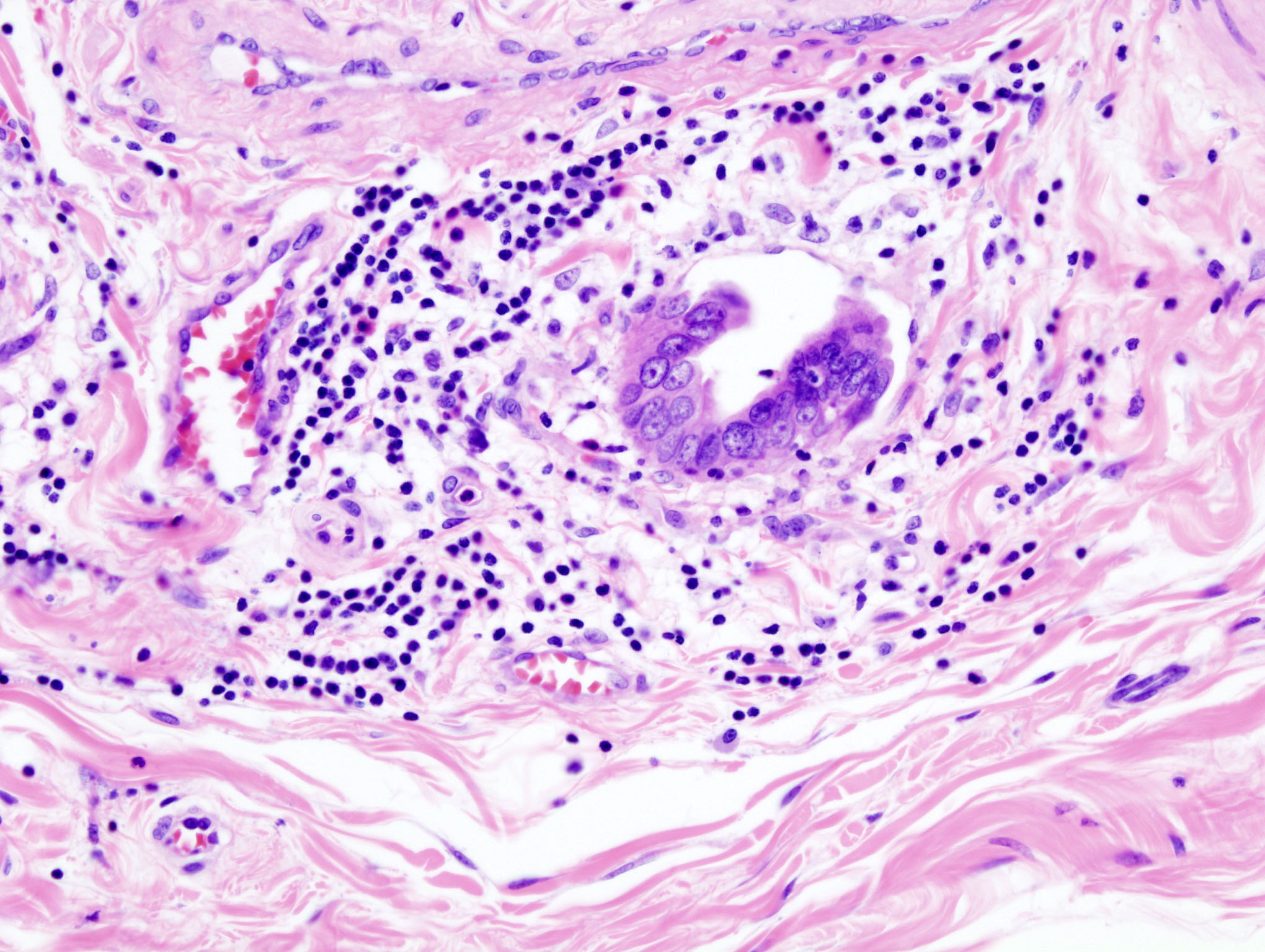
-
Gallbladder adenocarcinoma: Lymphatic invasion histopathology
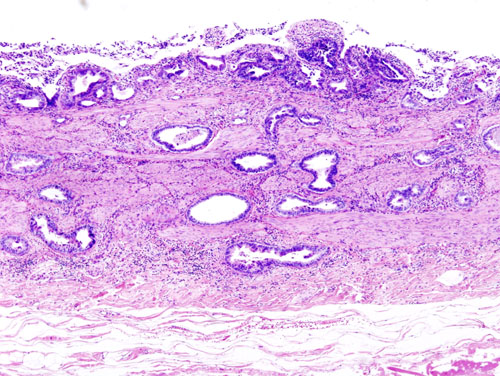
-
Gallbladder adenocarcinoma: Incidentally discovered gallbladder cancer (adenocarcinoma) following a cholecystectomy. H&E stain
References
- ↑ American Cancer Society.: Cancer Facts and Figures 2008. Atlanta, Ga: American Cancer Society, 2008.
- ↑ Gallbladder. In: American Joint Committee on Cancer.: AJCC Cancer Staging Manual. 6th ed. New York, NY: Springer, 2002, pp 139-44.
- ↑ Ji, J (2005 Sep). "Variation in the risk for liver and gallbladder cancers in socioeconomic and occupational groups in Sweden with etiological implications". Int Arch Occup Environ Health. 78 (8): 641–9. PMID 16001211. Retrieved 28 May 2007. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Ji J, Couto E, Hemminki K. Incidence differences for gallbladder cancer between occupational groups suggest an etiological role for alcohol Int J Cancer 2005 Sep 1;116(3):492-3.
- ↑ Gallbladder. In: American Joint Committee on Cancer.: AJCC Cancer Staging Manual. 6th ed. New York, NY: Springer, 2002, pp 139-44.
- ↑ Shirai Y, Yoshida K, Tsukada K, et al.: Inapparent carcinoma of the gallbladder. An appraisal of a radical second operation after simple cholecystectomy. Ann Surg 215 (4): 326-31, 1992.
- ↑ Tsukada K, Kurosaki I, Uchida K, et al.: Lymph node spread from carcinoma of the gallbladder. Cancer 80 (4): 661-7, 1997.
- ↑ Fong Y, Brennan MF, Turnbull A, et al.: Gallbladder cancer discovered during laparoscopic surgery. Potential for iatrogenic tumor dissemination. Arch Surg 128 (9): 1054-6, 1993.
- ↑ Chijiiwa K, Tanaka M: Carcinoma of the gallbladder: an appraisal of surgical resection. Surgery 115 (6): 751-6, 1994.
- ↑ Shirai Y, Yoshida K, Tsukada K, et al.: Inapparent carcinoma of the gallbladder. An appraisal of a radical second operation after simple cholecystectomy. Ann Surg 215 (4): 326-31, 1992
- ↑ Yamaguchi K, Chijiiwa K, Saiki S, et al.: Retrospective analysis of 70 operations for gallbladder carcinoma. Br J Surg 84 (2): 200-4, 1997.
- ↑ Wibbenmeyer LA, Wade TP, Chen RC, et al.: Laparoscopic cholecystectomy can disseminate in situ carcinoma of the gallbladder. J Am Coll Surg 181 (6): 504-10, 1995.
- ↑ Smoron GL: Radiation therapy of carcinoma of gallbladder and biliary tract. Cancer 40 (4): 1422-4, 1977.
- ↑ Hejna M, Pruckmayer M, Raderer M: The role of chemotherapy and radiation in the management of biliary cancer: a review of the literature. Eur J Cancer 34 (7): 977-86, 1998.
- ↑ Baron TH: Expandable metal stents for the treatment of cancerous obstruction of the gastrointestinal tract. N Engl J Med 344 (22): 1681-7, 2001.
- ↑ Bartlett DL, Ramanathan RK, Deutsch M: Cancer of the biliary tree. In: DeVita VT Jr, Hellman S, Rosenberg SA, eds.: Cancer: Principles and Practice of Oncology. 7th ed. Philadelphia, Pa: Lippincott Williams & Wilkins, 2005, pp 1009-31.
- ↑ Hejna M, Pruckmayer M, Raderer M: The role of chemotherapy and radiation in the management of biliary cancer: a review of the literature. Eur J Cancer 34 (7): 977-86, 1998.
- ↑ Chao TC, Greager JA: Primary carcinoma of the gallbladder. J Surg Oncol 46 (4): 215-21, 1991.
- ↑ Shoup M, Fong Y: Surgical indications and extent of resection in gallbladder cancer. Surg Oncol Clin N Am 11 (4): 985-94, 2002.
- ↑ Sasson AR, Hoffman JP, Ross E, et al.: Trimodality therapy for advanced gallbladder cancer. Am Surg 67 (3): 277-83; discussion 284, 2001.
Additional Resources
- Lewis, S.M., Heitkemper, M.M., & Dirksen, S.R. Medical-Surgical Nursing: Assessment and Management of Clinical Problems, 6th ed. St. Louis: Mosby, 2004.
- McCance,K., & Huether, S. Pathophysiology: The Biologic Basis for Disease in Adults & Children, 4th ed. St. Louis: Mosby, 2002.
- Gallbladder cancer at National Cancer Institute of USA
External Links
- Beth Israel Deaconess Medical Center: Gallbladder cancer
- Gallbladder adenocarcinoma case examples
- Gallbladder adenocarcinoma at Virtual Pathology Museum
- Well-differentiated adenocarcinoma of the gallbladder mimicking minimal deviation adenocarcinoma of the cervix: Case report
- Adenocarcinoma of the gallbladder--a 5 year review of outcome in Newcastle upon Tyne
- Aggressive adenocarcinoma of gallbladder with distant metastases and venous thrombosis at initial presentation
- A human gallbladder adenocarcinoma cell line
Template:Digestive system neoplasia Template:Tumors Template:SIB sv:Gallblåsecancer