Fournier gangrene: Difference between revisions
Megan Merlo (talk | contribs) |
|||
| Line 562: | Line 562: | ||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
Fournier gangrene is a urological emergency requiring [[intravenous]] antibiotics and [[debridement]] (surgical removal) of necrotic (dead) tissue. Despite such measures, the mortality rate overall is 40%, but 78% if [[sepsis]] is already present at the time of initial hospital admission.<ref name="Yanar2006"/>The spread of gangrene is rapid at the rate of 2–3 cm/h, hence early diagnosis and emergency surgical treatment is of very importance.<ref name="pmid1736475">{{cite journal| author=Paty R, Smith AD| title=Gangrene and Fournier's gangrene. | journal=Urol Clin North Am | year= 1992 | volume= 19 | issue= 1 | pages= 149-62 | pmid=1736475 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1736475 | Fournier gangrene is a urological emergency requiring [[intravenous]] antibiotics and [[debridement]] (surgical removal) of necrotic (dead) tissue. Despite such measures, the mortality rate overall is 40%, but 78% if [[sepsis]] is already present at the time of initial hospital admission.<ref name="Yanar2006"/>The spread of gangrene is rapid at the rate of 2–3 cm/h, hence early diagnosis and emergency surgical treatment is of very importance.<ref name="pmid1736475">{{cite journal| author=Paty R, Smith AD| title=Gangrene and Fournier's gangrene. | journal=Urol Clin North Am | year= 1992 | volume= 19 | issue= 1 | pages= 149-62 | pmid=1736475 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1736475 }}</ref> | ||
====Antimicrobial Therapy==== | ====Antimicrobial Therapy==== | ||
* Fournier gangrene<ref>{{cite book | last = Gilbert | first = David | title = The Sanford guide to antimicrobial therapy | publisher = Antimicrobial Therapy | location = Sperryville, Va | year = 2015 | isbn = 978-1930808843 }}</ref> | * Fournier gangrene<ref>{{cite book | last = Gilbert | first = David | title = The Sanford guide to antimicrobial therapy | publisher = Antimicrobial Therapy | location = Sperryville, Va | year = 2015 | isbn = 978-1930808843 }}</ref> | ||
Revision as of 15:29, 3 February 2017
For more information about necrotizing fasciitis click here
|
WikiDoc Resources for Fournier gangrene |
|
Articles |
|---|
|
Most recent articles on Fournier gangrene Most cited articles on Fournier gangrene |
|
Media |
|
Powerpoint slides on Fournier gangrene |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Fournier gangrene |
|
Clinical Trials |
|
Ongoing Trials on Fournier gangrene at Clinical Trials.gov Trial results on Fournier gangrene Clinical Trials on Fournier gangrene at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Fournier gangrene NICE Guidance on Fournier gangrene
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Fournier gangrene Discussion groups on Fournier gangrene Patient Handouts on Fournier gangrene Directions to Hospitals Treating Fournier gangrene Risk calculators and risk factors for Fournier gangrene
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Fournier gangrene |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Steven C. Campbell, M.D., Ph.D.; Associate Editor(s)-in-Chief: Yamuna Kondapally, M.B.B.S[1]; Jesus Rosario Hernandez, M.D. [2]
Synonyms and keywords: Fournier's gangrene; Idiopathic gangrene of scrotum; Periurethral phlegmon; Streptococcal scrotal gangrene; Genito-perineal gangrene; Phagedena
| Fournier gangrene | |
| ICD-10 | N49.8 (ILDS N49.81), N76.8 |
|---|---|
| ICD-9 | 608.83 |
| DiseasesDB | 31119 |
| MeSH | D018934 |
Overview
Fournier gangrene is a type of synergistic polymicrobial necrotizing infection (gangrene) of the perineal, genital or perianal regions usually affecting the male genitals but can also occur in females and children.[1] It is a fulminant form of necrotizing fasciitis. It was first described by Baurienne in 1764 and is named after a French venereologist, Jean Alfred Fournier following five cases he presented in clinical lectures in 1883.[2][3]
Historical Perspective
- Fournier gangrene was first described in 1764 by Baurienne.[2]
- The detailed description of Fournier gangrene was given by Jean Alfred Fournier, a French venereologist, in 1883.[3]
Classification
The ICD 10 classification of Fournier gangrene include:[4]
- ICD-10: N49.3
- Code Classification
- Diseases of the genitourinary system
Pathophysiology
The transmission of pathogens occurs through the following routes:[5]
- External trauma (e.g., laceration, abrasion, burn, insect bite)
- Direct spread from a perforated viscus (particularly colon, rectum, or anus) or another surgical procedure (e.g., vasectomy, hemorrhoidectomy)
- Urogenital organ
- Perirectal abscess
- Decubitus ulcer
Following transmission, the bacteria uses the entry site to invade the fascial planes which causes the wide spread necrosis of superficial fascia, deep fascia, subcutaneous fat, nerves, arteries, and veins. Superficial skin and deeper muscles are typically spared. In late stages, lesions develop liquefactive necrosis at all tissue levels.
Pathogenesis
- The pathogenesis of Fournier gangrene is the result of an imbalance between bacterial and host factors.[6][7][5]
- The aerobic and anaerobic bacteria produce exotoxins and enzymes, such as collagenase, heparinase, and hyaluronidase, which promote the spread of infection.
- The aerobic bacteria accelerate coagulation by promoting platelet aggregation and complement fixation and the anaerobic bacteria produce collagenase and heparinase that promote the formation of clots leading to Obliterating endarteritis.
- The development of cutaneous and subcutaneous vascular necrosis leads to local ischemia and further bacterial proliferation.
- The infection spreads from superficial (colles fascia) and deep fascial planes of genitalia to the overlying skin sparing the muscles. The infection then spreads from colles fascia to the penis and scrotum via Buck's and Dartos fascia or to the anterior abdominal wall via Scarpa's fascia or vice versa.
- The inferior epigastric and deep circumflex iliac arteries supply the anterior abdominal wall, and the deep external pudendal and internal pudendal arteries supply the scrotal wall. Except for the internal pudendal artery, each of these vessels travels within Camper's fascia and can therefore become thrombosed in the progression of Fournier gangrene.
- The progression of infection to the perineal body, urogenital diaphragm and pubic rami is limited due to perineal fascia.[8]
- Because of the direct supply of blood from the aorta, testicular involvement is limited in Fournier gangrene.[9] However involvement of testis suggests retroperitoneal origin or spread of infection.[10]
- Fournier gangrene of the male genetalia spares testes, urethra and deep penile tissues while the skin sloughs off.[11]
- Sepsis and multiorgan failure is the most common cause of death in Fournier gangrene.
Common locations
The common locations of Fournier gangrene are:[7]
Gross pathology
On gross pathology, the characteristic findings of Fournier gangrene include:
- Subcutaneous emphysema
- Swollen scrotal wall
- Edema
- Erythema
- Bullae
- Skin sloughing
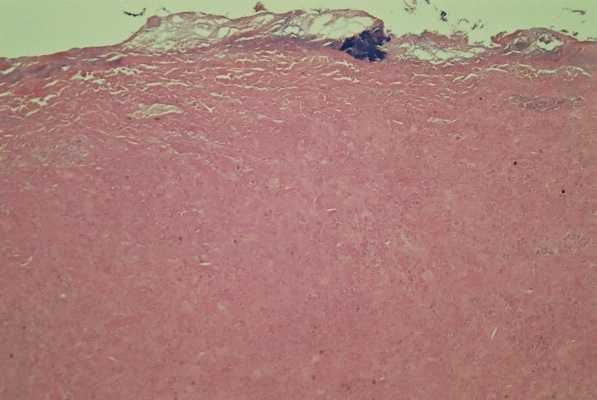
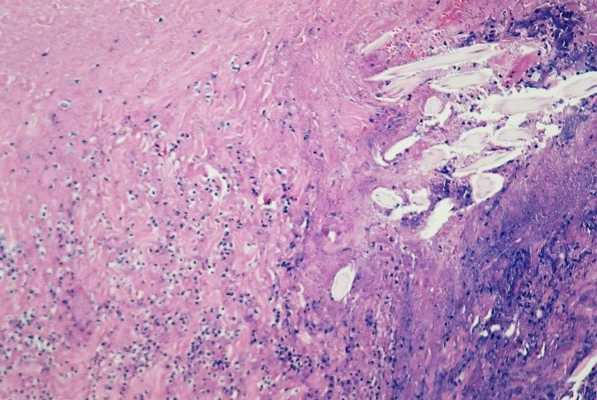
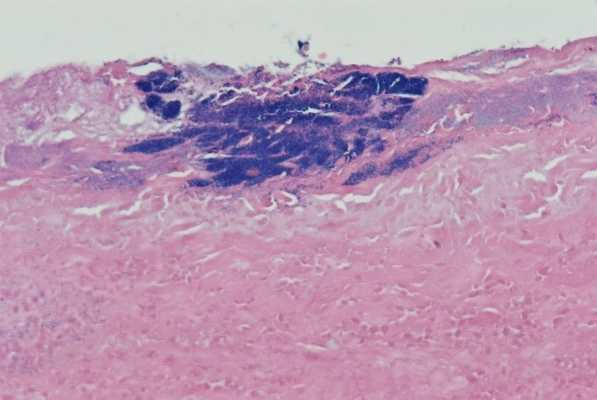
Microscopic histopathological analysis
On microscopic histopathological analysis, the characteristic findings of Fournier gangrene are:
- Early stages
- Obliterative vasculitis with microangiopathic thrombosis
- Acute inflammation of subcutaneous tissue
- Superficial hyaline necrosis along with edema and inflammation of the dermis and subcutaneous fat
- Dense neutrophil-predominant inflammatory infiltrate
- Late stages
- Noninflammatory intravascular coagulation and hemorrhage
- Myonecrosis
-
Histology of excised skin shows full thickness, featureless, coagulative necrosis with no viable tissue remaining
-
Histology of excised scrotal skin shows zones of neutrophil polymorph infiltration, with embedded foreign material possibly representing hair shafts
Causes
Fournier gangrene is caused by mixed aerobic and anaerobic organisms which normally exist below the pelvic diaphragm in the perineum and genitalia.[12] Fournier gangrene may be caused by the following organisms:[13]
Bacteria
Aerobic organisms
Most common aerobic organisms are:[14]
Anaerobic organisms
Most common anaerobic organisms are:
Other organisms
- Streptococcus
- Enterococcus
- Corynebacterium[15]
- Clostridium
- Pseudomonas
- proteus species
- Candida species[16]
- Lactobacillus gasseri[17]
Idiopathic
Less than quarter of cases of Fournier gangrene are idiopathic.[1][18]
Differentiating Fournier gangrene from Other Diseases
Fournier gangrene must be differentiated from other diseases that cause pain, swelling, erythema, discharge and raised temperature (fever) such as:[19][5]
- Scrotal abscess
- Herpes simplex
- Cellulitis
- Strangulated hernia
- Streptococcal necrotizing fasciitis
- Gonococcal balanitis and edema
- Vascular occlusion syndromes
- Allergic vasculitis
- Pyoderma gangrenosum
- Necrolytic migratory erythema
- Ecthyma gangrenosum
- Warfarin necrosis
- Polyarteritis nodosa
Epidemiology and Demographics
Incidence
Incidence of Fournier gangrene in the United states:[20]
- The overall incidence of Fournier gangrene annually are 1.6 cases per 100,000 males.The incidence peaked and remained steady after age 50 at 3.3 cases per 100,000 males.
- The incidence of Fournier gangrene increased 0.2 per 100,000 males for each 1% increase in the regional prevalence of diabetes.
- The incidence rate was highest in the south and the lowest in the west and Midwest US.
-
Distribution of annual cases per hospital.[20]
Age
Fournier gangrene affects individuals of all ages but commonly affects individuals older than 50 years of age.[5][7]
Gender
Men are more commonly affected with Fournier gangrene than women (male:female ratio is 10:1).[3][7]
Mortality
- Mortality rate decreases with early aggressive treatment.
- The mortality rate of Fournier gangrene is between 20% to 80%. Higher mortality rates are found in daibetics, alcoholics and those with colorectal sources of infection.[21]
Risk Factors
Common risk factors in the development of Fournier gangrene are:[22][23][18]
- Comorbid systemic disorders
- Age>50 yrs
- Male Gender
- Diabetes mellitus
- Alcohol misuse
- Immunosupression
- Chemotherapy
- Chronic corticosteroid use
- HIV
- Leukemia
- Liver disease
- Debilitating illness
- Malignancy
- Cytotoxic drugs
The most common foci of Fournier gangrene include:[12][24]
| Anorectal | Genitourinary | Dermatology | Gynaecological |
|---|---|---|---|
|
|
|
Neonates and Children
- Trauma[24]
- Burns
- Insect bites
- Circumcision
Screening
According to the U.S. Preventive Service Task Force (USPSTF), there is insufficient evidence to recommend routine screening for Fournier gangrene.
Natural History, Complications, and Prognosis
Natural history
- If left untreated, the acute inflammatory changes spread quickly, accompanied by high fever and extreme weakness.[25][26]
- The overlying skin becomes smooth, tense and shiny. Diffuse erythema without distinct borders is seen.
- First 1 or 2 days, the lesions develop with progressive colour changes from red to purple to blue and then becomes frankly gangrenous, first turning black, then greenish yellow.
- If the patient has survived, a line of demarcation between viable and necrotic tissue would become sharply defined from days 7 to 10.
- Sloughing of necrotic skin would reveal the underlying pus and extensive liquefactive necrosis of subcutaneous tissues, which will be significantly more extensive than would be suspected with the overlying area of necrotic skin.
- Metastatic abscesses and pulmonary distress may develop as well.
Complications
Common complications of Fournier gangrene include:[27][28]
Systemic complications
- Renal failure
- Acute respiratory distress syndrome
- Heart failure
- Cardiac arrhythmias
- Septic metastasis
- Urinary tract infection
- Stroke
- Acute thromboembolic disease of lower extremities
Surgical complications
Long term complications
- Pain (50% of patients)
- Impaired sexual function (due to penile deviation/torsion, loss of sensitivity of the penile skin or pain during erection)
- Stool incontinence
- Extensive scarring
Prognosis
Depending on the underlying comorbidities, the prognosis of Fournier gangrene varies. Few of the prognostic factors include:
- Severe sepsis
- Affected area calculation/extension of the necrosis
- <3% of body surface area rarely die
- ≥5% of body surface area have worse prognosis
Diagnosis
The diagnosis of Fournier gangrene is primarily based on clinical findings. The diagnosis is based on following criteria:[29]
- Soft tissue infections with involvement of the scrotum, perineum and perianal areas
- Presence of air infiltrating the subcutaneous tissue (demonstrated by physical examination or radiological findings)
- Surgical findings of gangrenous and necrotic tissue
- Histologically proven necrotising fasciitis.
Diagnostic Criteria
The Uludag Fournier gangrene severity index
| Physiologic Variables | High Abnormal Values | Normal | Low Abnormal Values | ||||||
|---|---|---|---|---|---|---|---|---|---|
| +4 | +3 | +2 | +1 | 0 | +1 | +2 | +3 | + 4 | |
| Temperature | >41 | 39-40.0 | 38.5-39 | 36-38.4 | 34-35.9 | 32-33.9 | 30-31.9 | <29.9 | |
| Heart Rate | >180 | 140-179 | 110-139 | 70-109 | 55-69 | 40-54 | <39 | ||
| Respiratory Rate | >50 | 35-49 | 25-34 | 12-24 | 10-11 | 6-9 | <5 | ||
| Serum Sodium (mmol/L) | >180 | 160-179 | 155-159 | 150-154 | 130-149 | 120-129 | 111-119 | <110 | |
| Serum Potassium (mmol/L) | >7 | 6-6.9 | 5.5-5.9 | 3.5-5.4 | 3-3.4 | 2.5-2.9 | <2.5 | ||
| Serum Creatinine (mg/100/ml*2 for acute renal failure) |
>3.5 | 2-3.4 | 1.5-1.9 | 0.6-1.4 | <0.6 | ||||
| Hematocrit | >60 | 50-59.9 | 46-49.9 | 30-45.9 | 20-29.9 | <20 | |||
| WBC (Total/mm*1000) | >40 | 20-39.9 | 15-19.9 | 3-14.9 | 1-2.9 | <1 | |||
| Serum Bicarbonate (Venous,mmol/l) | >52 | 41-51.9 | 32-40.9 | 22-31.9 | 18-21.9 | 15-17.9 | <15 | ||
- Score >10.5 indicates 96% probability of death[30]
- Score ≤10.5 indicates 96% probability of survival
According to Loar and colleagues, the severity of Fournier gangrene is:
- Score ≥9 indicates 46% probability of death
- Score <9 indicates 96% probability of survival
Laboratory risk indicator for necrotizing fasciitis (LRINEC) scoring system
- LRINEC is a diagnostic scoring system used to distinguish necrotizing fasciitis from other soft tissue infections.[31][5]
- It was first established by Wong et al in 2004.
- Risk assessment of necrotizing faciitis using LRINEC score:
- Low risk: ≤5
- Intermediate risk: 6-7
- High risk: ≥8
| Variable | Score |
|---|---|
| C reactive protein (mg/dL)
<150 |
0 |
| Total white blood cell count (/mm3)
<15 |
0 |
| Hemoglobin (g/dL)
<13.5 |
0 |
| Sodium (mmol/L)
≥135 |
0 |
| Creatinine (μmol/L)
<141 |
0 |
| Glucose (mmol/L)
<10 |
0 |
History
A detailed and thorough history from the patient is necessary. Specific areas of focus when obtaining a history from the patient include:[22][23][18]
- Trauma
- Alcohol misuse
- Immunosupression
- Chemotherapy
- Chronic corticosteroid use
- HIV
- Leukemia
- Liver disease
- Debilitating illness
- Malignancy
- Cytotoxic drugs
- Abdominal disease
- Surgery
- Epididymitis or orchitis
Symptoms
The symptoms of Fournier gangrene include:[5][32]
- Pain and swelling in the scrotum
- Erythema
- Discoloration of involved skin
- Purulence or wound discharge
- Pallor
- Fever>38°C
- Crepitation
- Prostration
- Fluctuance
- Fetid odour
Physical examination
The physical examination of Fournier gangrene include:
Appearance of the Patient
The patients with Fournier gangrene are usually ill appearing.
Vitals
- Fever (is often absent)
- Tachycardia
- Low blood pressure
- Tachypnea
Skin
- Jaundice
- Evidence of trauma, surgery, insect or human bites, or injection sites
Local examination
Local examination of patient under local anesthesia includes palpation of genitalia and perineum, and digital rectal examination.
- Induration
- Warmth
- Tenderness beyond margins of erythema
- Swelling
- Erythema with ill defined margins
- Blistering/bullae
- Skin discoloration
- Foul discharge (greyish or brown discharge)
- Fluctuance
- Crepitus
- Skin sloughing or necrosis
- Absence of lymphangitis or lymphadenopathy (lymphangitis is rarely seen in Fournier gangrene)
- Sensory and motor deficits (e.g. localized anesthesia)
Images
Genitourinary system
-
Fournier gangrene. [34]
-
Fournier gangrene. [34]
-
Fournier gangrene. [34]
-
Fournier gangrene. [34]
-
Fournier gangrene. [34]
Laboratory Findings
Laboratory findings consistent with the diagnosis of Fournier gangrene include:
- CBC with differential count
- Culture of open wound or abscess
- Disseminated intravascular coagulation panel
- Coagulation studies(PT, aPTT, thrombin time etc)
- Fibrinogen/fibrin degradation product levels
- Blood culture
- Urine culture
- Arterial blood gas analysis
- Electrolyte panel
- Blood urea nitrogen (BUN)
- Creatinine
- Blood glucose levels
Imaging Findings
The diagnosis of Fournier gangrene is based on clinical findings.The role of imaging includes:[19]
- Diagnosis not established
- Determine the extent of disease
- Detect underlying cause
Radiography
- On X-ray, Fournier gangrene is characterized by:[19]
- Subcutaneous gas or soft tissue swelling (specific x-ray finding) seen extending from scrotum and perineum to the inguinal regions, anterior abdominal wall, and thighs.
- Increase in the soft tissue thickness and opacity.
- Plain x-ray is a poor screening study for Fournier gangrene because:
- Subcutaneous emphysema is an insensitive finding and is present in a minority of patients
- In the early stages the findings are similar to cellulitis
Ultrasound
On ultrasound, Fournier gangrene is characterized by:[5][35]
- Thickened scrotal wall
- Echogenic gas foci in scrotum pathognomonic-Seen as dirty shadowing
- Testes and epididymi spared (due to their separate blood supply)
- Reactive unilateral or bilateral hydroceles are present
- Differentiate Fournier gangrene from inguinoscrotal incarcerated hernia (In inguinoscrotal incarcerated hernia gas is observed in the obstructed bowel lumen, away from the scrotal wall)
Computed tomography
The CT of Fournier gangrene is characterized by:[19]
- Soft tissue stranding and fascial thickening
- Soft tissue gas
- The extent of disease can be assessed prior to surgery
- A cause of infection may be apparent (e.g.perineal abscess, fistula)
MRI
On MRI, Fournier gangrene is characterized by:[36]
- Edema and inflammation of skin and subcutaneous planes of the scrotum and perineal planes
- Subcutaneous emphysema
Gallery of Imaging Findings
-
X ray of Fournier gangrene [19]
-
Ultrasound of Fournier gangrene [19]
-
CT of Fournier gangrene [19]
-
CT of Fournier gangrene with spontaneous perforation of rectal cancer [19]
Treatment
Medical Therapy
Fournier gangrene is a urological emergency requiring intravenous antibiotics and debridement (surgical removal) of necrotic (dead) tissue. Despite such measures, the mortality rate overall is 40%, but 78% if sepsis is already present at the time of initial hospital admission.[37]The spread of gangrene is rapid at the rate of 2–3 cm/h, hence early diagnosis and emergency surgical treatment is of very importance.[14]
Antimicrobial Therapy
- Fournier gangrene[38]
- If caused by streptococcus species or clostridia
- Preferred regimen: Penicillin G
- Polymicrobial
-
- MRSA (methicillin resistant staphylococcus aureus) suspected
- Preferred regimen: vancomycin OR daptomycin
Nutritional Support
- The metabolic demands of Fournier gangrene patients are similar to those of other major trauma or burns.[39]
- Nutritional support to replace lost proteins and fluids from large wounds and/or the result of shock is required from the first day of patients hospital admission.
Hyperbaric oxygen
- Delivery of 100% oxygen (hyperbaric) at two or three times the atmospheric pressure for 30 to 90 minutes with three to four treatments daily.[40]
- Hyperbaric oxygen inhibits infection and exotoxin release.[41]
- It enhances efficacy of antibiotics by increasing local oxygen tension in tissue and augment oxidative burst and killing ability of leukocytes.[42]
- These effects results in reduced need for surgical debridement and improved morbidity and mortality in patients with necrotizing fasciitis.
Contraindications to hyperbaric oxygen are:[43][44]
- Pneumothorax
- Cisplatin ((which decreases the production of superoxide dismutase which is protective against damaging effects of high partial O2 pressure)
- Doxorubicin therapy
Side effects of hyperbaric oxygen are:
- Barotrauma of the middle ear
- Seizures
- Loss of respiratory drive in hypercapnic patients (therefore, frequent periods of breathing in room air are interposed when patients are on HBOT)
- Vasoconstriction
IV γ-globulin
- Use of intravenous immune globulin is not FDA approved.
- If used, this treatment is restricted to critically ill patients with either staphylococcal or streptococcal infections.[45]
Surgery
Radical surgical debridement
Surgery is the mainstay of treatment for Fournier gangrene.[39]
- Indications include:[39]
- Patients displaying intense pain and skin color change such as edema and/or ecchymoses
- Signs of skin ischemia with blisters and bullae
- Altered mental status, hypotension, elevated band forms in the differential WBC count and metabolic acidosis.
- Immediate surgical referral remains the only method of reducing mortality and morbidity in Fournier gangrene patients.[46][47]
- As the patient's are cardiovascularly unstable, immediate resuscitation with intravenous fluids, colloids and inotropic agents are usually necessary.[48]
- Effects of analgesia can be measured by documenting pain score regularly.
- Stop the NSAID's on admission of patients.
Procedure
- Radical debridement of areas of overt subcutaneous necrosis should be done in operation theater in the lithotomy position (allows access to all perineal structures).
- Deep fascia and muscle are rarely involved. Hence debridement is usually not required.
- Separation of the skin and subcutaneous tissue with a hemostat has been recommended to define the limits of excision. Debridement is stopped where these tissues do not separate easily.
Fecal and urinary diversion
- Urinary or fecal diversion are required to treat an underlying condition or prevent wound contamination.[14]
- When there is gross urinary extravasation or periurethral inflammation, suprapubic cystostomy is required (urinary catheter is used in milder cases).
- Colostomy is required when there is gross sphincter infection or colonic or rectal perforation.
- Testes are temporarily implanted into subcutaneous tissue pouch (medial thigh or lower abdomen) until healing or reconstruction is complete.
- Orchidectomy is performed if there is any pre-existing epididymo-orchitis or scrotal abscess.
Plastic reconstruction
- The split thickness skin graft is commonly used technique for reconstructive surgery. For large defects, rotational or free myocutaneous flaps and omental flaps are used to cover larger defects.[14]
Wound management
- The wound is monitored closely after surgery.
- Multiple surgical debridement are required with an average of 3.5 procedures per patient.[10]
- Sodium hypochlorite or hydrogen peroxide are used post-operatively for topical application.[49]
- Lyophilized collagenase (an enzyme that digests and debrides necrotic tissues) is used for enzymatic debridement twice daily until definite reconstruction can be performed.[50]
Vacuum-assisted closure device
- Vacuum assisted closure device is used for faster and effective wound closure.[51][39]
- Helps wound healing by absorbing excess exudates, reducing localized edema, and finally drawing wound edges together.
Prevention
Primary prevention
Effective measures for the primary prevention of Fournier gangrene include:
- Prevention of trauma/breaks in skin integrity that act as portal of entry
- Treatment of cellulitis to prevent extension into the subcutaneous tissue
- Wounds should be cleaned and monitored for signs of infection
- Do not delay first aid of wounds like blisters, scrapes, or any break in the skin
- Patients with underlying co-morbidities should watch carefully for any signs of infection
Secondary prevention
Secondary prevention strategies following Fournier gangrene include:
- Early diagnosis and prompt treatment with either antibiotics or surgery.
- This strategy prevents or slows the progression and complications of the disease.
External links
References
- ↑ 1.0 1.1 Smith GL, Bunker CB, Dinneen MD (1998). "Fournier's gangrene". Br J Urol. 81 (3): 347–55. PMID 9523650.
- ↑ 2.0 2.1 Nathan B (1998). "Fournier's gangrene: a historical vignette". Can J Surg. 41 (1): 72. PMC 3950066. PMID 9492752.
- ↑ 3.0 3.1 3.2 Chennamsetty A, Khourdaji I, Burks F, Killinger KA (2015). "Contemporary diagnosis and management of Fournier's gangrene". Ther Adv Urol. 7 (4): 203–15. doi:10.1177/1756287215584740. PMC 4580094. PMID 26445600.
- ↑ Classification http://apps.who.int/classifications/icd10/browse/2016/en#/N49.8 (2016) Accessed on October 14, 2016
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Mallikarjuna MN, Vijayakumar A, Patil VS, Shivswamy BS (2012). "Fournier's Gangrene: Current Practices". ISRN Surg. 2012: 942437. doi:10.5402/2012/942437. PMC 3518952. PMID 23251819.
- ↑ Morua AG, Lopez JA, Garcia JD, Montelongo RM, Guerra LS (2009). "Fournier's gangrene: our experience in 5 years, bibliographic review and assessment of the Fournier's gangrene severity index". Arch Esp Urol. 62 (7): 532–40. PMID 19815967.
- ↑ 7.0 7.1 7.2 7.3 Shyam DC, Rapsang AG (2013). "Fournier's gangrene". Surgeon. 11 (4): 222–32. doi:10.1016/j.surge.2013.02.001. PMID 23578806.
- ↑ Katib A, Al-Adawi M, Dakkak B, Bakhsh A (2013). "A three-year review of the management of Fournier's gangrene presented in a single Saudi Arabian institute". Cent European J Urol. 66 (3): 331–4. doi:10.5173/ceju.2013.03.art22. PMC 3974467. PMID 24707378.
- ↑ Gupta A, Dalela D, Sankhwar SN, Goel MM, Kumar S, Goel A; et al. (2007). "Bilateral testicular gangrene: does it occur in Fournier's gangrene?". Int Urol Nephrol. 39 (3): 913–5. doi:10.1007/s11255-006-9126-1. PMID 17323114.
- ↑ 10.0 10.1 Chawla SN, Gallop C, Mydlo JH (2003). "Fournier's gangrene: an analysis of repeated surgical debridement". Eur Urol. 43 (5): 572–5. PMID 12706005.
- ↑ Campos JA, Martos JA, Gutiérrez del Pozo R, Carretero P (1990). "Synchronous caverno-spongious thrombosis and Fournier's gangrene". Arch Esp Urol. 43 (4): 423–6. PMID 2383054.
- ↑ 12.0 12.1 Eke N (2000). "Fournier's gangrene: a review of 1726 cases". Br J Surg. 87 (6): 718–28. doi:10.1046/j.1365-2168.2000.01497.x. PMID 10848848.
- ↑ Thwaini A, Khan A, Malik A, Cherian J, Barua J, Shergill I, Mammen K (2006). "Fournier's gangrene and its emergency management". Postgrad Med J. 82 (970): 516–9. PMID 16891442.
- ↑ 14.0 14.1 14.2 14.3 Paty R, Smith AD (1992). "Gangrene and Fournier's gangrene". Urol Clin North Am. 19 (1): 149–62. PMID 1736475.
- ↑ Yanar H, Taviloglu K, Ertekin C, Guloglu R, Zorba U, Cabioglu N; et al. (2006). "Fournier's gangrene: risk factors and strategies for management". World J Surg. 30 (9): 1750–4. doi:10.1007/s00268-005-0777-3. PMID 16927060.
- ↑ Jensen P, Zachariae C, Grønhøj Larsen F (2010). "Necrotizing soft tissue infection of the glans penis due to atypical Candida species complicated with Fournier's gangrene". Acta Derm Venereol. 90 (4): 431–2. doi:10.2340/00015555-0847. PMID 20574621.
- ↑ Tleyjeh IM, Routh J, Qutub MO, Lischer G, Liang KV, Baddour LM (2004). "Lactobacillus gasseri causing Fournier's gangrene". Scand J Infect Dis. 36 (6–7): 501–3. PMID 15307582.
- ↑ 18.0 18.1 18.2 Vick R, Carson CC (1999). "Fournier's disease". Urol Clin North Am. 26 (4): 841–9. PMID 10584624.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 19.7 Fournier's gangrene https://radiopaedia.org/articles/fournier-gangrene (2016) Accessed on October 12, 2016
- ↑ 20.0 20.1 Sorensen MD, Krieger JN (2016). "Fournier's Gangrene: Epidemiology and Outcomes in the General US Population". Urol Int. 97 (3): 249–259. doi:10.1159/000445695. PMID 27172977.
- ↑ Moslemi MK, Sadighi Gilani MA, Moslemi AA, Arabshahi A (2009). "Fournier gangrene presenting in a patient with undiagnosed rectal adenocarcinoma: a case report". Cases J. 2: 9136. doi:10.1186/1757-1626-2-9136. PMC 2803933. PMID 20062653.
- ↑ 22.0 22.1 Clayton MD, Fowler JE, Sharifi R, Pearl RK (1990). "Causes, presentation and survival of fifty-seven patients with necrotizing fasciitis of the male genitalia". Surg Gynecol Obstet. 170 (1): 49–55. PMID 2294630.
- ↑ 23.0 23.1 Morpurgo E, Galandiuk S (2002). "Fournier's gangrene". Surg Clin North Am. 82 (6): 1213–24. PMID 12516849.
- ↑ 24.0 24.1 Amendola MA, Casillas J, Joseph R, Antun R, Galindez O (1994). "Fournier's gangrene: CT findings". Abdom Imaging. 19 (5): 471–4. PMID 7950832.
- ↑ Morgan MS (2010). "Diagnosis and management of necrotising fasciitis: a multiparametric approach". J Hosp Infect. 75 (4): 249–57. doi:10.1016/j.jhin.2010.01.028. PMID 20542593.
- ↑ Ecker KW, Derouet H, Omlor G, Mast GJ (1993). "[Fournier's gangrene]". Chirurg. 64 (1): 58–62. PMID 8436051.
- ↑ Akcan A, Sözüer E, Akyildiz H, Yilmaz N, Küçük C, Ok E (2009). "Necessity of preventive colostomy for Fournier's gangrene of the anorectal region". Ulus Travma Acil Cerrahi Derg. 15 (4): 342–6. PMID 19669962.
- ↑ Thwaini A, Khan A, Malik A, Cherian J, Barua J, Shergill I; et al. (2006). "Fournier's gangrene and its emergency management". Postgrad Med J. 82 (970): 516–9. doi:10.1136/pgmj.2005.042069. PMC 2585703. PMID 16891442.
- ↑ Kuo CF, Wang WS, Lee CM, Liu CP, Tseng HK (2007). "Fournier's gangrene: ten-year experience in a medical center in northern Taiwan". J Microbiol Immunol Infect. 40 (6): 500–6. PMID 18087630.
- ↑ Kabay S, Yucel M, Yaylak F, Algin MC, Hacioglu A, Kabay B; et al. (2008). "The clinical features of Fournier's gangrene and the predictivity of the Fournier's Gangrene Severity Index on the outcomes". Int Urol Nephrol. 40 (4): 997–1004. doi:10.1007/s11255-008-9401-4. PMID 18563618.
- ↑ Wong CH, Khin LW, Heng KS, Tan KC, Low CO (2004). "The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections". Crit Care Med. 32 (7): 1535–41. PMID 15241098.
- ↑ Yeniyol CO, Suelozgen T, Arslan M, Ayder AR (2004). "Fournier's gangrene: experience with 25 patients and use of Fournier's gangrene severity index score". Urology. 64 (2): 218–22. doi:10.1016/j.urology.2004.03.049. PMID 15302463.
- ↑ 33.0 33.1 Talwar A, Puri N, Singh M (2010). "Fournier's Gangrene of the Penis: A Rare Entity". J Cutan Aesthet Surg. 3 (1): 41–4. doi:10.4103/0974-2077.63394. PMC 2890137. PMID 20606995.
- ↑ 34.0 34.1 34.2 34.3 34.4 Fourniers gangrene http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=157 Accessed on October 14,2016
- ↑ Rajan DK, Scharer KA (1998). "Radiology of Fournier's gangrene". AJR Am J Roentgenol. 170 (1): 163–8. doi:10.2214/ajr.170.1.9423625. PMID 9423625.
- ↑ Kickuth R, Adams S, Kirchner J, Pastor J, Simon S, Liermann D (2001). "Magnetic resonance imaging in the diagnosis of Fournier's gangrene". Eur Radiol. 11 (5): 787–90. doi:10.1007/s003300000599. PMID 11372608.
- ↑
- ↑ Gilbert, David (2015). The Sanford guide to antimicrobial therapy. Sperryville, Va: Antimicrobial Therapy. ISBN 978-1930808843.
- ↑ 39.0 39.1 39.2 39.3 Misiakos EP, Bagias G, Patapis P, Sotiropoulos D, Kanavidis P, Machairas A (2014). "Current concepts in the management of necrotizing fasciitis". Front Surg. 1: 36. doi:10.3389/fsurg.2014.00036. PMC 4286984. PMID 25593960.
- ↑ Escobar SJ, Slade JB, Hunt TK, Cianci P (2005). "Adjuvant hyperbaric oxygen therapy (HBO2)for treatment of necrotizing fasciitis reduces mortality and amputation rate". Undersea Hyperb Med. 32 (6): 437–43. PMID 16509286.
- ↑ Korhonen K (2000). "Hyperbaric oxygen therapy in acute necrotizing infections with a special reference to the effects on tissue gas tensions". Ann Chir Gynaecol Suppl (214): 7–36. PMID 11199291.
- ↑ Hyperbaric oxygen therapy. http://onlinelibrary.wiley.com/doi/10.1080/110241500750008583/abstract (2016) Accessed on September 12, 2016
- ↑ Kindwall EP, Gottlieb LJ, Larson DL (1991). "Hyperbaric oxygen therapy in plastic surgery: a review article". Plast Reconstr Surg. 88 (5): 898–908. PMID 1924583.
- ↑ Capelli-Schellpfeffer M, Gerber GS (1999). "The use of hyperbaric oxygen in urology". J Urol. 162 (3 Pt 1): 647–54. PMID 10458334.
- ↑ Darabi K, Abdel-Wahab O, Dzik WH (2006). "Current usage of intravenous immune globulin and the rationale behind it: the Massachusetts General Hospital data and a review of the literature". Transfusion. 46 (5): 741–53. doi:10.1111/j.1537-2995.2006.00792.x. PMID 16686841.
- ↑ Roje Z, Roje Z, Matić D, Librenjak D, Dokuzović S, Varvodić J (2011). "Necrotizing fasciitis: literature review of contemporary strategies for diagnosing and management with three case reports: torso, abdominal wall, upper and lower limbs". World J Emerg Surg. 6 (1): 46. doi:10.1186/1749-7922-6-46. PMC 3310784. PMID 22196774.
- ↑ Mok MY, Wong SY, Chan TM, Tang WM, Wong WS, Lau CS (2006). "Necrotizing fasciitis in rheumatic diseases". Lupus. 15 (6): 380–3. PMID 16830885.
- ↑ Baxter F, McChesney J (2000). "Severe group A streptococcal infection and streptococcal toxic shock syndrome". Can J Anaesth. 47 (11): 1129–40. doi:10.1007/BF03027968. PMID 11097546.
- ↑ Hejase MJ, Simonin JE, Bihrle R, Coogan CL (1996). "Genital Fournier's gangrene: experience with 38 patients". Urology. 47 (5): 734–9. PMID 8650874.
- ↑ Aşci R, Sarikaya S, Büyükalpelli R, Yilmaz AF, Yildiz S (1998). "Fournier's gangrene: risk assessment and enzymatic debridement with lyophilized collagenase application". Eur Urol. 34 (5): 411–8. PMID 9803004.
- ↑ Silberstein J, Grabowski J, Parsons JK (2008). "Use of a Vacuum-Assisted Device for Fournier's Gangrene: A New Paradigm". Rev Urol. 10 (1): 76–80. PMC 2312348. PMID 18470279.
![Distribution of annual cases per hospital.[20]](/images/4/45/Epidemiology.jpg)
![Brownish-black discolouration of the penis with erythema of the scrotum.[33]](/images/8/87/Fourniers_gangrene_1.jpg)
![Discolouration of the penis with vesicles filled with hemorrhagic fluid.[33]](/images/7/7e/Fourniers_gangrene_2.jpg)
![Fournier gangrene. [34]](/images/5/58/Fournier%27s_gangrene_01.jpeg)
![Fournier gangrene. [34]](/images/2/22/Fournier%27s_gangrene_02.jpeg)
![Fournier gangrene. [34]](/images/2/2c/Fournier%27s_gangrene_03.jpeg)
![Fournier gangrene. [34]](/images/1/1b/Fournier%27s_gangrene_04.jpeg)
![Fournier gangrene. [34]](/images/0/04/Fournier%27s_gangrene_05.jpeg)
![X ray of Fournier gangrene [19]](/images/2/2d/Founier-gangrene_X-ray.JPG)
![Ultrasound of Fournier gangrene [19]](/images/3/32/Fournier-gangrene-usg.jpg)
![CT of Fournier gangrene [19]](/images/2/2d/Fournier-gangrene_CT.jpg)
![CT of Fournier gangrene with spontaneous perforation of rectal cancer [19]](/images/4/40/Fournier-gangrene-spontaneous-perforation-of-rectal-cancer.jpg)