Fentanyl (sublingual)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Chetan Lokhande, M.B.B.S [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Warning: risk of respiratory depression, medication errors, abuse potential
See full prescribing information for complete Boxed Warning.
|
Overview
Fentanyl (sublingual) is an analgesic opioid that is FDA approved for the treatment of breakthrough cancer pain, in opioid-tolerant patients, pain, chronic (severe), in opioid-tolerant patients requiring a long-term daily around-the-clock opioid analgesic.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include dermatologic: application site reaction (adults, 1% or greater ; pediatrics, 3% to 10% ), diaphoresis (adults: transdermal 10% or greater , sublingual 1% or greater ; pediatrics: transdermal 1% or greater ), pruritus (transdermal, 3% to 10% ; sublingual, 1% or greater gastrointestinal: abdominal pain (transdermal, 3% to 10% ; sublingual, 1% or greater ), constipation (adults, 10% or greater ; pediatrics, 3% to 10% ), diarrhea (adults: transdermal 3% to 10% , sublingual 1% or greater ; pediatrics: transdermal 1% or greater ), indigestion (transdermal, 3% to 10% ; sublingual, 1% or greater ), loss of appetite (transdermal, 3% to 10% ; sublingual, 1% or greater ), nausea (10% or greater ), vomiting (10% or greater ), xerostomia (adults: transdermal 10% or greater , sublingual 1% or greater ; pediatrics: transdermal 1% or greater ), neurologic: asthenia (adults, 9.7% or greater ; pediatrics, 3% to 10% ), confusion (adults: transdermal 10% or greater , sublingual 1% or greater ; pediatrics: transdermal 1% or greater ), dizziness (adults, 3% to 10% ; pediatrics, 1% or greater ), feeling nervous (3% to 10% ), headache (transdermal, 3% to 10% ; sublingual, 1% or greater ), insomnia (adults, 1% or greater ; pediatrics, 3% to 10% ), somnolence (adult, 1% to 19% ; pediatrics, 16% ), psychiatric: Anxiety (adults, 3% to 10% ; pediatrics, 1% or greater ), depression (adults: transdermal 3% to 10% , sublingual 1% or greater ; pediatrics: transdermal 1% or greater ), euphoria (3% to 10% ), hallucinations (adults: transdermal 3% to 10%, sublingual 1% or greater ; pediatrics: transdermal 1% or greater ), renal: urinary retention (adults: transdermal 3% to 10% , sublingual less than 1% ; pediatrics: transdermal 1% or greater ), respiratory: dyspnea (adults: transdermal 3% to 10%, sublingual 10.4% ; pediatrics: transdermal 1% or greater ), upper respiratory infection (3% to 10% ), other: Fatigue (transdermal, 3% to 10% ; sublingual, 1% or greater ), influenza-like symptoms (3% to 10% ).
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- For use in opioid-tolerant patients only, ie; those patients tolerant to at least 60 mg of morphine/day, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, or an equianalgesic dose of another opioid for a week or longer.
- SL spray (Subsys(R)): do not substitute for any other fentanyl products on a mcg per mcg basis, as the SL spray is not bioequivalent to other fentanyl products and this may result in fatal overdose.
- Transdermal system (Duragesic(R)): individualize initial dose selection based on previous opiate requirements, degree of tolerance, and patient status; close attention should be paid to dose conversion guidelines to prevent overestimation of fentanyl dose and fatal overdose, do not discontinue abruptly.
- Breakthrough cancer pain, in opioid-tolerant patients: SL spray (Subsys(TM)) initial, all patients 100 mcg under the tongue; may repeat once after 30 minutes; do not use more than 2 doses per episode of breakthrough pain; repeated treatment of subsequent episode should be separated by at least 4 hours; if adequate pain relief is achieved, use this dose for subsequent episodes of breakthrough pain.
- Breakthrough cancer pain, in opioid-tolerant patients: SL spray (Subsys(TM)) dose titration, increase dose to the next highest strength (eg, 200 mcg, 400 mcg, 600 mcg, 800 mcg, 1200 mcg, then 1600 mcg); may repeat the same dose after 30 minutes; do not use more than 2 doses per episode of breakthrough pain; repeated treatment of subsequent episode should be separated by at least 4 hours; if adequate pain relief is achieved, use this dose for subsequent episodes of breakthrough pain.
- Breakthrough cancer pain, in opioid-tolerant patients: SL spray (Subsys(TM)) maintenance dose, once a successful dose has been found, use only 1 dose of the appropriate strength per breakthrough pain episode; limit use to 4 episodes of breakthrough pain per day.
- Breakthrough cancer pain, in opioid-tolerant patients: (conversion from Actiq(R) to Subsys(R)) current Actiq(R) dose 200 to 400 mcg, initiate Subsys(R) 100 mcg and titrate by multiples of 100 mcg; current Actiq(R) dose 600 to 800 mcg, initiate Subsys(R) 200 mcg and titrate by multiples of 200 mcg; current Actiq(R) dose 1200 to 1600 mcg, initiate Subsys(R) 400 mcg and titrate by multiples of 400 mcg [5]
- Pain, chronic (severe), in opioid-tolerant patients requiring a long-term daily around-the-clock opioid analgesic: individualize dose; initial dose selection must take into account prior analgesic treatment experience and risk factors for addiction, abuse, and misuse; discontinue all other around-the-clock opioids prior to fentanyl initiation; due to substantial inter-patient variability in relative potency of different opioid products, when converting it is recommended to underestimate a patient's 24-hour fentanyl requirements and provide rescue mediation as needed.
- Pain, chronic (severe), in opioid-tolerant patients requiring a long-term daily around-the-clock opioid analgesic: initial dose recommendations based on daily oral morphine requirement: initiate at 25 mcg/hr for oral morphine doses of 60 to 134 mg/day; initiate at 50 mcg/hr for oral morphine doses of 135 to 224 mg/day; initiate at 75 mcg/hr for oral morphine doses of 225 to 314 mg/day; initiate at 100 mcg/hr for oral morphine doses of 315 to 404 mg/day; initiate at 125 mcg/hr for oral morphine doses of 405 to 494 mg/day; initiate at 150 mcg/hr for oral morphine doses of 495 to 584 mg/day; initiate at 175 mcg/hr for oral morphine doses of 585 to 674 mg/day; initiate at 200 mcg/hr for oral morphine doses of 675 to 764 mg/day; initiate at 225 mcg/hr for oral morphine doses of 765 to 854 mg/day; initiate at 250 mcg/hr for oral morphine doses of 855 to 944 mg/day; initiate at 275 mcg/hr for oral morphine doses of 945 to 1034 mg/day; initiate at 300 mcg/hr for oral morphine doses of 1035 to 1124 mg/day; apply transdermally; replace patch every 72 hours; for delivery rates exceeding 100 mcg/hr multiple patches may be used.
- Pain, chronic (severe), in opioid-tolerant patients requiring a long-term daily around-the-clock opioid analgesic: dose titration: do not increase dose in first 3 days; first dose titration should be based on the daily dose of supplemental opioid analgesics required on day 2 or 3; subsequent titrations should occur no more often than every 6 days and dose increases should be based on daily supplemental opioid dose using the ratio 45 mg/24 hours of oral morphine to a 12 mcg/hr increase in transdermal fentanyl ; a small number of patients may require patch application every 48 hours; a dose increase should be evaluated before considering a change in dosing interval
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Fentanyl in adult patients.
Non–Guideline-Supported Use
- Osteoarthritis (Moderate to Severe), inadequate response with weak opioid analgesic therapy
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- SL spray (Subsys(R)): safety and efficacy have not been established in pediatric patients younger than 18 years.
- Transdermal system (Duragesic(R)): safety of transdermal fentanyl has not been established in children younger than 2 years for use in opioid-tolerant patients only (ie, those patients tolerant to at least 60 mg of morphine/day, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, or an equianalgesic dose of another opioid for a week or longer).
- Transdermal system (Duragesic(R)): individualize initial dose selection based on previous opiate requirements, degree of tolerance, and patient status; close attention should be paid to dose conversion guidelines to prevent overestimation of fentanyl dose and fatal overdose; do not discontinue abruptly.
- Pain, chronic (severe), in opioid-tolerant patients requiring a long-term daily around-the-clock opioid analgesic: individualize dose; initial dose selection must take into account prior analgesic treatment experience and risk factors for addiction, abuse, and misuse; discontinue all other around-the-clock opioids prior to fentanyl initiation; due to substantial inter-patient variability in relative potency of different opioid products, when converting it is recommended to underestimate a patient's 24-hour fentanyl requirements and provide rescue mediation as needed.
- Pain, chronic (severe), in opioid-tolerant patients requiring a long-term daily around-the-clock opioid analgesic: (2 years or older) initial dose recommendations based on daily oral morphine requirement:
- Initiate at 25 mcg/hr for oral morphine doses of 60 to 134 mg/day;
- Initiate at 50 mcg/hr for oral morphine doses of 135 to 224 mg/day;
- Initiate at 75 mcg/hr for oral morphine doses of 225 to 314 mg/day;
- Initiate at 100 mcg/hr for oral morphine doses of 315 to 404 mg/day;
- Initiate at 125 mcg/hr for oral morphine doses of 405 to 494 mg/day;
- Initiate at 150 mcg/hr for oral morphine doses of 495 to 584 mg/day;
- Initiate at 175 mcg/hr for oral morphine doses of 585 to 674 mg/day;
- Initiate at 200 mcg/hr for oral morphine doses of 675 to 764 mg/day;
- Initiate at 225 mcg/hr for oral morphine doses of 765 to 854 mg/day;
- Initiate at 250 mcg/hr for oral morphine doses of 855 to 944 mg/day;
- Initiate at 275 mcg/hr for oral morphine doses of 945 to 1034 mg/day;
- Initiate at 300 mcg/hr for oral morphine doses of 1035 to 1124 mg/day;
- Apply transdermally; replace patch every 72 hours; for delivery rates exceeding 100 mcg/hr multiple patches may be used.
- Pain, chronic (Severe), in opioid-tolerant patients requiring a long-term daily around-the-clock opioid analgesic: dose titration: do not increase dose in first 3 days; first dose titration should be based on the daily dose of supplemental opioid analgesics required on day 2 or 3; subsequent titrations should occur no more often than every 6 days and dose increases should be based on daily supplemental opioid dose using the ratio 45 mg/24 hours of oral morphine to a 12 mcg/hr increase in transdermal fentanyl.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Fentanyl in pediatric patients.
Non–Guideline-Supported Use
There is limited information about Off-Label Non–Guideline-Supported Use of Fentanyl in pediatric patients.
Contraindications
- Fentanyl is contraindicated in the management of pain in opioid non-tolerant patients, because life-threatening hypoventilation could occur at any dose in patients not already taking around-the-clock opioid therapy. Patients considered opioid tolerant are those who are taking at least 60 mg oral morphine/day, or at least 25 mcg transdermal fentanyl/hour, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mg oral oxymorphone/day, or an equianalgesic dose of another opioid for a week or longer.
- Fentanyl is contraindicated in the management of acute or postoperative pain, including headache/migraine, dental pain, or use in the emergency room.
- Fentanyl is contraindicated in patients with known intolerance or hypersensitivity to any of its components or the drug fentanyl. Anaphylaxis and hypersensitivity have been reported in association with the use of other oral transmucosal fentanyl products.
Warnings
|
Warning: risk of respiratory depression, medication errors, abuse potential
See full prescribing information for complete Boxed Warning.
|
Hypoventilation (Respiratory Depression)
- Serious or fatal respiratory depression can occur even at recommended doses in patients using Fentanyl. Respiratory depression is more likely to occur in patients with underlying respiratory disorders and elderly or debilitated patients, usually following large initial doses, including Fentanyl, in opioid non-tolerant patients, or when opioids are given in conjunction with other drugs that depress respiration.
- Respiratory depression from opioids is manifested by a reduced urge to breathe and a decreased rate of respiration, often associated with the "sighing" pattern of breathing (deep breaths separated by abnormally long pauses). Carbon dioxide retention from opioid- induced respiratory depression can exacerbate the sedating effects of opioids. This makes overdoses involving drugs with sedative properties and opioids especially dangerous.
Fentanyl and Other Fentanyl Products
- Fentanyl is not equivalent to all other fentanyl products used to treat breakthrough pain on a mcg per mcg basis. There are differences in the pharmacokinetics of Fentanyl relative to other fentanyl products which could potentially result in clinically important differences in the amount of fentanyl absorbed and could result in a fatal overdose.
- When prescribing Fentanyl to a patient, Do not convert from other fentanyl products. Directions for safely converting patients to Fentanyl from other fentanyl products are not currently available. (Note: This includes oral, transdermal, or parenteral formulations of fentanyl). Therefore, for opioid-tolerant patients starting treatment for breakthrough pain, the initial dose of Fentanyl is 100 mcg. Individually titrate each patient's dose to provide adequate analgesia while minimizing side effects. [See Dosage and Administration]
- When dispensing Fentanyl to a patient, Do not substitute it for any other fentanyl product prescription.
Patient/Caregiver Instructions
- Patients and their caregivers must be instructed that Fentanyl contains a medicine in an amount which can be fatal to a child. Even though Fentanyl is provided in child-resistant packaging, patients and their caregivers must be instructed to keep tablets out of the reach of children. [see How Supplied/Storage and Handling, and Patient Counseling Information].
- Taking Fentanyl could be fatal in individuals for whom it is not prescribed and for those who are not opioid-tolerant.
- Physicians and dispensing pharmacists must specifically question patients or caregivers about the presence of children in the home (on a full time or visiting basis) and counsel them regarding the dangers to children from inadvertent exposure.
Additive CNS Depressant Effects
- The concomitant use of Fentanyl with other CNS depressants, including other opioids, sedatives or hypnotics, general anesthetics, phenothiazines, tranquilizers, skeletal muscle relaxants, sedating antihistamines, and alcoholic beverages may produce increased depressant effects (e.g., hypoventilation, hypotension, and profound sedation). Concomitant use with potent inhibitors of cytochrome P450 3A4 isoform (e.g., erythromycin, ketoconazole, and certain protease inhibitors) may increase fentanyl levels, resulting in increased depressant effects [see Drug Interactions].
- Patients on concomitant CNS depressants must be monitored for a change in opioid effects and the dose of Fentanyl adjusted, if warranted.
Effects on Ability to Drive and Use Machines
- Opioid analgesics impair the mental and/or physical ability required for the performance of potentially dangerous tasks (e.g., driving a car or operating machinery). Warn patients taking fentanyl of these dangers and counsel them accordingly.
Chronic Pulmonary Disease
- Because potent opioids can cause hypoventilation, titrate fentanyl with caution in patients with chronic obstructive pulmonary disease or pre-existing medical conditions predisposing them to hypoventilation. In such patients, even normal therapeutic doses of Fentanyl may further decrease respiratory drive to the point of respiratory failure.
Head Injuries and Increased Intracranial Pressure
- Administer fentanyl with extreme caution in patients who may be particularly susceptible to the intracranial effects of CO2 retention such as those with evidence of increased intracranial pressure or impaired consciousness. Opioids may obscure the clinical course of a patient with a head injury; use only if clinically warranted.
Cardiac Disease
- Intravenous administration of fentanyl may produce bradycardia. Therefore, use fentanyl with caution in patients with bradyarrhythmias.
MAO Inhibitors
- Fentanyl is not recommended for use in patients who have received MAO inhibitors within the past 14 days. Severe and unpredictable potentiation by MAO inhibitors has been reported with opioid analgesics.
- Transmucosal immediate Release Fentanyl (TIRF) Risk Evaluation and Mitigation Strategy (REMS) Access Program
- Because of the risk for misuse, abuse, addiction, and overdose [see Drug Abuse and Dependence], Fentanyl is available only through a restricted program called the TIRF REMS Access program. Under the TIRF REMS Access program, outpatients, healthcare professionals who prescribe to outpatients, pharmacies, and distributors must enroll in the program. For inpatient administration (e.g., hospitals, hospices, and long-term care facilities that prescribe for inpatient use) of Fentanyl, patient and prescriber enrollment is not required.
- Required components of the TIRF REMS Access program are:
- Healthcare professionals who prescribe Fentanyl must review the prescriber educational materials for the TIRF REMS Access program, enroll in the program, and comply with the REMS requirements.
- To receive Fentanyl, outpatients must understand the risks and benefits and sign a Patient-Prescriber Agreement.
- Pharmacies that dispense Fentanyl must enroll in the program and agree to comply with the REMS requirements.
- Wholesalers and distributors that distribute Fentanyl must enroll in the program and distribute only to authorized pharmacies.
- Further information, including a list of qualified pharmacies/distributors, is available at www.TIRFREMSAccess.com or by calling 1-866-822-1483.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse event rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The safety of Fentanyl has been evaluated in 311 opioid-tolerant cancer patients with breakthrough pain. Two hundred and seventy (270) of these patients were treated in multiple-dose studies. The duration of therapy for patients in multiple-dose studies ranged from 1-405 days with an average duration of 131 days and with 44 patients treated for at least 12 months.
- The most commonly observed adverse reactions with Fentanyl include typical opioid adverse reactions, such as nausea, constipation, somnolence and headache. Expect opioid side effects and manage them accordingly.
- The clinical trials of Fentanyl were designed to evaluate safety and efficacy in treating patients with cancer and breakthrough pain; all patients were taking concomitant opioids, such as sustained-release morphine, sustained-release oxycodone or transdermal fentanyl, for their persistent pain.
- The adverse reaction data presented in Table 1 reflect the actual percentage of patients experiencing reactions among patients who received Fentanyl for breakthrough pain along with concomitant opioid use for persistent pain. There has been no attempt to correct for concomitant use of other opioids, duration of Fentanyl therapy or cancer-related symptoms.Table 1 lists adverse reactions with an overall frequency of 5% or greater within the total population that occurred during titration by maximum dose received. The ability to assign Fentanyl a dose-response relationship to these adverse reactions is limited by the titration schemes used in these studies.

- The frequencies listed below represent adverse reactions that occurred in ≥ 1% of patients from two clinical trials who experienced that reaction while receiving Fentanyl. Reactions are classified by system organ class.
Adverse Reactions (≥ 1%)
- Cardiac disorders: bradycardia, tachycardia.
- Eye disorders: vision blurred.
- Gastrointestinal disorders: abdominal pain, abdominal pain upper, aphthous stomatitis, constipation, dry mouth, dyspepsia, gingival ulceration, impaired gastric emptying, lip ulceration, mouth ulceration, nausea, stomach discomfort, stomatitis, tongue disorder, vomiting.
- General disorders and administration site conditions: asthenia, drug withdrawal syndrome, fatigue, malaise.
- Immune system disorders: drug hypersensitivity.
- Injury, poisoning and procedural complications: accidental overdose.
- Metabolism and nutrition disorders: anorexia, decreased appetite.
- Nervous system disorders: amnesia, disturbance in attention, dizziness, dysgeusia, headache, hypoesthesia, lethargy, parosmia, somnolence, tremor.
- Psychiatric disorders: affect lability, anxiety, confusional state, depression, disorientation, dysphoria, euphoric mood, insomnia, mental status changes, paranoia, sleep disorder.
- Reproductive system and breast disorders: erectile dysfunction.
- Respiratory, thoracic and mediastinal disorder: dyspnea, oropharyngeal pain, throat tightness.
- Skin and subcutaneous disorders: hyperhidrosis, night sweats, pruritus, rash, skin lesion.
- Vascular disorders: hypotension.
Postmarketing Experience
There is limited information regarding Fentanyl (sublingual) Postmarketing Experience in the drug label.
Drug Interactions
- Fentanyl is metabolized mainly via the human cytochrome P450 3A4 isoenzyme system (CYP3A4); therefore potential interactions may occur when Fentanyl is given concurrently with agents that affect CYP3A4 activity.
- The concomitant use of Fentanyl with CYP3A4 inhibitors (e.g., indinavir, nelfinavir, ritonavir, clarithromycin, itraconazole, ketoconazole, nefazodone, saquinavir, telithromycin, aprepitant, diltiazem, erythromycin, fluconazole, grapefruit juice, verapamil, or cimetidine) may result in a potentially dangerous increase in fentanyl plasma concentrations, which could increase or prolong adverse drug effects and may cause potentially fatal respiratory depression. Patients receiving Fentanyl who begin therapy with, or increase the dose of, CYP3A4 inhibitors need to be carefully monitored for signs of opioid toxicity over an extended period of time. Increase dosage conservatively.
- The concomitant use of Fentanyl with CYP3A4 inducers (e.g., barbiturates, carbamazepine, efavirenz, glucocorticoids, modafinil, nevirapine, oxcarbazepine, phenobarbital, phenytoin, pioglitazone, rifabutin, rifampin, St. John's wort, or troglitazone) may result in a decrease in fentanyl plasma concentrations, which could decrease the efficacy of Fentanyl.
- Patients receiving Fentanyl who stop therapy with, or decrease the dose of, CYP3A4 inducers need to be monitored for signs of increased Fentanyl activity and the dose of Fentanyl must be adjusted accordingly.
Use in Specific Populations
Pregnancy
- There are no adequate and well-controlled studies in pregnant women.
- Use Fentanyl during pregnancy only if the potential benefit justifies the potential risk to the fetus. No epidemiological studies of congenital anomalies in infants born to women treated with fentanyl during pregnancy have been reported.
- Chronic maternal treatment with fentanyl during pregnancy has been associated with transient respiratory depression, behavioral changes, or seizures in newborn infants characteristic of neonatal abstinence syndrome.
- In women treated acutely with intravenous or epidural fentanyl during labor, symptoms of neonatal respiratory or neurological depression were no more frequent than would be expected in infants of untreated mothers.
- Transient neonatal muscular rigidity has been observed in infants whose mothers were treated with intravenous fentanyl.
- Fentanyl is embryocidal in rats as evidenced by increased resorptions in pregnant rats at doses of 30 mcg/kg intravenously or 160 mcg/kg subcutaneously. Conversion to human equivalent doses indicates this is within the range of the human recommended dosing for Fentanyl.
- Fentanyl citrate was not teratogenic when administered to pregnant animals. Published studies demonstrated that administration of fentanyl (10, 100, or 500 mcg/kg/day) to pregnant rats from day 7 to 21, of their 21 day gestation, via implanted microosmotic minipumps, was not teratogenic (the high dose was approximately 6-times the human dose of 800 mcg per pain episode on a mcg/m2 basis). Intravenous administration of fentanyl (10 mcg/kg or 30 mcg/kg) to pregnant female rats from gestation day 6 to 18, was embryo- or feto-toxic, and caused a slightly increased mean delivery time in the 30 mcg/kg/day group, but was not teratogenic.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Fentanyl (sublingual) in women who are pregnant.
Labor and Delivery
- Fentanyl readily crosses the placenta. Therefore do not use Fentanyl during labor and delivery (including caesarean section) since it may cause respiratory depression in the fetus or in the newborn infant.
Nursing Mothers
- Fentanyl is excreted in human milk; therefore, do not use Fentanyl in women who are nursing because of the possibility of sedation and/or respiratory depression in their infants. Symptoms of opioid withdrawal may occur in infants at the cessation of nursing by women using Fentanyl.
Pediatric Use
The safety and efficacy of Fentanyl have not been established in patients below 18 years of age.
Geriatic Use
- Of the 270 opioid tolerant patients with breakthrough cancer pain in the Phase 3 clinical studies of Fentanyl, 58 (21%) were 65 years of age and older. There was no difference in the median titrated dose in patients aged 65 years and older compared to those <65 years. No clinically meaningful difference was noted in the safety profile of the group 65 years of age and older as compared to younger patients in Fentanyl clinical trials.
- Elderly patients have been shown to be more sensitive to the effects of fentanyl when administered intravenously, compared with the younger adult population. Therefore, exercise caution when individually titrating Fentanyl in elderly patients to provide adequate efficacy while minimizing risk.
Gender
- Both male and female opioid-tolerant cancer patients were studied for the treatment of breakthrough cancer pain. No clinically relevant gender differences were noted either in efficacy or in observed adverse reactions.
Race
There is no FDA guidance on the use of Fentanyl (sublingual) with respect to specific racial populations.
Renal Impairment
- Insufficient information exists to make recommendations regarding the use of Fentanyl in patients with impaired renal or hepatic function. Fentanyl is metabolized primarily via human cytochrome P450 3A4 isoenzyme system and the inactive metabolite is mostly eliminated in urine. If the drug is used in these patients, use the drug with caution because of the reduced hepatic metabolism and renal excretion capacity in such patients.
Hepatic Impairment
- Insufficient information exists to make recommendations regarding the use of Fentanyl in patients with impaired renal or hepatic function. Fentanyl is metabolized primarily via human cytochrome P450 3A4 isoenzyme system and the inactive metabolite is mostly eliminated in urine. If the drug is used in these patients, use the drug with caution because of the reduced hepatic metabolism and renal excretion capacity in such patients.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Fentanyl (sublingual) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Fentanyl (sublingual) in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Fentanyl (sublingual) Administration in the drug label.
Monitoring
There is limited information regarding Fentanyl (sublingual) Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Fentanyl (sublingual) and IV administrations.
Overdosage
Clinical Presentation
- The manifestations of Fentanyl overdosage are expected to be similar in nature to intravenous fentanyl and other opioids, and are an extension of its pharmacological actions with the most serious significant effect being hypoventilation [see Clinical Pharmacology (12.2)].
Immediate Management
- Immediate management of opioid overdose includes removal of the Fentanyl tablet, if still in the mouth, ensuring a patent airway, physical and verbal stimulation of the patient, and assessment of level of consciousness, ventilatory and circulatory status.
Treatment of Overdosage (Accidental Ingestion) in the Opioid NON-Tolerant Person
- Provide ventilatory support, obtain intravenous access, and administer naloxone or other opioid antagonists as clinically indicated. The duration of respiratory depression following overdose may be longer than the effects of the opioid antagonist's action (e.g., the half-life of naloxone ranges from 30 to 81 minutes) and repeated administration may be necessary. Consult the package insert of the individual opioid antagonist for details.
Treatment of Overdosage in Opioid-Tolerant Patients
- Provide ventilatory support and obtain intravenous access as clinically indicated. Judicious use of naloxone or another opioid antagonist may be warranted in some instances, but at the risk of precipitating an acute withdrawal syndrome.
General Considerations for Overdose
- Management of severe Fentanyl overdose includes: securing a patent airway, assisting or controlling ventilation and establishing intravenous access. In the presence of hypoventilation or apnea, assist or control ventilation, and administer oxygen as indicated.
- Carefully observe and appropriately manage patients with overdose until their clinical condition is well controlled.
- Although muscle rigidity interfering with respiration has not been seen following the use of Fentanyl, this is possible with fentanyl and other opioids. If it occurs, manage it by using assisted or controlled ventilation, by an opioid antagonist, and as a final alternative, by a neuromuscular blocking agent.
Pharmacology
Mechanism of Action
- Fentanyl is a pure opioid agonist whose principal therapeutic action is analgesia. Other members of the class known as opioid agonists include substances such as morphine, oxycodone, hydromorphone, codeine, and hydrocodone.
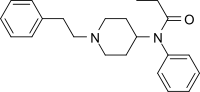
Structure
- Fentanyl (fentanyl) sublingual tablet is a solid formulation of fentanyl citrate, a potent opioid analgesic intended for oral sublingual administration. Fentanyl is formulated as a white tablet available in six strengths, distinguishable by the shape of the tablet and by de-bossing on the tablet surface.
- Active Ingredient: Fentanyl citrate, USP is N-(1-Phenethyl-4-piperidyl) propionanilide citrate (1:1). Fentanyl is a highly lipophilic compound (octanol-water partition coefficient at pH 7.4 is 816:1) that is freely soluble in organic solvents and sparingly soluble in water (1:40). The molecular weight of the free base is 336.5 (the citrate salt is 528.6). The pKa of the tertiary nitrogens are 7.3 and 8.4. The compound has the following structural formula:

- All tablet strengths are expressed as the amount of fentanyl free base, e.g., the 100 mcg strength tablet contains 100 mcg of fentanyl free base.
- Inactive Ingredients: Croscarmellose sodium, magnesium stearate, mannitol, and silicified microcrystalline cellulose.
Pharmacodynamics
- Pharmacological effects of opioid agonists include anxiolysis, euphoria, feelings of relaxation, respiratory depression, constipation, miosis, cough suppression, and analgesia. Like all pure opioid agonist analgesics, with increasing doses there is increasing analgesia, unlike with mixed agonist/antagonists or non-opioid analgesics, where there is a limit to the analgesic effect with increasing doses. With pure opioid agonist analgesics, there is no defined maximum dose; the ceiling to analgesic effectiveness is imposed only by side effects, the more serious of which may include somnolence and respiratory depression.
Analgesia
- In general, the effective concentration and the concentration at which toxicity occurs increase with increasing tolerance with any and all opioids. The rate of development of tolerance varies widely among individuals. As a result, individually titrate the dose of Fentanyl to achieve the desired effect [see Dosage and Administration].
Central Nervous System
- The precise mechanism of the analgesic action is unknown although fentanyl is known to be a μ-opioid receptor agonist. Specific CNS opioid receptors for endogenous compounds with opioid-like activity have been identified throughout the brain and spinal cord and play a role in the analgesic effects of this drug.
- Fentanyl produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves both a reduction in the responsiveness of the brain stem to increases in carbon dioxide and to electrical stimulation.
- Fentanyl causes miosis even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origin may produce similar findings).
Gastrointestinal System
- Fentanyl causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach and in the duodenum. Digestion of food is delayed in the small intestine and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone may be increased to the point of spasm resulting in constipation. Other opioid induced-effects may include a reduction in gastric, biliary and pancreatic secretions, spasm of the sphincter of Oddi, and transient elevations in serum amylase.
Cardiovascular System
- Fentanyl may produce release of histamine with or without associated peripheral vasodilation. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, sweating, and/or orthostatic hypotension.
Endocrine System
- Opioid agonists have been shown to have a variety of effects on the secretion of hormones. Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin secretion, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon in humans and other species (e.g., rats and dogs). Thyroid stimulating hormone (TSH) has been shown to be both inhibited and stimulated by opioids.
Respiratory System
- All opioid mu-receptor agonists, including fentanyl, produce dose-dependent respiratory depression. The risk of respiratory depression is less in patients receiving chronic opioid therapy who develop tolerance to these effects. Peak respiratory depressive effects may be seen as early as 15 to 30 minutes from the start of oral transmucosal fentanyl citrate administration and may persist for several hours.
- Serious or fatal respiratory depression can occur even at recommended doses. Fentanyl depresses the cough reflex as a result of its CNS activity. Although not observed with oral transmucosal fentanyl products in clinical trials, fentanyl given rapidly by intravenous injection in large doses may cause rigidity in the muscles of respiration resulting in respiratory difficulties. Therefore, be aware of this potential complication [see Boxed Warning - Warnings: Importance Of Proper Patient Selection and Potential for Abuse, Contraindications, Warnings And Precautions, Adverse Reactions, and Overdosage].
Pharmacokinetics
Absorption
- Fentanyl is a highly lipophilic drug. Orally administered fentanyl undergoes pronounced hepatic and intestinal first pass effects. Absorption of fentanyl from Fentanyl sublingual tablets is mainly through the oral mucosa.
- The bioavailability of Fentanyl sublingual tablets has been calculated to be 54%.
- Dose proportionality across the 100 mcg to 800 mcg Fentanyl dose range has been demonstrated (Table 3). Mean plasma fentanyl levels following single doses of Fentanyl are shown in Figure 1. The median time to maximum plasma concentration (Tmax) across these four doses of Fentanyl varied from 30 to 60 minutes (range of 15 - 240 minutes).
- Figure 1: Mean (+/- SD) Plasma Fentanyl Concentration versus Time after Administration of Single Doses of 100 mcg, 200 mcg, 400 mcg and 800 mcg Fentanyl to Healthy Subjects

- In another study, dose proportionality between 800 mcg and 1600 mcg in Cmax and AUC has also been demonstrated.
- Pharmacokinetic studies have shown that multiple tablets are bioequivalent to single tablets of the equivalent dose.
Distribution
- Fentanyl is highly lipophilic. Animal data showed that following absorption, fentanyl is rapidly distributed to the brain, heart, lungs, kidneys and spleen followed by a slower redistribution to muscles and fat. The plasma protein binding of fentanyl is 80-85%. The main binding protein is alpha-1-acid glycoprotein, but both albumin and lipoproteins contribute to some extent. The free fraction of fentanyl increases with acidosis. The mean volume of distribution at steady state (Vss) was 4 L/kg.
Metabolism
- Fentanyl is metabolized in the liver and in the intestinal mucosa to norfentanyl by cytochrome P450 3A4 isoform. Norfentanyl was not found to be pharmacologically active in animal studies [see Drug Interactions].
Elimination
- Fentanyl is more than 90% eliminated by biotransformation to N-dealkylated and hydroxylated inactive metabolites. Less than 7% of the dose is excreted unchanged in the urine, and only about 1% is excreted unchanged in the feces. The metabolites are mainly excreted in the urine, while fecal excretion is less important. The total plasma clearance of fentanyl was 0.5 L/hr/kg (range 0.3 - 0.7 L/ hr/kg).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Long-term studies in animals have not been performed to evaluate the carcinogenic potential of fentanyl.
- Fentanyl citrate was not mutagenic in the in vitro Ames reverse mutation assay in S. typhimurium or E. coli, or the mouse lymphoma mutagenesis assay, and was not clastogenic in the in vivo mouse micronucleus assay.
- Fentanyl has been shown to impair fertility in rats at doses of 30 mcg/kg intravenously and 160 mcg/kg subcutaneously. Conversion to the human equivalent doses indicates that this is within the range of the human recommended dosing for Fentanyl.
Clinical Studies
- The efficacy of Fentanyl was investigated in a clinical trial in opioid tolerant adult patients experiencing breakthrough cancer pain. Breakthrough cancer pain was defined as a transient flare of moderate-to-severe pain occurring in patients with cancer experiencing persistent cancer pain otherwise controlled with maintenance doses of opioid medications including at least 60 mg morphine/day, 50 mcg transdermal fentanyl/hour, or an equianalgesic dose of another opioid for 1 week or longer. All patients were on stable doses of either long-acting oral opioids or transdermal fentanyl for their persistent cancer pain.
- A double-blind, placebo-controlled, crossover study was performed in patients with cancer to evaluate the effectiveness of Fentanyl for the treatment of breakthrough cancer pain. Open-label titration identified a dose of Fentanyl in which a patient obtained adequate analgesia with tolerable side effects, within the range of 100 mcg to 800 mcg. In the double-blind efficacy study, patients who identified a successful dose were randomized to a sequence of 10 treatments; seven with Fentanyl and three with placebo.
- Of the 131 patients who entered the titration phase of the study, 78 (60%) achieved a successful dose during the titration phase. Sixty- six patients entered the double-blind phase and 60 completed the study. The dose of Fentanyl was determined by titration starting at 100 mcg. The final titrated dose of Fentanyl for breakthrough cancer pain was not predicted from the daily maintenance dose of opioid used to manage the persistent cancer pain. In a second open-label safety study using an identical titration regimen, 96 of 139 patients (69%) who entered the study titrated to a dose in which the patient obtained adequate analgesia with tolerable side effects during the titration phase. Table 4 presents the final titrated dose for both the double-blind efficacy and open-label safety studies.

How Supplied
Storage and Handling
- Fentanyl is supplied in individually sealed child-resistant blister packages contained in a cardboard outer carton, in pack sizes of 12 (100 mcg, 200 mcg, 300 mcg and 400 mcg strengths) or 32 (all strengths) tablets. The packaging is color-coded for each Fentanyl tablet strength.
- The amount of fentanyl contained in Fentanyl can be fatal to a child, individual for whom it is not prescribed or non-opioid tolerant adult. * Patients and their caregivers must be instructed to keep Fentanyl out of the reach of children [see Boxed Warning - Warnings: Potential For Abuse and Importance Of Proper Patient Selection and Warnings And Precautions , and Patient Counseling Information].
- Store at 20-25°C (68-77°F); excursions permitted between 15-30°C (59-86°F) [see USP Controlled Room Temperature]. Protect from moisture.
Disposal of Fentanyl
- Patients and their household members must be advised to dispose of any tablets remaining from a prescription as soon as they are no longer needed. Instructions are included in Patient Counseling Information and in the Medication Guide.
- To dispose of any unused Fentanyl tablets, remove them from the blister cards and flush down the toilet. Do not dispose of the Fentanyl blister cards or cartons down the toilet.
- If additional assistance is required, call Galena Biopharma, Inc. at 1-888-227-8725.
Storage
- Fentanyl is supplied in six dosage strengths. Tablets are supplied in child-resistant, protective blister cards with peelable foil. Each blister card contains 4 tablets, in pack sizes of 12 (100 mcg, 200 mcg, 300 mcg and 400 mcg strengths) or 32 (all strengths) tablets. Each tablet is white in color, with the strength distinguishable by the shape of the dosage unit and by de-bossing on the tablet surface:

Images
Drug Images
{{#ask: Page Name::Fentanyl (sublingual) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Fentanyl (sublingual) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Patient/Caregiver Instructions
- Before initiating treatment with Fentanyl, explain the statements below to patients and/or caregivers. Instruct patients to read the Medication Guide each time Fentanyl is dispensed because new information may be available.
- TIRF REMS Access Program
- Outpatients must be enrolled in the TIRF REMS Access program before they can receive Fentanyl.
- Allow patients the opportunity to ask questions and discuss any concerns regarding Fentanyl or the TIRF REMS Access program.
- As a component of the TIRF REMS Access program, prescribers must review the contents of the Fentanyl Medication Guide with every patient before initiating treatment with Fentanyl.
- Advise the patient that Fentanyl is available only from pharmacies that are enrolled in the TIRF REMS Access program, and provide them with the telephone number and website for information on how to obtain the drug.
- Advise the outpatient that only enrolled health care providers may prescribe Fentanyl.
- Patient must sign the Patient-Prescriber Agreement to acknowledge that they understand the risks of Fentanyl.
- Advise patients that they may be requested to participate in a survey to evaluate the effectiveness of the TIRF REMS Access program.
- Instruct patients and their caregivers that Fentanyl contains medicine in an amount that could be fatal in children, in individuals for whom Fentanyl is not prescribed, and in those who are not opioid tolerant. Patients and their caregivers must be instructed to keep Fentanyl, both used and unused dosage units, out of the reach of children. Patients and their caregivers must be instructed to dispose of any unneeded tablets remaining from a prescription as soon as possible [see How Supplied/Storage and Handling (16.2), and Warnings and Precautions (5.2).]
- Instruct patients and their caregivers to read the Medication Guide each time Fentanyl is dispensed because new information may be available.
- Instruct patients not to take Fentanyl for acute pain, postoperative pain, pain from injuries, headache, migraine, or any other short- term pain, even if they have taken other opioid analgesics for these conditions.
- Instruct patients on the meaning of opioid tolerance and Fentanyl is only to be used as a supplemental pain medication for patients with pain requiring regular opioids, who have developed tolerance to the opioid medication and who need additional opioid treatment of breakthrough pain episodes.
- Instruct that if they are not taking an opioid medication on a regular around-the-clock basis, they must not take Fentanyl.
- You must not take more than 2 doses of Fentanyl for each episode of breakthrough cancer pain.
- You must wait two hours before treating a new episode of breakthrough pain with Fentanyl.
- Instruct patients NOT to share Fentanyl and that sharing Fentanyl with anyone else could result in the other individual's death due to overdose.
- Advise patients that Fentanyl contains fentanyl, which is a pain medication similar to hydromorphone, methadone, morphine, oxycodone, and oxymorphone.
- Advise patients that the active ingredient in Fentanyl, fentanyl, is a drug that some people abuse. Fentanyl is to be taken only by the patient for whom it was prescribed, and protected from theft or misuse in the work or home environments.
- Instruct patients to talk to their doctor if breakthrough pain is not alleviated or worsens after taking Fentanyl.
- Instruct patients to use Fentanyl exactly as prescribed by their doctor and not to take Fentanyl more often than prescribed.
- Caution patients that Fentanyl can affect a person's ability to perform activities that require a high level of attention (such as driving or using heavy machinery). Warn patients taking Fentanyl of these dangers and counsel accordingly.
- Warn patients not to combine Fentanyl with alcohol, sleep aids, or tranquilizers except by order of the prescribing physician, because dangerous additive effects may occur resulting in serious injury or death.
- Inform female patients that if they become pregnant or plan to become pregnant during treatment with Fentanyl to ask their doctor about the effects that Fentanyl (or any medicine) may have on them and their unborn child.
Disposal of Unopened Fentanyl Blister Packages When No Longer Needed
- Advise patients and their household members to dispose of any unopened packs remaining from a prescription as soon as they are no longer needed.
- Instruct patients that, to dispose of any unused Fentanyl tablets, remove them from the blister cards and flush them down the toilet. Do not dispose of the Fentanyl blister cards or cartons down the toilet.
- Detailed instructions for the proper storage, administration, disposal, and important instructions for managing an overdose of Fentanyl are provided in the Fentanyl Medication Guide. Ensure patients read this information in its entirety and give them an opportunity to have their questions answered.
- In the event that a caregiver requires additional assistance in disposing of excess units that remain in the home after the drug is no longer needed, instruct them to call the toll-free number for Galena Biopharma, Inc. 1-888-227-8725 or seek assistance from their local DEA office.
- Medication Guide
- Fentanyl® (AB-stral) CII
(fentanyl)
- Sublingual tablets
- 100 mcg, 200 mcg, 300 mcg, 400 mcg, 600 mcg, 800 mcg

- Read this Medication Guide completely before you start taking Fentanyl, and each time you get a new prescription. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment. Be sure to share this important information with members of your household and other caregivers.
What is the most important information I should know about Fentanyl?
- Fentanyl can cause life-threatening breathing problems which can lead to death.
- Do not take Fentanyl if you are not opioid tolerant.
- If you stop taking your around-the-clock opioid pain medicine for your cancer pain, you must stop taking Fentanyl. You may no longer be opioid tolerant. Talk to your healthcare provider about how to treat your pain.
- Take Fentanyl exactly as prescribed by your healthcare provider.
- You must not take more than 2 doses of Fentanyl for each episode of breakthrough cancer pain.
- You must wait two hours before treating a new episode of breakthrough pain with Fentanyl. See the Medication Guide section "How should I take Fentanyl?" and the Patient Instructions for Use at the end of this Medication Guide for detailed information about how to take Fentanyl the right way.
- Do not switch from Fentanyl to other medicines that contain fentanyl without talking with your healthcare provider. The amount of fentanyl in a dose of Fentanyl is not the same as the amount of fentanyl in other medicines that contain fentanyl. Your healthcare provider will prescribe a starting dose of Fentanyl that may be different than other fentanyl containing medicines you may have been taking.
- Do not take Fentanyl for short-term pain that you would expect to go away in a few days, such as:
- Pain after surgery
- Headache or migraine
- Dental pain
- Never give Fentanyl to anyone else, even if they have the same symptoms you have. It may harm them or even cause death.
- Fentanyl is a federally controlled substance (CII) because it is a strong opioid (narcotic) pain medicine that can be misused by people who abuse prescription medicines or street drugs.
- Prevent theft, misuse or abuse. Keep Fentanyl in a safe place to protect it from being stolen. Fentanyl can be a target for people who abuse opioid (narcotic) medicines or street drugs.
- Selling or giving away this medicine is against the law.
- Fentanyl is available only through a program called the TIRF (Transmucosal Immediate-Release Fentanyl) REMS (Risk Evaluation and Mitigation Strategy) Access program. To receive Fentanyl, you must:
- Talk to your healthcare provider
- Understand the benefits and risks of Fentanyl
- Agree to all of the instructions
- Sign the Patient-Prescriber Agreement form
What is Fentanyl?
- Fentanyl is a prescription medicine that contains the medicine fentanyl.
- Fentanyl is used to manage breakthrough pain in adults with cancer (18 years of age and older) who are already routinely taking other opioid pain medicines around-the-clock for cancer pain.
- Fentanyl is started only after you have been taking other opioid pain medicines and your body has become used to them (you are opioid tolerant). Do not use Fentanyl if you are not opioid tolerant.
- Fentanyl is a small tablet that is placed on the floor of the mouth under your tongue (sublingual) and allowed to dissolve.
- You must stay under your healthcare provider's care while taking Fentanyl.
- Fentanyl is only:
- Available through the TIRF REMS Access program
- Given to people who are opioid tolerant
- It is not known if Fentanyl is safe and effective in children under 18 years of age.
Who should not take Fentanyl?
- Do not take Fentanyl:
- If you are not opioid tolerant. Opioid tolerant means that you are already taking other opioid pain medicines around-the- clock for your cancer pain, and your body is used to these medicines.
- For short-term pain that you would expect to go away in a few days, such as:
- Pain after surgery
- Headache or migraine
- Dental pain
- If you are allergic to any of the ingredients in Fentanyl. See the end of this Medication Guide for a complete list of other ingredients in Fentanyl.
What should I tell my healthcare provider before taking Fentanyl?
- Before taking Fentanyl, tell your healthcare provider if you:
- Have trouble breathing or lung problems such as asthma, wheezing, or shortness of breath
- Have or had a head injury or brain problem
- Have liver or kidney problems
- Have seizures
- Have a slow heart rate or other heart problems
- Have low blood pressure
- Have mental health problems including major depression, schizophrenia or hallucinations (seeing or hearing things that are not there)
- Have a past or present drinking problem (alcoholism), or a family history of drinking problems
- Have a past or present drug abuse problem or addiction problem, or a family history of a drug abuse problem or addiction problem
- Have any other medical conditions
- Are pregnant or plan to become pregnant. Fentanyl may cause serious harm to your unborn baby.
- Are breastfeeding or plan to breastfeed. Fentanyl can pass into your breast milk. It can cause serious harm to your baby. You should not use Fentanyl while breastfeeding.
- Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Some medicines may cause serious or life-threatening side effects when taken with Fentanyl. Sometimes, the doses of certain medicines and Fentanyl may need to be changed if used together.
- Do not take any medicine while using Fentanyl until you have talked to your healthcare provider. Your healthcare provider will tell you if it is safe to take other medicines while you are using Fentanyl.
- Be very careful about taking other medicines that may make you sleepy, such as other pain medicines, anti-depressants, sleeping pills, anti-anxiety medicines, antihistamines, or tranquilizers.
- Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take Fentanyl?
- Before you can begin to take Fentanyl:
- Your healthcare provider will explain the TIRF REMS Access program to you.
- You will sign the TIRF REMS Access program Patient-Prescriber Agreement form.
- Fentanyl is only available at pharmacies that are part of the TIRF REMS Access program. Your healthcare provider will let you know the pharmacy closest to your home where you can have your Fentanyl prescription filled.
Taking Fentanyl
- Take Fentanyl exactly as prescribed. Do not take Fentanyl more often than prescribed.
- If you notice that your tablets are a different shape or color, be sure to check with your pharmacist to make sure you have the right strength of medicine.
- Do not suck, chew or swallow the tablet.
- See the detailed Patient Instructions for Use at the end of this Medication Guide for information about how to take Fentanyl the right way.
- Your healthcare provider will change the dose until you and your healthcare provider find the right dose for you.
- You must not use more than 2 doses of Fentanyl for each episode of breakthrough cancer pain:
- Take 1 dose for an episode of breakthrough cancer pain.
- If your breakthrough pain does not get better within 30 minutes after taking the first dose of Fentanyl, you can take 1 more dose of Fentanyl as instructed by your healthcare provider.
- If your breakthrough pain does not get better after the second dose of Fentanyl, call your healthcare provider for instructions. Do not take another dose of Fentanyl at this time.
- Wait at least 2 hours before treating a new episode of breakthrough cancer pain with Fentanyl:
- If you only need to take 1 dose of Fentanyl for an episode of breakthrough pain, you must wait 2 hours from the time of that dose to take a dose of Fentanyl for a new episode of breakthrough pain
- If you need to take 2 doses of Fentanyl for an episode of breakthrough pain, you must wait 2 hours after the second dose to take a dose of Fentanyl for a new episode of breakthrough pain.
- It is important for you to keep taking your around-the-clock opioid pain medicine while taking Fentanyl.
- Talk to your healthcare provider if your dose of Fentanyl does not relieve your breakthrough cancer pain. Your healthcare provider will decide if your dose of Fentanyl needs to be changed.
- Talk to your healthcare provider if you have more than 4 episodes of breakthrough cancer pain per day. The dose of your around- the-clock opioid pain medicine may need to be adjusted.
- If you take too much Fentanyl or overdose, you or your caregiver should call for emergency medical help or have someone take you to the nearest hospital emergency room right away.
What should I avoid while taking Fentanyl?
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how Fentanyl affects you. Fentanyl can make you sleepy. Ask your healthcare provider when it is okay to do these activities.
- Do not drink alcohol while using Fentanyl. It can increase your chance of getting dangerous side effects.
What are the possible side effects of Fentanyl?
- Fentanyl can cause serious side effects, including:
- Breathing problems that can become life-threatening. See "What is the most important information I should know about Fentanyl?"
- Call your healthcare provider or get emergency medical help right away if you:
- Have trouble breathing
- Have drowsiness with slowed breathing
- Have shallow breathing (little chest movement with breathing)
- Feel faint, very dizzy, confused, or have other unusual symptoms
- These symptoms can be a sign that you have taken too much Fentanyl or the dose is too high for you. These symptoms may lead to serious problems or death if not treated right away. If you have any of these symptoms, do not take any more Fentanyl until you have talked to your healthcare provider.
- Decreased blood pressure. This can make you feel dizzy or lightheaded if you get up too fast from sitting or lying down.
- Physical dependence. Do not stop taking Fentanyl or any other opioid, without talking to your healthcare provider. You could become sick with uncomfortable withdrawal symptoms because your body has become used to these medicines. Physical dependency is not the same as drug addiction.
- A chance of abuse or addiction. This chance is higher if you are or have ever been addicted to or abused other medicines, street drugs, or alcohol, or if you have a history of mental health problems.
- The most common side effects of Fentanyl are:
- Nausea
- Sleepiness
- Headache
- Constipation (not often enough or hard bowel movements) is a very common side effect of pain medicines (opioids) including Fentanyl and is unlikely to go away without treatment. Talk to your healthcare provider about dietary changes, and the use of laxatives (medicines to treat constipation) and stool softeners to prevent or treat constipation while taking Fentanyl.
- Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
- These are not all the possible side effects of Fentanyl. For more information, ask your healthcare provider or pharmacist.
- Call your doctor for medical advice about your side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Fentanyl?
- Always keep Fentanyl in a safe place away from children and from anyone for whom it has not been prescribed. Protect Fentanyl from theft.
- Store Fentanyl at room temperature, 59°F to 86°F (15°C to 30°C) until ready to use.
- Keep Fentanyl in the original blister unit. Do not remove Fentanyl tablets from their blister packaging for storage in a temporary container, such as a pillbox.
How should I dispose of unopened Fentanyl tablets when they are no longer needed?
- Dispose of any unopened Fentanyl units remaining from a prescription as soon as you no longer need them:
- Remove the tablets from the blister cards and flush them down the toilet.
- Do not flush the Fentanyl blister cards, units or cartons down the toilet.
- If you need help with disposal of Fentanyl, call Galena Biopharma, Inc.., at 1-888-227-8725 or call your local Drug Enforcement Agency (DEA) office.
General information about Fentanyl
- Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Use Fentanyl only for the purpose for which it was prescribed. Do not give Fentanyl to other people, even if they have the same symptoms you have. Fentanyl can harm other people and even cause death. Sharing Fentanyl is against the law.
- This Medication Guide summarizes the most important information about Fentanyl. If you would like more information, talk with your healthcare provider or pharmacist. You can ask your pharmacist or healthcare provider for information about Fentanyl that is written for healthcare professionals.
- For more information about the TIRF REMS Access program, go to www.TIRFREMSAccess.com or call 1-866-822-1483.
What are the ingredients in Fentanyl?
- Active Ingredient: fentanyl citrate
- Inactive Ingredients: croscarmellose sodium, magnesium stearate, mannitol, and silicified microcrystalline cellulose.
Patient Instructions for Use
- Before you take Fentanyl, it is important that you read the Medication Guide and these Patient Instructions for Use. Be sure that you read, understand, and follow these Patient Instructions for Use so that you take Fentanyl the right way. Ask your healthcare provider or pharmacist if you have questions about the right way to take Fentanyl.
- When you get an episode of breakthrough pain, take the dose prescribed by your healthcare provider as follows:
- If your mouth is dry, take a sip of water to moisten it. Spit out or swallow the water. Dry your hands if they are wet before you handle Fentanyl tablets.
- Fentanyl comes in a blister card with 4 blister units. Each blister unit contains an Fentanyl tablet. It is important that the tablet stays sealed in the blister unit until you are ready to use it.
- When you are ready to take an Fentanyl tablet, pull apart 1 of the blister units from the blister card by tearing along the dotted lines (perforations) until it is fully separated. (See Figures 1 and 2)

- If more than 1 tablet is required, spread them around the floor of your mouth under your tongue.
- Let the tablet dissolve completely.
- Fentanyl dissolves under your tongue and will be absorbed by your body to help provide relief for your breakthrough cancer pain.
- Do not suck, chew or swallow the tablet.
- You should not drink or eat anything until the tablet has completely dissolved under your tongue and you can no longer feel it in your mouth.
- Manufactured by:
- Pharmaceutics International, Inc.
- Hunt Valley, MD 21031
- Manufactured for:
- Galena Biopharma, Inc.
- Lake Oswego, OR 97034
- Issued: July 2013
- This Medication Guide has been approved by the U.S. Food and Drug Administration. Copyright © 2013, Galena Biopharma, Inc. All rights reserved.
- Fentanyl and Galena Biopharma are trademarks owned by the Galena Biopharma, Inc.
Precautions with Alcohol
Alcohol-Fentanyl interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Fentanyl (sublingual) Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Fentanyl (sublingual) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Janssen Pharmaceuticals (Duragesic)
- ↑ Hess R, Stiebler G, Herz A (June 1972). "Pharmacokinetics of fentanyl in man and the rabbit". Eur. J. Clin. Pharmacol. 4 (3): 137–41. doi:10.1007/BF00561135. PMID 4655287.
{{#subobject:
|Page Name=Fentanyl (sublingual) |Pill Name=No image.jpg |Drug Name=Fentanyl |Pill Ingred=Croscarmellose sodium, magnesium stearate, mannitol, cellulose, microcrystalline|+sep=; |Pill Imprint=8 |Pill Dosage=0.8 Sublingual Tablet mg |Pill Color=Blue|+sep=; |Pill Shape=Capsule |Pill Size (mm)=10.00 |Pill Scoring=1 |Pill Image= |Drug Author=Galena Biopharma, Inc. |NDC=57881-338-32
}}
{{#subobject:
|Page Name=Fentanyl (sublingual) |Pill Name=No image.jpg |Drug Name=Fentanyl |Pill Ingred=Croscarmellose sodium, magnesium stearate, mannitol, cellulose, microcrystalline|+sep=; |Pill Imprint=4 |Pill Dosage=0.4 Sublingual Tablet mg |Pill Color=Purple|+sep=; |Pill Shape=Diamond |Pill Size (mm)=10.00 |Pill Scoring=1 |Pill Image= |Drug Author=Galena Biopharma, Inc. |NDC=57881-334-32
}}
{{#subobject:
|Page Name=Fentanyl (sublingual) |Pill Name=No image.jpg |Drug Name=Fentanyl |Pill Ingred=Croscarmellose sodium, magnesium stearate, mannitol, cellulose, microcrystalline|+sep=; |Pill Imprint=2 |Pill Dosage=0.2 Sublingual Tablet mg |Pill Color=Orange|+sep=; |Pill Shape=Oval |Pill Size (mm)=10.00 |Pill Scoring=1 |Pill Image= |Drug Author=Galena Biopharma, Inc. |NDC=57881-334-32
}}
{{#subobject:
|Page Name=Fentanyl (sublingual) |Pill Name=No image.jpg |Drug Name=Fentanyl |Pill Ingred=Croscarmellose sodium, magnesium stearate, mannitol, cellulose, microcrystalline|+sep=; |Pill Imprint=1 |Pill Dosage=0.1 Sublingual Tablet mg |Pill Color=Blue|+sep=; |Pill Shape=Round |Pill Size (mm)=10.00 |Pill Scoring=1 |Pill Image= |Drug Author=Galena Biopharma, Inc. |NDC=57881-334-32
}}
{{#subobject:
|Page Name=Fentanyl (sublingual) |Pill Name=No image.jpg |Drug Name=Fentanyl |Pill Ingred=Croscarmellose sodium, magnesium stearate, mannitol, cellulose, microcrystalline|+sep=; |Pill Imprint=6 |Pill Dosage=0.6 Sublingual Tablet mg |Pill Color=Turquoise|+sep=; |Pill Shape=SemiCircle |Pill Size (mm)=10.00 |Pill Scoring=1 |Pill Image= |Drug Author=Galena Biopharma, Inc. |NDC=57881-334-32
}}
{{#subobject:
|Page Name=Fentanyl (sublingual) |Pill Name=No image.jpg |Drug Name=Fentanyl |Pill Ingred=Croscarmellose sodium, magnesium stearate, mannitol, cellulose, microcrystalline|+sep=; |Pill Imprint=3 |Pill Dosage=0.3 Sublingual Tablet mg |Pill Color=Brown|+sep=; |Pill Shape=Triangular |Pill Size (mm)=10.00 |Pill Scoring=1 |Pill Image= |Drug Author=Galena Biopharma, Inc. |NDC=57881-334-32
}}
{{#subobject:
|Label Page=Fentanyl (sublingual) |Label Name=Fentanyl label.png
}}