Euthyroid sick syndrome classification: Difference between revisions
Akshun Kalia (talk | contribs) |
Akshun Kalia (talk | contribs) |
||
| (27 intermediate revisions by 5 users not shown) | |||
| Line 2: | Line 2: | ||
{{Euthyroid sick syndrome}} | {{Euthyroid sick syndrome}} | ||
{{CMG}}; {{AE}} | {{CMG}}; {{AE}}{{Akshun}} | ||
==Overview== | ==Overview== | ||
[[Euthyroid]] sick syndrome may be classified according to the level of [[thyroid hormones]] and the severity of the underlying [[disease]] into mild, moderate, severe, and [[recovery]] phase. | |||
==Classification== | ==Classification== | ||
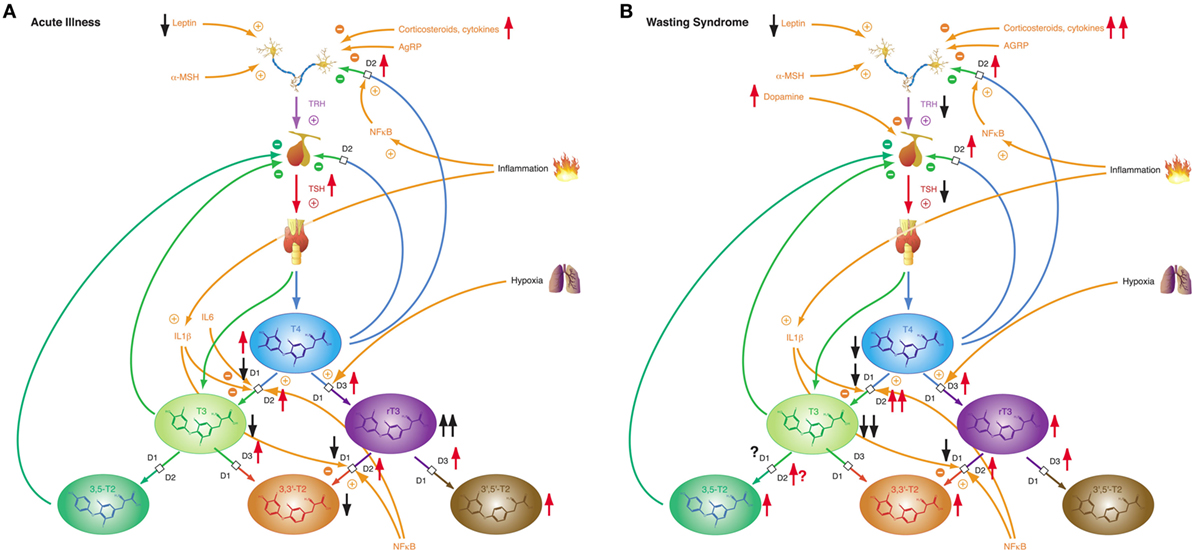
Euthyroid sick syndrome may be classified according to the level of thyroid hormones and the severity of the underlying disease. Depending upon the severity and duration of the [[Stress (medicine)|stress]] inducing [[condition]], the [[thyroid-stimulating hormone]]([[TSH]]), [[thyroxine]] ([[T4]]), and [[free T4]] ([[FT4]]) are affected in variable proportions. The drop in levels of [[T3]] and [[T4]] | [[File:Acute NTIS and Wasting Syndrome.jpeg|thumb|left|Phenotypes of NTIS|Source: Courtesy of Chatzitomaris A et al Endocrinol. 8:163. doi: 10.3389/fendo.2017.00163 (2017)made freely available under a Creative Commons Attribution License (CC BY) ]] | ||
Euthyroid sick syndrome may be classified according to the level of [[thyroid hormones]] and the severity of the underlying [[disease]]. Depending upon the severity and duration of the [[Stress (medicine)|stress]] inducing [[condition]], the [[thyroid-stimulating hormone]] ([[TSH]]), [[thyroxine]] ([[T4]]), and [[free T4]] ([[FT4]]) are affected in variable proportions. The drop in levels of [[T3]] and [[T4]] is associated with more severe illnesses. On the basis of [[thyroid hormone]] levels euthyroid sick syndrome can be categorized into:<ref name="pmid19007679">{{cite journal |vauthors=Golombek SG |title=Nonthyroidal illness syndrome and euthyroid sick syndrome in intensive care patients |journal=Semin. Perinatol. |volume=32 |issue=6 |pages=413–8 |year=2008 |pmid=19007679 |doi=10.1053/j.semperi.2008.09.010 |url=}}</ref><ref name="pmid27403906">{{cite journal |vauthors=Frączek MM, Gackowski A, Przybylik-Mazurek E, Nessler J |title=[The relation between the low T3 syndrome in the clinical course of myocardial infarction and heart failure] |language=Polish |journal=Pol. Merkur. Lekarski |volume=40 |issue=240 |pages=380–3 |year=2016 |pmid=27403906 |doi= |url=}}</ref><ref name="pmid24845024">{{cite journal |vauthors=Van den Berghe G |title=Non-thyroidal illness in the ICU: a syndrome with different faces |journal=Thyroid |volume=24 |issue=10 |pages=1456–65 |year=2014 |pmid=24845024 |pmc=4195234 |doi=10.1089/thy.2014.0201 |url=}}</ref><ref name="pmid23214076">{{cite journal |vauthors=Murakami M |title=[Nonthyroidal illness (NTI)] |language=Japanese |journal=Nippon Rinsho |volume=70 |issue=11 |pages=2005–10 |year=2012 |pmid=23214076 |doi= |url=}}</ref><ref name="pmid27065175">{{cite journal |vauthors=Lee S, Farwell AP |title=Euthyroid Sick Syndrome |journal=Compr Physiol |volume=6 |issue=2 |pages=1071–80 |year=2016 |pmid=27065175 |doi=10.1002/cphy.c150017 |url=}}</ref><ref name="pmid28775711">Chatzitomaris A, Hoermann R, Midgley JE, Hering S, Urban A, Dietrich B, Abood A, Klein HH, Dietrich JW. Thyroid Allostasis-Adaptive Responses of Thyrotropic Feedback Control to Conditions of Strain, Stress, and Developmental Programming. Front Endocrinol (Lausanne). 2017 Jul 20;8:163. {{doi|10.3389/fendo.2017.00163}}. {{PMID|28775711}}; PMCID PMC5517413</ref><ref>Dietrich JW, Landgrafe G, Fotiadou EH. TSH and Thyrotropic Agonists: Key Actors in Thyroid Homeostasis. J Thyroid Res. 2012;2012:351864. {{doi|10.1155/2012/351864}}. {{PMID|23365787}}; PMCID PMC3544290.</ref> | |||
Additionally, two phenotypes of euthyroid sick syndrome use to be distinguished, depending on the question if it occurs over short time in acute illness or if it represents a chronic condition (referred to as ''wasting syndrome'')<ref name="pmid24845024"/>. In the latter case, concentrations of T3 are even more reduced, and [[3,5-T2]] concentrations are increased<ref name="pmid28775711"/>. | |||
{| | |||
{{familytree/start}} | |||
{{familytree | | | | | | | | | | |A01 | | | | | |A01=Euthyroid Sick Syndrome | |||
|boxstyle_A01 =background-color: #aef; | |||
}} | |||
( | {{familytree | |,|-|-|-|-|-|-|v|-|-|^|-|-|-|v|-|-|-|-|-|-|.| }} | ||
{{familytree |B01 | | | | |B02 | | | | |B03 | | | | |B04 |B01=Mild euthyroid sick syndrome|B02=Moderate euthyroid sick syndrome|B03=Severe euthyroid sick syndrome|B04=Recovery phase | |||
|boxstyle_B01 = background-color: #ff0; | |||
|boxstyle_B02 = background-color: #f90; | |||
|boxstyle_B03 = background-color: #f66; | |||
|boxstyle_B04 = background-color: #afa; | |||
}} | |||
|- | {{familytree | |!| | | | | | |!| | | | | | |!| | | | | | |!| }} | ||
| | {{familytree |boxstyle=text-align: left; |C01 | | | | |C02 | | | | |C03 | | | | |C04 |C01=•Decreased [[T3]]<br>•Normal [[T4]], [[FT4]] and [[TSH]]<br>•Increased [[reverse T3]]| C02= • Decreased [[T3]]<br>• Normal/decreased [[FT4]] and [[TSH]]<br>• Increased [[reverse T3]] | C03=• Decreased [[T3]], [[T4]] and [[TSH]]<br>• Normal/decreased [[FT4]]<br>• Increased reverse [[T3]]|C04=• Normal/decreased [[T3]] <br>• Normal/increased [[T4]], [[FT4]] and [[TSH]]<br>• Normal/increased [[reverse T3]] | ||
| | |boxstyle_C01 = background-color: #ff0; | ||
| | |boxstyle_C02 = background-color: #f90; | ||
| | |boxstyle_C03 = background-color: #f66; | ||
| | |boxstyle_C04 = background-color: #afa; | ||
| | }} | ||
|- | {{familytree/end}} | ||
|Moderate euthyroid sick syndrome | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
==References== | ==References== | ||
Latest revision as of 16:30, 28 November 2017
|
Euthyroid sick syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Euthyroid sick syndrome classification On the Web |
|
American Roentgen Ray Society Images of Euthyroid sick syndrome classification |
|
Risk calculators and risk factors for Euthyroid sick syndrome classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akshun Kalia M.B.B.S.[2]
Overview
Euthyroid sick syndrome may be classified according to the level of thyroid hormones and the severity of the underlying disease into mild, moderate, severe, and recovery phase.
Classification
Euthyroid sick syndrome may be classified according to the level of thyroid hormones and the severity of the underlying disease. Depending upon the severity and duration of the stress inducing condition, the thyroid-stimulating hormone (TSH), thyroxine (T4), and free T4 (FT4) are affected in variable proportions. The drop in levels of T3 and T4 is associated with more severe illnesses. On the basis of thyroid hormone levels euthyroid sick syndrome can be categorized into:[1][2][3][4][5][6][7]
Additionally, two phenotypes of euthyroid sick syndrome use to be distinguished, depending on the question if it occurs over short time in acute illness or if it represents a chronic condition (referred to as wasting syndrome)[3]. In the latter case, concentrations of T3 are even more reduced, and 3,5-T2 concentrations are increased[6].
| Euthyroid Sick Syndrome | |||||||||||||||||||||||||||||||||||||||||||||||
| Mild euthyroid sick syndrome | Moderate euthyroid sick syndrome | Severe euthyroid sick syndrome | Recovery phase | ||||||||||||||||||||||||||||||||||||||||||||
| •Decreased T3 •Normal T4, FT4 and TSH •Increased reverse T3 | • Decreased T3 • Normal/decreased FT4 and TSH • Increased reverse T3 | • Decreased T3, T4 and TSH • Normal/decreased FT4 • Increased reverse T3 | • Normal/decreased T3 • Normal/increased T4, FT4 and TSH • Normal/increased reverse T3 | ||||||||||||||||||||||||||||||||||||||||||||
References
- ↑ Golombek SG (2008). "Nonthyroidal illness syndrome and euthyroid sick syndrome in intensive care patients". Semin. Perinatol. 32 (6): 413–8. doi:10.1053/j.semperi.2008.09.010. PMID 19007679.
- ↑ Frączek MM, Gackowski A, Przybylik-Mazurek E, Nessler J (2016). "[The relation between the low T3 syndrome in the clinical course of myocardial infarction and heart failure]". Pol. Merkur. Lekarski (in Polish). 40 (240): 380–3. PMID 27403906.
- ↑ 3.0 3.1 Van den Berghe G (2014). "Non-thyroidal illness in the ICU: a syndrome with different faces". Thyroid. 24 (10): 1456–65. doi:10.1089/thy.2014.0201. PMC 4195234. PMID 24845024.
- ↑ Murakami M (2012). "[Nonthyroidal illness (NTI)]". Nippon Rinsho (in Japanese). 70 (11): 2005–10. PMID 23214076.
- ↑ Lee S, Farwell AP (2016). "Euthyroid Sick Syndrome". Compr Physiol. 6 (2): 1071–80. doi:10.1002/cphy.c150017. PMID 27065175.
- ↑ 6.0 6.1 Chatzitomaris A, Hoermann R, Midgley JE, Hering S, Urban A, Dietrich B, Abood A, Klein HH, Dietrich JW. Thyroid Allostasis-Adaptive Responses of Thyrotropic Feedback Control to Conditions of Strain, Stress, and Developmental Programming. Front Endocrinol (Lausanne). 2017 Jul 20;8:163. doi:10.3389/fendo.2017.00163. PMID 28775711; PMCID PMC5517413
- ↑ Dietrich JW, Landgrafe G, Fotiadou EH. TSH and Thyrotropic Agonists: Key Actors in Thyroid Homeostasis. J Thyroid Res. 2012;2012:351864. doi:10.1155/2012/351864. PMID 23365787; PMCID PMC3544290.