Esophageal cancer surgery
|
Esophageal cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Esophageal cancer surgery On the Web |
|
American Roentgen Ray Society Images of Esophageal cancer surgery |
|
Risk calculators and risk factors for Esophageal cancer surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Hadeel Maksoud M.D.[2]
Overview
The predominant therapy for esophageal cancer is surgical resection by esophagectomy. The disease must be localised in order for it to be operable. Adjunctive chemotherapy and radiation may be required in more advanced cases of esophageal cancer, and to shrink down a localised tumor so that it may become operable.
Esophagectomy
- Removing a segment of the esophagus is called an esophagectomy.[1][2][3]
- The disease must be localised in order for it to be operable.
- If a tumor is particularly large but still localised, it may be shrunk down first using chemotherapy and/or radiotherapy until the tumor becomes of a size that is operable.
- The procedure shortens the distance between the pharynx and the stomach.
- The stomach, or some other part of the gastrointestinal tract, such as the colon, is brought up into the chest cavity where it is interposed.
- There are several surgical approaches including:
- Transhiatal esophagectomy
- Cervical esophageal cancer resection
- Thoracic cancer resection
- Ivor-Lewis transthoracic esophagectomy
- Modified Ivor-Lewis transthoracic esophagectomy
- Tri-incisional esophagectomy
- Esophagogastric junction cancer resection
Surgical Considerations
- Patients with resectable tumors account for 20-30% of cases with esophageal cancer.[2][3]
- In patients with adenocarcinoma, surgery is recommended even if there is a good response with chemotherapy. Surgery achieves a higher rate of local control and less need for palliative maneuvers later on.
- Patients in this category should undergo surgery after having completed 4 to 6 weeks of chemotherapy or chemoradiotherapy.
- Unless, the patient is able to achieve cure without surgery or is unfit for surgery.
Indications
- The following are candidates for first line therapy with esophagectomy:[4][5]
- T1N0M0 lesions
- T2N0M0 lesions
- The patients with the following are candidates for esophagectomy following neoadjuvant chemotherapy or chemoradiotherapy:
- Thoracic esophageal or esophagogastric junction tumors and full-thickness (T3) involvement of the esophagus with/without nodal disease
- T4a disease with invasion of local structures (pericardium, pleura, and/or diaphragm only) that can be resected en bloc, and who are without evidence of metastatic disease to other organ.
Contraindications
The following are relative contraindications for esophagectomy:[6]
- Advanced age
- Associated with greater morbidity following esophagectomy
- Comorbid illness
- Obesity can lead to postoperative complications such as cardiorespiratory complications, anastomotic leakage, and wound infection
Indications for unresectability
The presence of metastatic disease:
- Such as peritoneal, lung, bone, adrenal, brain, or liver metastases, or extraregional lymph node spread
Surgery
Stage 0 Esophageal Cancer
Stage 0 squamous esophageal cancer is rarely seen in the United States, but surgery has been used for this stage of cancer[7]
Stage I Esophageal Cancer
Standard treatment options:
- Chemoradiation with subsequent surgery
- Surgery
Stage II Esophageal Cancer
Standard treatment options:
- Chemoradiation with subsequent surgery
- Chemoradiation alone
- Surgery alone
Stage III Esophageal Cancer
Standard treatment options:
- Chemoradiation with subsequent surgery
- Chemoradiation alone
Stage IV Esophageal Cancer
- At diagnosis, approximately 50% of patients with esophageal cancer will have metastatic disease and will be candidates for palliative therapy.[8]
- Standard treatment options:
- Chemoradiation with subsequent surgery (for patients with stage IVA disease)
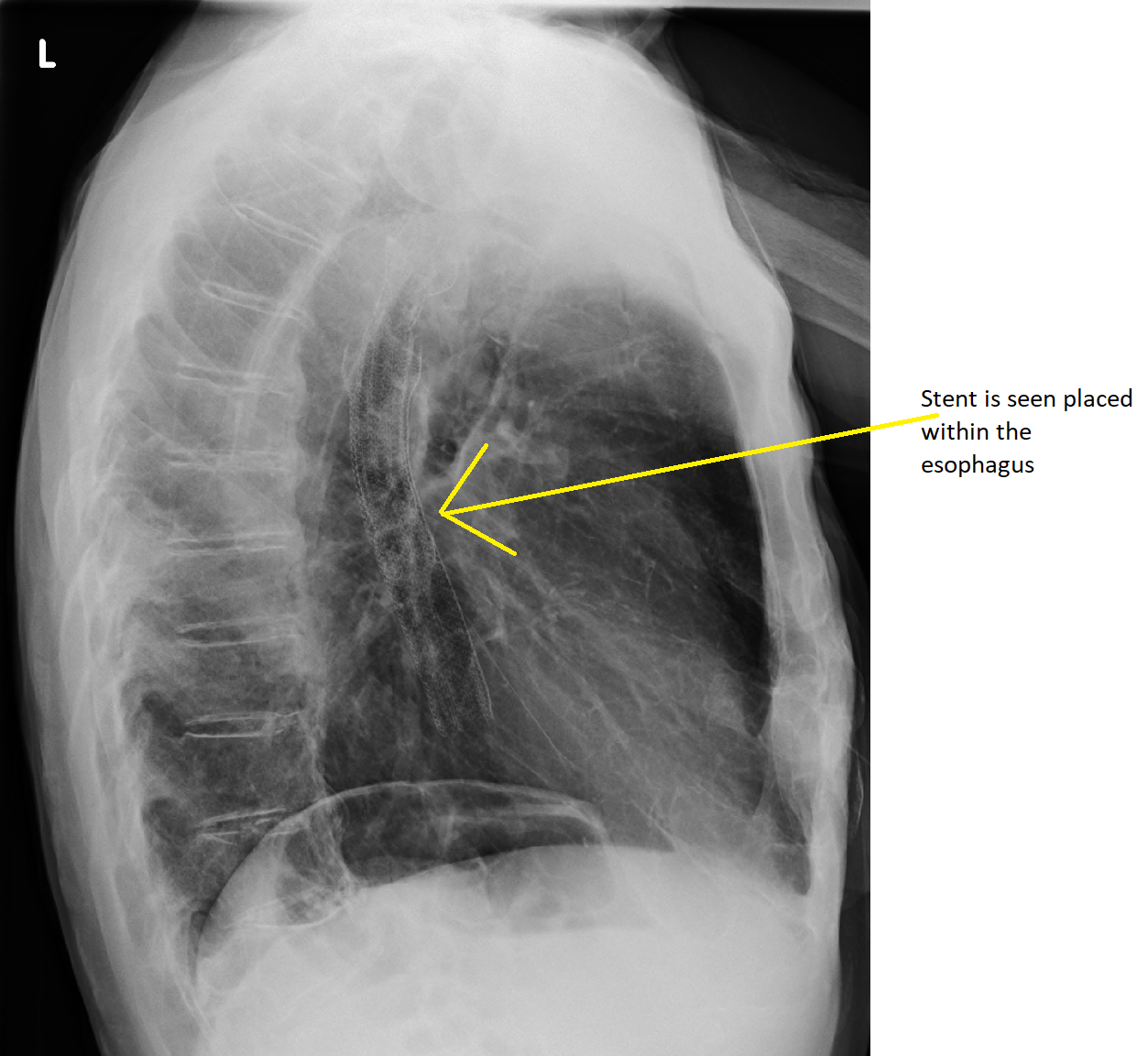
- Endoscopic-placed stents to provide palliation of dysphagia
- Radiation therapy with or without intraluminal intubation and dilation
- Intraluminal brachytherapy to provide palliation of dysphagia
- Nd:YAG laser endoluminal tumor destruction or electrocoagulation
- Chemotherapy has provided partial responses for patients with metastatic distal esophageal adenocarcinoma
Stenting
- If the patient cannot swallow at all, a stent may be inserted to keep the esophagus patent.[9]
- Stents may also assist in occluding fistulas.
- A nasogastric tube may be necessary to continue feeding while treatment for the tumor is given, and some patients may require a gastrostomy (feeding hole in the skin that gives direct access to the stomach).
- Nasogastric tube and gastrostomy are especially important if the patient tends to aspirate food or saliva into the airways, predisposing for aspiration pneumonia.
Laser therapy
- Laser therapy is described as the use of a high intensity beam of light to destroy malignant cells; it affects only the area it is focused on whilst unharming the healthy cells.[10][11]
- Laser therapy is given when tumors are inoperable because of their size, location and/or spread.
- Sometimes, the aim of laser therapy is palliation, to relieve some symptoms such as dysphagia and pain.
- Photodynamic therapy (PDT), a type of laser therapy, involving the use of drugs that are absorbed by cancer cells; when exposed to a particular wave length of light, the drugs become active and destroy the tumor cells.
Radiotherapy
- Radiotherapy is given before, during or after chemotherapy or surgery, and sometimes on its own to control symptoms.[12][13]
- In patients with localized disease but contraindications to surgery, "proton radiotherapy" may be used with curative intent.
References
- ↑ Wang HW, Chu PY, Kuo KT, Yang CH, Chang SY, Hsu WH, Wang LS (2006). "A reappraisal of surgical management for squamous cell carcinoma in the pharyngoesophageal junction". J Surg Oncol. 93 (6): 468–76. doi:10.1002/jso.20472. PMID 16615159.
- ↑ 2.0 2.1 Triboulet JP, Mariette C, Chevalier D, Amrouni H (2001). "Surgical management of carcinoma of the hypopharynx and cervical esophagus: analysis of 209 cases". Arch Surg. 136 (10): 1164–70. PMID 11585510.
- ↑ 3.0 3.1 Deschamps C, Nichols FC, Cassivi SD; et al. (2005). "Long-term function and quality of life after esophageal resection for cancer and Barrett's". Surgical Clinics of North America. 85 (3): 649–656. PMID 15927658.
- ↑ Wu AJ, Goodman KA (2015). "Clinical tools to predict outcomes in patients with esophageal cancer treated with definitive chemoradiation: are we there yet?". J Gastrointest Oncol. 6 (1): 53–9. doi:10.3978/j.issn.2078-6891.2014.099. PMC 4294820. PMID 25642338.
- ↑ Lin SH, Wang J, Allen PK, Correa AM, Maru DM, Swisher SG, Hofstetter WL, Liao Z, Ajani JA (2015). "A nomogram that predicts pathologic complete response to neoadjuvant chemoradiation also predicts survival outcomes after definitive chemoradiation for esophageal cancer". J Gastrointest Oncol. 6 (1): 45–52. doi:10.3978/j.issn.2078-6891.2014.054. PMC 4294819. PMID 25642337.
- ↑ Miao L, Chen H, Xiang J, Zhang Y (2015). "A high body mass index in esophageal cancer patients is not associated with adverse outcomes following esophagectomy". J. Cancer Res. Clin. Oncol. 141 (5): 941–50. doi:10.1007/s00432-014-1878-x. PMID 25428458.
- ↑ Affleck DG, Karwande SV, Bull DA, Haller JR, Stringham JC, Davis RK (2000). "Functional outcome and survival after pharyngolaryngoesophagectomy for cancer". Am. J. Surg. 180 (6): 546–50. PMID 11182415.
- ↑ "Esophageal Cancer Treatment".
- ↑ Bethge N, Sommer A, Vakil N (1997). "A prospective trial of self-expanding metal stents in the palliation of malignant esophageal strictures near the upper esophageal sphincter". Gastrointest. Endosc. 45 (3): 300–3. PMID 9087839.
- ↑ Haddad NG, Fleischer DE (1994). "Endoscopic laser therapy for esophageal cancer". Gastrointest. Endosc. Clin. N. Am. 4 (4): 863–74. PMID 7529119.
- ↑ Mellow MH, Pinkas H (1985). "Endoscopic laser therapy for malignancies affecting the esophagus and gastroesophageal junction. Analysis of technical and functional efficacy". Arch. Intern. Med. 145 (8): 1443–6. PMID 4026476.
- ↑ Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, Shank B, Solin LJ, Wesson M (1991). "Tolerance of normal tissue to therapeutic irradiation". Int. J. Radiat. Oncol. Biol. Phys. 21 (1): 109–22. PMID 2032882.
- ↑ SEAMAN WB, ACKERMAN LV (1957). "The effect of radiation on the esophagus; a clinical and histologic study of the effects produced by the betatron". Radiology. 68 (4): 534–41. doi:10.1148/68.4.534. PMID 13432180.