Erenumab: Difference between revisions
No edit summary |
No edit summary |
||
| Line 302: | Line 302: | ||
|PK=(Description) | |PK=(Description) | ||
|nonClinToxic=(Description) | |nonClinToxic=(Description) | ||
|clinicalStudies= | |clinicalStudies=*The efficacy of AIMOVIG was evaluated as a preventive treatment of episodic or chronic migraine in three randomized, double-blind, placebo-controlled studies: two studies in patients with episodic migraine (4 to 14 migraine days per month) (Study 1 and Study 2) and one study in patients with chronic migraine (≥ 15 headache days per month with ≥ 8 migraine days per month) (Study 3). The studies enrolled patients with a history of migraine, with or without aura, according to the International Classification of Headache Disorders (ICHD-III) diagnostic criteria. | ||
=====Episodic Migraine===== | |||
=== | *Study 1 (NCT 02456740) was a randomized, multi-center, 6-month, placebo-controlled, double-blind study evaluating AIMOVIG for the preventive treatment of episodic migraine. A total of 955 patients with a history of episodic migraine were randomized to receive either AIMOVIG 70 mg (N = 317), AIMOVIG 140 mg (N = 319), or placebo (N = 319) by subcutaneous injection once monthly (QM) for 6 months. Patients were allowed to use acute headache treatments including migraine-specific medications (i.e., triptans, ergotamine derivatives) and NSAIDs during the study. | ||
*The study excluded patients with medication overuse headache as well as patients with myocardial infarction, stroke, transient ischemic attacks, unstable angina, coronary artery bypass surgery, or other revascularization procedures within 12 months prior to screening. | |||
===== | *The primary efficacy endpoint was the change from baseline in mean monthly migraine days over months 4 to 6. Secondary endpoints included the achievement of a ≥ 50% reduction from baseline in mean monthly migraine days over months 4 to 6 (“≥ 50% MMD responders”), the change from baseline in mean monthly acute migraine-specific medication days over months 4 to 6, and the change from baseline in mean Migraine Physical Function Impact Diary (MPFID) over months 4 to 6. The MPFID measures the impact of migraine on everyday activities (EA) and physical impairment (PI) using an electronic diary administered daily. Monthly MPFID scores are averaged over 28 days, including days with and without migraine; scores are scaled from 0 to 100. Higher scores indicate worse impact on EA and PI. Reductions from baseline in MPFID scores indicate improvement. | ||
*A total of 858 (90%) patients completed the 6-month double-blind study. Patients had a median age of 42 years (range: 18 to 65 years), 85% were female, and 89% were white. Three percent of patients were taking concomitant preventive treatments for migraine. The mean migraine frequency at baseline was approximately 8 migraine days per month and was similar across treatment groups. | |||
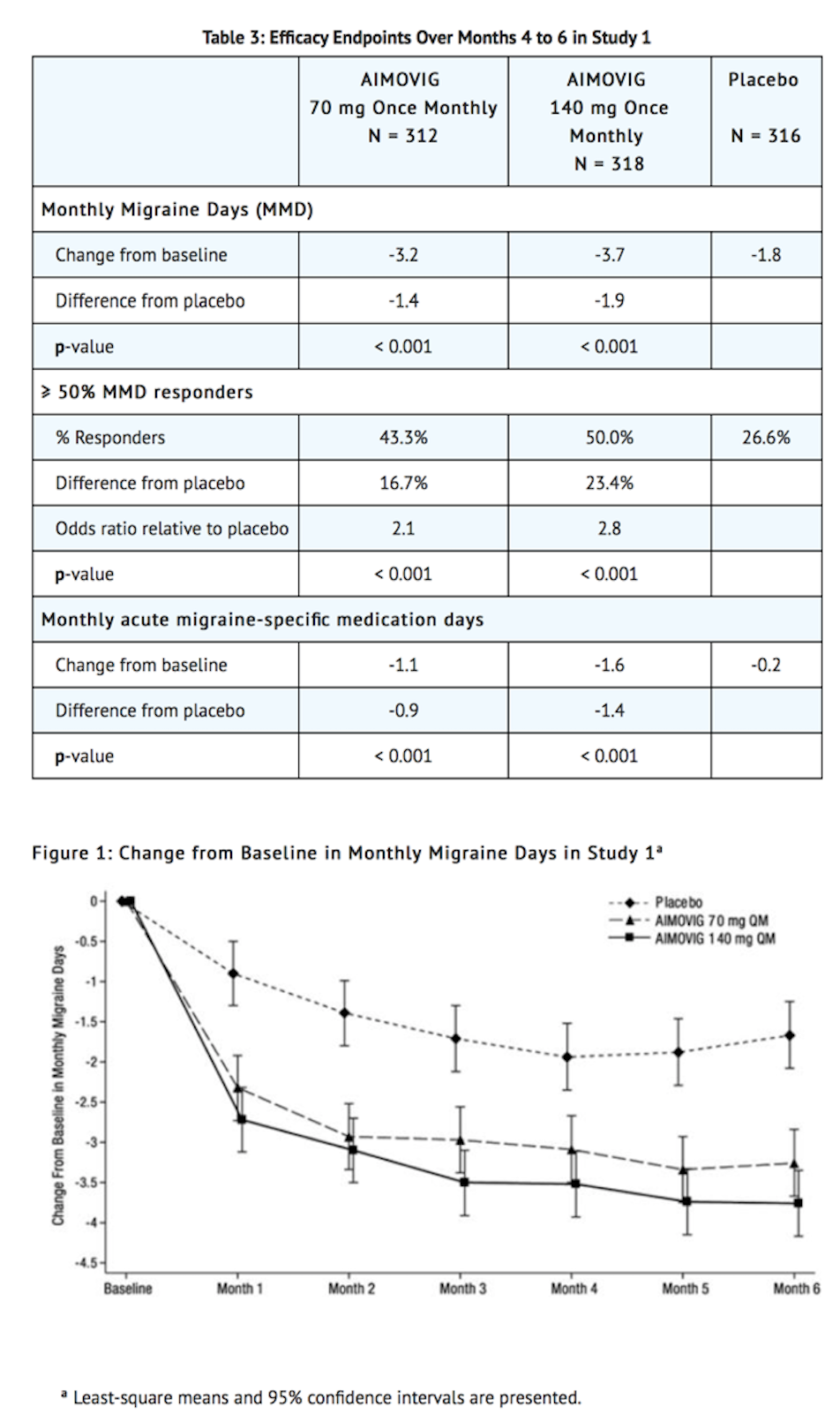
*AIMOVIG treatment demonstrated statistically significant improvements for key efficacy endpoints compared to placebo, as summarized in Table 3. | |||
[[image:Erenumab_Clinical_Studies_Table_1_and_Figure_1.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
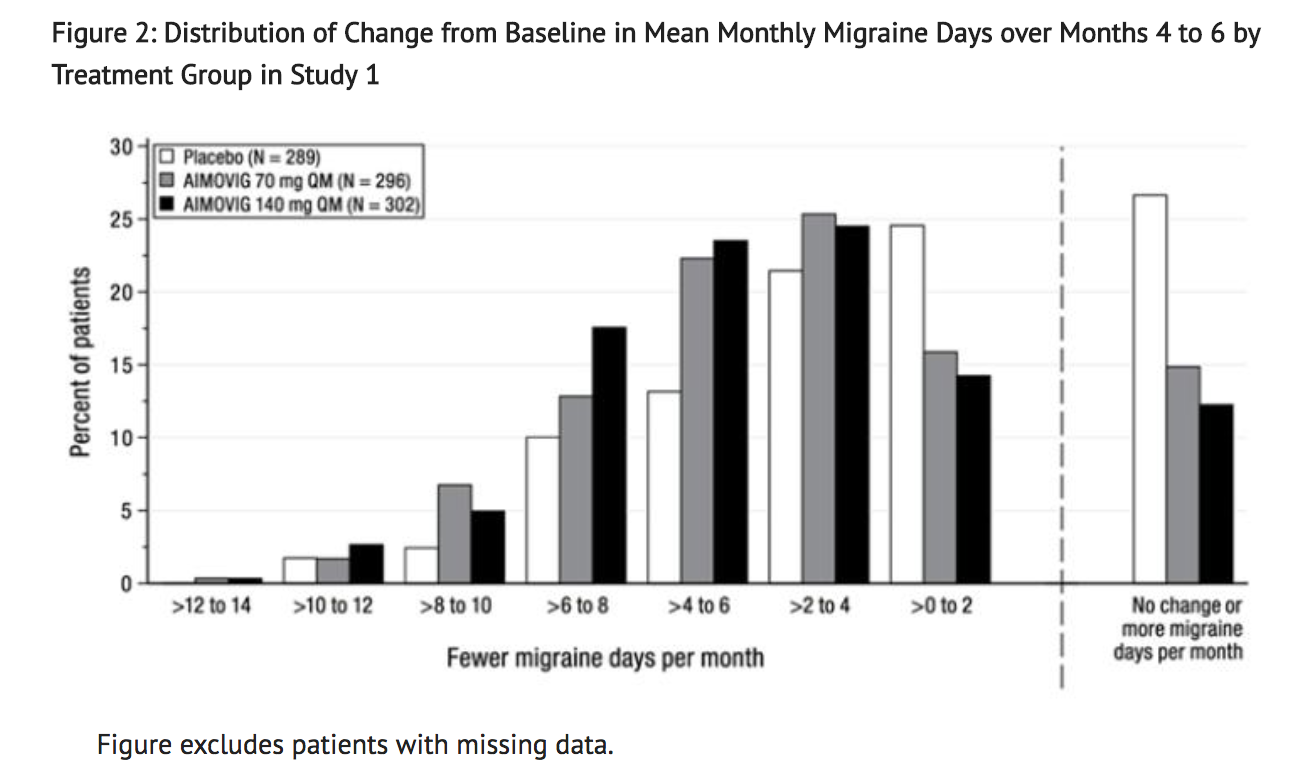
*Figure 2 shows the distribution of change from baseline in mean monthly migraine days over months 4 to 6 in bins of 2 days by treatment group. A treatment benefit over placebo for both doses of AIMOVIG is seen across a range of changes from baseline in monthly migraine days. | |||
[[image:Erenumab_Clinical_Studies_Figure_2.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
*Compared to placebo, patients treated with AIMOVIG 70 mg once monthly and 140 mg once monthly showed greater reductions from baseline in mean monthly MPFID everyday activity scores averaged over months 4 to 6 [difference from placebo: -2.2 for AIMOVIG 70 mg and -2.6 for AIMOVIG 140 mg; p-value < 0.001 for both], and in mean monthly MPFID physical impairment scores averaged over months 4 to 6 [difference from placebo: -1.9 for AIMOVIG 70 mg and -2.4 for AIMOVIG 140 mg; p-value < 0.001 for both]. | |||
*Study 2 (NCT 02483585) was a randomized, multi-center, 3-month, placebo-controlled, double-blind study evaluating AIMOVIG for the preventive treatment of episodic migraine. A total of 577 patients with a history of episodic migraine were randomized to receive either AIMOVIG 70 mg (N = 286) or placebo (N = 291) by subcutaneous injection once monthly for 3 months. Patients were allowed to use acute headache treatments including migraine-specific medications (i.e., triptans, ergotamine derivatives) and NSAIDs during the study. | |||
*The study excluded patients with medication overuse headache as well as patients with myocardial infarction, stroke, transient ischemic attacks, unstable angina, coronary artery bypass surgery, or other revascularization procedures within 12 months prior to screening. | |||
*The primary efficacy endpoint was the change from baseline in monthly migraine days at month 3. Secondary endpoints included the achievement of a ≥ 50% reduction from baseline in monthly migraine days (“≥ 50% MMD responders”), the change from baseline in monthly acute migraine-specific medication days at month 3, and the proportion of patients with at least a 5-point score reduction from baseline in MPFID at month 3. | |||
*A total of 546 (95%) patients completed the 3-month double-blind study. Patients had a median age of 43 years (range: 18 to 65 years), 85% were female, and 90% were white. Six to seven percent of patients were taking concomitant preventive migraine treatment. The mean migraine frequency at baseline was approximately 8 migraine days per month and was similar between treatment groups. | |||
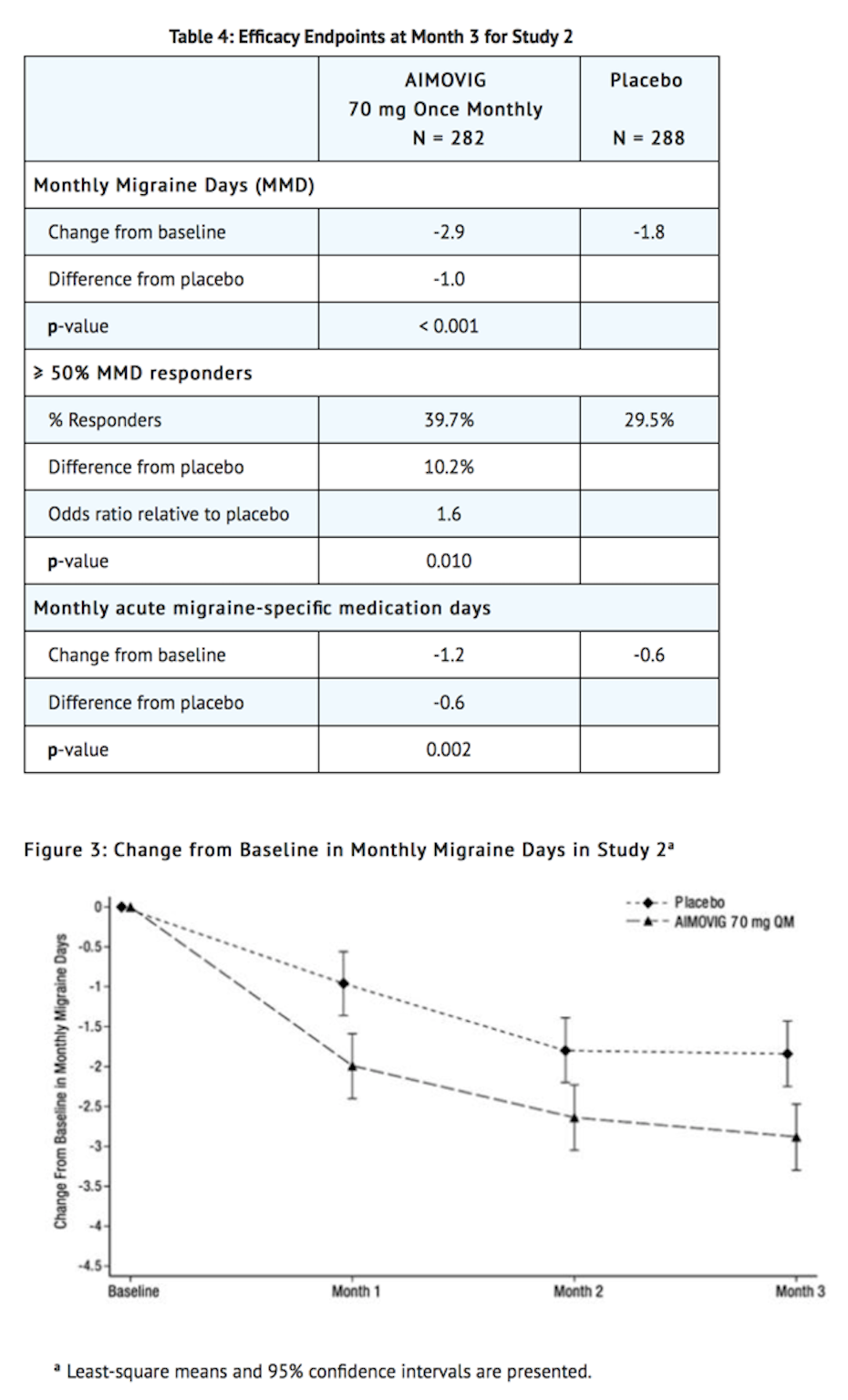
*AIMOVIG treatment demonstrated statistically significant improvements for key efficacy endpoints compared to placebo, as summarized in Table 4. | |||
[[image:Erelumab_Clinical_Studies_Table_2_and_Figure_3.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
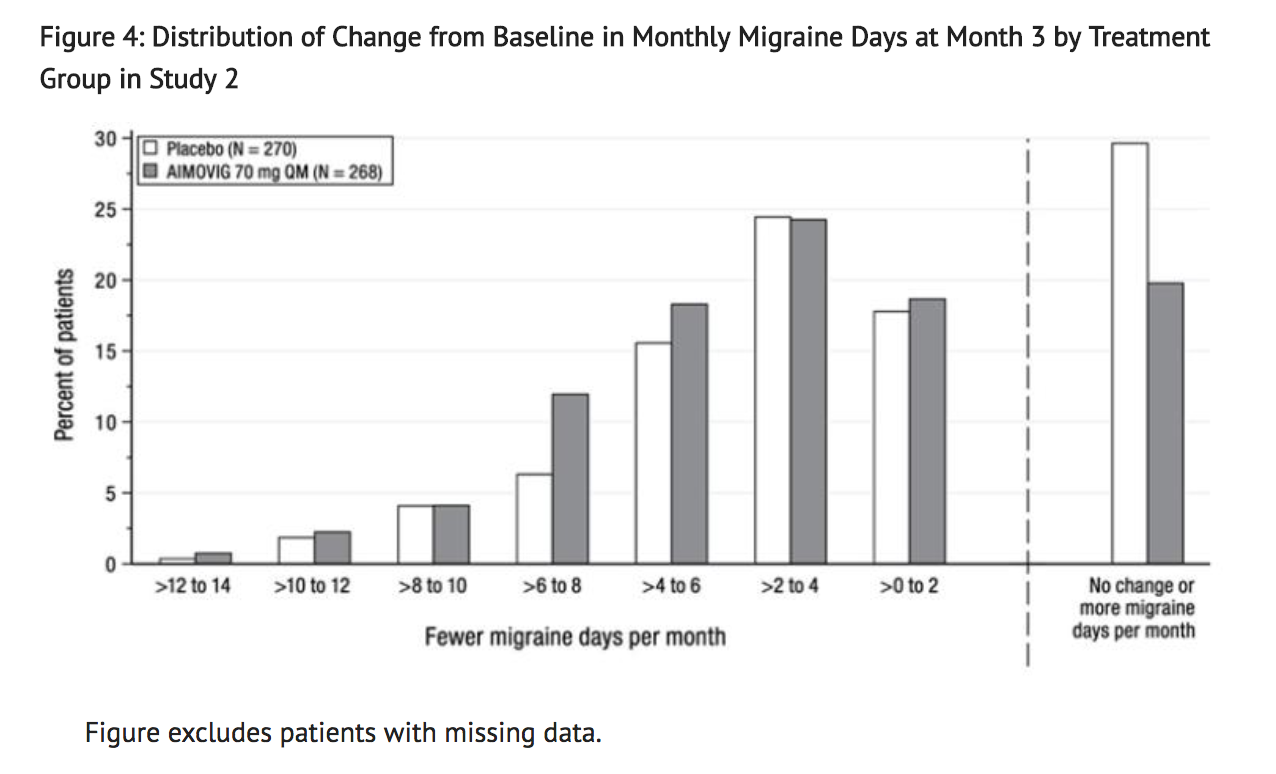
*Figure 4 shows the distribution of change from baseline in monthly migraine days at month 3 in bins of 2 days by treatment group. A treatment benefit over placebo for AIMOVIG is seen across a range of changes from baseline in monthly migraine days. | |||
[[image:Erelumab_Clinical_Studies_Figure_4.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
*The pre-specified analysis for the MPFID was based on at least a 5-point reduction within-patient responder definition. AIMOVIG 70 mg once monthly was not significantly better than placebo for the proportion of responders for everyday activity [difference from placebo: 4.7%; odds ratio = 1.2; p-value = 0.26] and physical impairment [difference from placebo: 5.9%; odds ratio = 1.3; p-value = 0.13]. In an exploratory analysis of the change from baseline in the mean MPFID scores at month 3, patients treated with AIMOVIG 70 mg, as compared to placebo, showed nominally greater reductions of physical impairment scores [difference from placebo: -1.3; p-value = 0.021], but not of everyday activities scores [difference from placebo: -1.1; p-value = 0.061]. | |||
Chronic Migraine | |||
*Study 3 (NCT 02066415) was a randomized, multi-center, 3-month, placebo-controlled, double-blind study evaluating AIMOVIG as a preventive treatment of chronic migraine. A total of 667 patients with a history of chronic migraine with or without aura were randomized to receive AIMOVIG 70 mg (N = 191), AIMOVIG 140 mg (N = 190), or placebo (N = 286) by subcutaneous injections once monthly for 3 months. Patients were allowed to use acute headache treatments including migraine-specific medications (i.e., triptans, ergotamine derivatives) and NSAIDs during the study. | |||
*The study excluded patients with medication overuse headache caused by opiate overuse and patients with concurrent use of migraine preventive treatments. Patients with myocardial infarction, stroke, transient ischemic attacks, unstable angina, coronary artery bypass surgery, or other revascularization procedures within 12 months prior to screening were also excluded. | |||
*The primary efficacy endpoint was the change from baseline in monthly migraine days at month 3. Secondary endpoints included the achievement of a ≥ 50% reduction from baseline in monthly migraine days (“≥ 50% MMD responders”) and change from baseline in monthly acute migraine-specific medication days at month 3. | |||
*A total of 631 (95%) patients completed the 3-month double-blind study. Patients had a median age of 43 years (range: 18 to 66 years), 83% were female, and 94% were white. The mean migraine frequency at baseline was approximately 18 migraine days per month and was similar across treatment groups. | |||
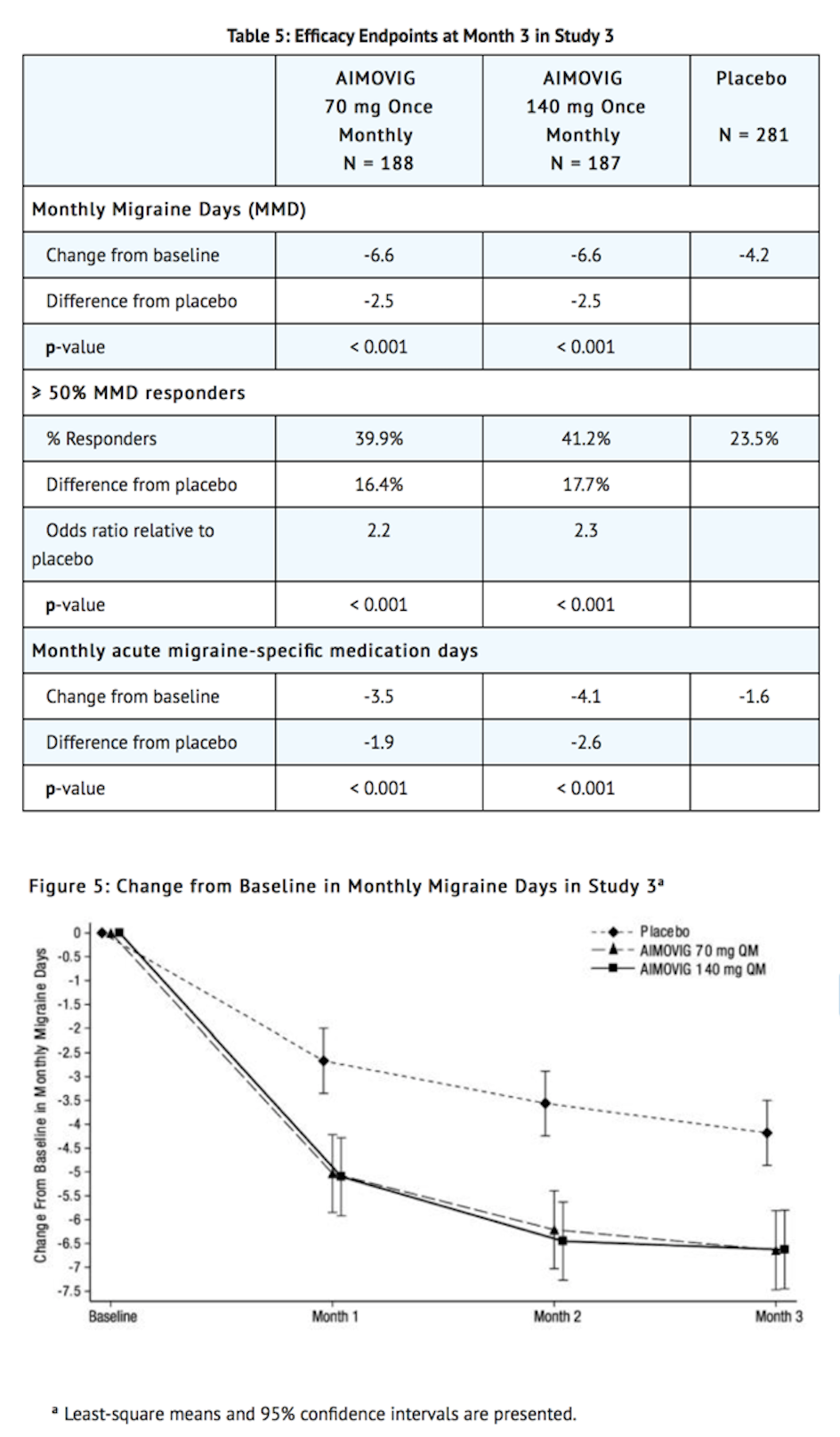
*AIMOVIG treatment demonstrated statistically significant improvements for key efficacy outcomes compared to placebo, as summarized in Table 5. | |||
[[image:Erenumab_Clinical_Studies_Table_3_and_Figure_5.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
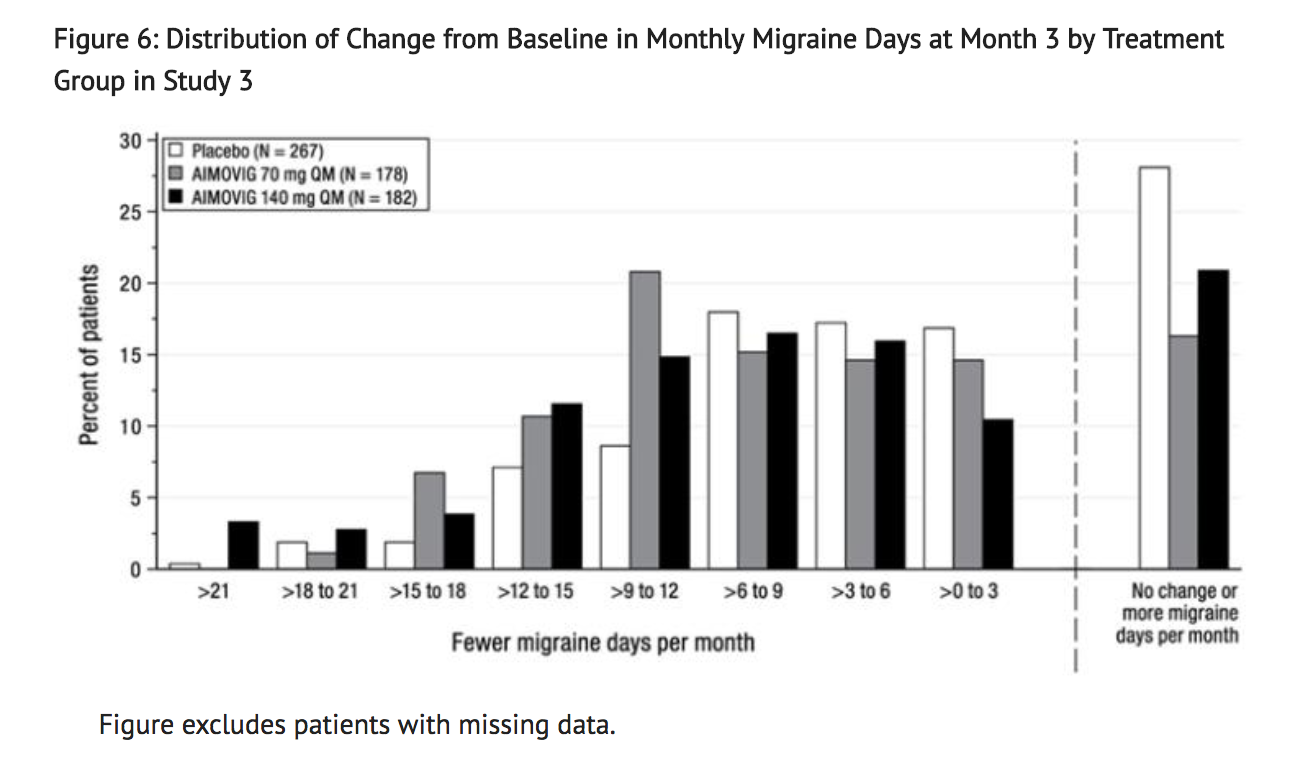
*Figure 6 shows the distribution of change from baseline in monthly migraine days at month 3 in bins of 3 days by treatment group. A treatment benefit over placebo for both doses of AIMOVIG is seen across a range of changes from baseline in migraine days. | |||
[[image:Erenumab_Clinical_Studies_Figure_6.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
|howSupplied=*AIMOVIG (erenumab-aooe) injection is a sterile, clear to opalescent, colorless to light yellow solution for subcutaneous administration. | |howSupplied=*AIMOVIG (erenumab-aooe) injection is a sterile, clear to opalescent, colorless to light yellow solution for subcutaneous administration. | ||
Revision as of 16:48, 16 July 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2];
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Warning Title
See full prescribing information for complete Boxed Warning.
Condition Name: (Content)
|
Overview
Erenumab is a Acetylcholine release inhibitor, Adrenergic receptor agonist that is FDA approved for the (type of indication of drug) of a list of indications, separated by commas.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include a list of adverse reactions, separated by commas..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Contraindications
CONTRAINDICATIONS
Warnings
|
Warning Title
See full prescribing information for complete Boxed Warning.
Condition Name: (Content)
|
Conidition 1
(Description)
Conidition 2
(Description)
Conidition 3
(Description)
Adverse Reactions
Clinical Trials Experience
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Condition 2
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Postmarketing Experience
(Description)
Drug Interactions
- Drug 1
- Drug 2
- Drug 3
- Drug 4
- Drug 5
Drug 1
(Description)
Drug 2
(Description)
Drug 3
(Description)
Drug 4
(Description)
Drug 5
(Description)
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
(Description)
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Erenumab in women who are pregnant.
Labor and Delivery
(Description)
Nursing Mothers
(Description)g
Pediatric Use
(Description)
Geriatic Use
(Description)
Gender
(Description)
Race
(Description)
Renal Impairment
(Description)
Hepatic Impairment
(Description)
Females of Reproductive Potential and Males
(Description)
Immunocompromised Patients
(Description)
Others
(Description)
Administration and Monitoring
Administration
(Oral/Intravenous/etc)
Monitoring
Condition 1
(Description regarding monitoring, from Warnings section)
Condition 2
(Description regarding monitoring, from Warnings section)
Condition 3
(Description regarding monitoring, from Warnings section)
IV Compatibility
There is limited information regarding the compatibility of Erenumab and IV administrations.
Overdosage
Acute Overdose
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description)
Pharmacology
Erenumab
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | ? |
| ATC code | ? |
| PubChem | ? |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
(Description)
Structure
(Description with picture)
Pharmacodynamics
(Description)
Pharmacokinetics
(Description)
Nonclinical Toxicology
(Description)
Clinical Studies
- The efficacy of AIMOVIG was evaluated as a preventive treatment of episodic or chronic migraine in three randomized, double-blind, placebo-controlled studies: two studies in patients with episodic migraine (4 to 14 migraine days per month) (Study 1 and Study 2) and one study in patients with chronic migraine (≥ 15 headache days per month with ≥ 8 migraine days per month) (Study 3). The studies enrolled patients with a history of migraine, with or without aura, according to the International Classification of Headache Disorders (ICHD-III) diagnostic criteria.
Episodic Migraine
- Study 1 (NCT 02456740) was a randomized, multi-center, 6-month, placebo-controlled, double-blind study evaluating AIMOVIG for the preventive treatment of episodic migraine. A total of 955 patients with a history of episodic migraine were randomized to receive either AIMOVIG 70 mg (N = 317), AIMOVIG 140 mg (N = 319), or placebo (N = 319) by subcutaneous injection once monthly (QM) for 6 months. Patients were allowed to use acute headache treatments including migraine-specific medications (i.e., triptans, ergotamine derivatives) and NSAIDs during the study.
- The study excluded patients with medication overuse headache as well as patients with myocardial infarction, stroke, transient ischemic attacks, unstable angina, coronary artery bypass surgery, or other revascularization procedures within 12 months prior to screening.
- The primary efficacy endpoint was the change from baseline in mean monthly migraine days over months 4 to 6. Secondary endpoints included the achievement of a ≥ 50% reduction from baseline in mean monthly migraine days over months 4 to 6 (“≥ 50% MMD responders”), the change from baseline in mean monthly acute migraine-specific medication days over months 4 to 6, and the change from baseline in mean Migraine Physical Function Impact Diary (MPFID) over months 4 to 6. The MPFID measures the impact of migraine on everyday activities (EA) and physical impairment (PI) using an electronic diary administered daily. Monthly MPFID scores are averaged over 28 days, including days with and without migraine; scores are scaled from 0 to 100. Higher scores indicate worse impact on EA and PI. Reductions from baseline in MPFID scores indicate improvement.
- A total of 858 (90%) patients completed the 6-month double-blind study. Patients had a median age of 42 years (range: 18 to 65 years), 85% were female, and 89% were white. Three percent of patients were taking concomitant preventive treatments for migraine. The mean migraine frequency at baseline was approximately 8 migraine days per month and was similar across treatment groups.
- AIMOVIG treatment demonstrated statistically significant improvements for key efficacy endpoints compared to placebo, as summarized in Table 3.
- Figure 2 shows the distribution of change from baseline in mean monthly migraine days over months 4 to 6 in bins of 2 days by treatment group. A treatment benefit over placebo for both doses of AIMOVIG is seen across a range of changes from baseline in monthly migraine days.
- Compared to placebo, patients treated with AIMOVIG 70 mg once monthly and 140 mg once monthly showed greater reductions from baseline in mean monthly MPFID everyday activity scores averaged over months 4 to 6 [difference from placebo: -2.2 for AIMOVIG 70 mg and -2.6 for AIMOVIG 140 mg; p-value < 0.001 for both], and in mean monthly MPFID physical impairment scores averaged over months 4 to 6 [difference from placebo: -1.9 for AIMOVIG 70 mg and -2.4 for AIMOVIG 140 mg; p-value < 0.001 for both].
- Study 2 (NCT 02483585) was a randomized, multi-center, 3-month, placebo-controlled, double-blind study evaluating AIMOVIG for the preventive treatment of episodic migraine. A total of 577 patients with a history of episodic migraine were randomized to receive either AIMOVIG 70 mg (N = 286) or placebo (N = 291) by subcutaneous injection once monthly for 3 months. Patients were allowed to use acute headache treatments including migraine-specific medications (i.e., triptans, ergotamine derivatives) and NSAIDs during the study.
- The study excluded patients with medication overuse headache as well as patients with myocardial infarction, stroke, transient ischemic attacks, unstable angina, coronary artery bypass surgery, or other revascularization procedures within 12 months prior to screening.
- The primary efficacy endpoint was the change from baseline in monthly migraine days at month 3. Secondary endpoints included the achievement of a ≥ 50% reduction from baseline in monthly migraine days (“≥ 50% MMD responders”), the change from baseline in monthly acute migraine-specific medication days at month 3, and the proportion of patients with at least a 5-point score reduction from baseline in MPFID at month 3.
- A total of 546 (95%) patients completed the 3-month double-blind study. Patients had a median age of 43 years (range: 18 to 65 years), 85% were female, and 90% were white. Six to seven percent of patients were taking concomitant preventive migraine treatment. The mean migraine frequency at baseline was approximately 8 migraine days per month and was similar between treatment groups.
- AIMOVIG treatment demonstrated statistically significant improvements for key efficacy endpoints compared to placebo, as summarized in Table 4.
- Figure 4 shows the distribution of change from baseline in monthly migraine days at month 3 in bins of 2 days by treatment group. A treatment benefit over placebo for AIMOVIG is seen across a range of changes from baseline in monthly migraine days.
- The pre-specified analysis for the MPFID was based on at least a 5-point reduction within-patient responder definition. AIMOVIG 70 mg once monthly was not significantly better than placebo for the proportion of responders for everyday activity [difference from placebo: 4.7%; odds ratio = 1.2; p-value = 0.26] and physical impairment [difference from placebo: 5.9%; odds ratio = 1.3; p-value = 0.13]. In an exploratory analysis of the change from baseline in the mean MPFID scores at month 3, patients treated with AIMOVIG 70 mg, as compared to placebo, showed nominally greater reductions of physical impairment scores [difference from placebo: -1.3; p-value = 0.021], but not of everyday activities scores [difference from placebo: -1.1; p-value = 0.061].
Chronic Migraine
- Study 3 (NCT 02066415) was a randomized, multi-center, 3-month, placebo-controlled, double-blind study evaluating AIMOVIG as a preventive treatment of chronic migraine. A total of 667 patients with a history of chronic migraine with or without aura were randomized to receive AIMOVIG 70 mg (N = 191), AIMOVIG 140 mg (N = 190), or placebo (N = 286) by subcutaneous injections once monthly for 3 months. Patients were allowed to use acute headache treatments including migraine-specific medications (i.e., triptans, ergotamine derivatives) and NSAIDs during the study.
- The study excluded patients with medication overuse headache caused by opiate overuse and patients with concurrent use of migraine preventive treatments. Patients with myocardial infarction, stroke, transient ischemic attacks, unstable angina, coronary artery bypass surgery, or other revascularization procedures within 12 months prior to screening were also excluded.
- The primary efficacy endpoint was the change from baseline in monthly migraine days at month 3. Secondary endpoints included the achievement of a ≥ 50% reduction from baseline in monthly migraine days (“≥ 50% MMD responders”) and change from baseline in monthly acute migraine-specific medication days at month 3.
- A total of 631 (95%) patients completed the 3-month double-blind study. Patients had a median age of 43 years (range: 18 to 66 years), 83% were female, and 94% were white. The mean migraine frequency at baseline was approximately 18 migraine days per month and was similar across treatment groups.
- AIMOVIG treatment demonstrated statistically significant improvements for key efficacy outcomes compared to placebo, as summarized in Table 5.
- Figure 6 shows the distribution of change from baseline in monthly migraine days at month 3 in bins of 3 days by treatment group. A treatment benefit over placebo for both doses of AIMOVIG is seen across a range of changes from baseline in migraine days.
How Supplied
- AIMOVIG (erenumab-aooe) injection is a sterile, clear to opalescent, colorless to light yellow solution for subcutaneous administration.
- The needle shield within the white cap of the AIMOVIG prefilled autoinjector and gray needle cap of the AIMOVIG prefilled syringe contain dry natural rubber (a derivative of latex). Each single-dose prefilled SureClick® autoinjector or single-dose prefilled syringe of AIMOVIG contains a Type 1 glass syringe and stainless steel needle and delivers 1 mL of 70 mg/mL solution.
- AIMOVIG is supplied as follows:
SureClick® Autoinjector
- Pack of 1 autoinjector: 70 mg/mL single-dose prefilled autoinjector NDC 55513-841-01.
- Pack of 2 autoinjectors: 140 mg/2 mL (2 x 70 mg/mL single-dose prefilled autoinjectors) NDC 55513-841-02
Syringe
- Pack of 1 syringe: 70 mg/mL single-dose prefilled syringe NDC 55513-840-01
- Pack of 2 syringes: 140 mg/2 mL (2 x 70 mg/mL single-dose prefilled syringes) NDC 55513-840-02
Storage
- Store refrigerated at 2°C to 8°C (36°F to 46°F) in the original carton to protect from light until time of use.
- If removed from the refrigerator, AIMOVIG should be kept at room temperature (up to 25°C [77°F]) in the original carton and must be used within 7 days. Throw away AIMOVIG that has been left at room temperature for more than 7 days.
- Do not freeze.
- Do not shake.
Images
Drug Images
{{#ask: Page Name::Erenumab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
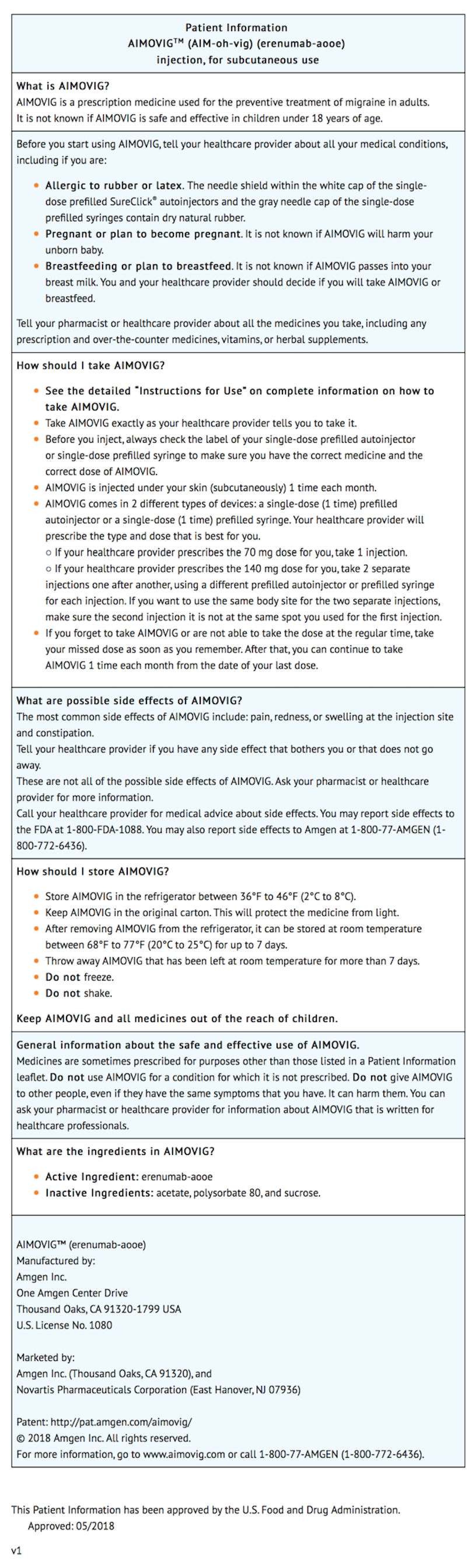
Package and Label Display Panel
{{#ask: Label Page::Erenumab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Information on Preparation and Administration:
- Provide guidance to patients and caregivers on proper subcutaneous administration technique, including aseptic technique, and how to use the single-dose prefilled autoinjector or single-dose prefilled syringe. Instruct patients and/or caregivers to read and follow the Instructions for Use each time they use AIMOVIG.
- Instruct patients prescribed 140 mg to administer the once monthly dosage as two separate subcutaneous injections of 70 mg each.
- Advise latex-sensitive patients that the needle shield within the white cap of the AIMOVIG prefilled autoinjector and gray needle cap of the AIMOVIG prefilled syringe contain dry natural rubber (a derivative of latex) that may cause allergic reactions in individuals sensitive to latex.
Precautions with Alcohol
Alcohol-Erenumab interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Aimovig
Look-Alike Drug Names
There is limited information regarding Erenumab Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.