Epidural abscess MRI: Difference between revisions
Joao Silva (talk | contribs) No edit summary |
m (Bot: Removing from Primary care) |
||
| (32 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Epidural abscess}} | {{Epidural abscess}} | ||
{{CMG}} | {{CMG}} {{AE}} {{JS}}; {{AG}} | ||
==Overview== | ==Overview== | ||
[[MRI]] may be helpful in the diagnosis of epidural abscess, as it is the preferred imaging study. Epidural abscess appearance varies depending on the location of the disease. On MRI, intracranial epidural abscess appears as a lentiform or crescent-shaped fluid collection. On T2-weighted images, epidural abscesses appear hyperintense compared to the [[cerebrospinal fluid]]. On T1-weighted images, epidural abscesses appear isointense or hypointense when compared to the [[brain]]. Following administration of [[gadolinium]] contrast, the [[dura mater]] is enhanced on T1-weighted images.<ref name=Harris>{{Cite book | last1 = Longo | first1 = Dan L. (Dan Louis) | title = Harrison's principles of internal medici | date = 2012 | publisher = McGraw-Hill | location = New York | isbn = 978-0-07-174889-6 | pages = }}</ref> On [[MRI]], spinal epidural abscess is characterized by low or intermediate intensity on T1-weighted MR sequences and high or intermediate intensity on T2-weighted images. | |||
==MRI== | ==MRI== | ||
[[MRI]] is the preferred imaging study in the diagnosis of epidural abscess. MRI is considered to be as effective as [[myelography]] in the diagnosis of epidural abscess, however MRI is superior, particularly in emergency situations, as it allows for visualization of the [[spinal cord]] in all planes without having to move the patient, who might have a neurological injury.<ref name="Grewal2006">{{cite journal|last1=Grewal|first1=S.|title=Epidural abscesses|journal=British Journal of Anaesthesia|volume=96|issue=3|year=2006|pages=292–302|issn=0007-0912|doi=10.1093/bja/ael006}}</ref> | |||
===Intracranial Epidural Abscess=== | |||
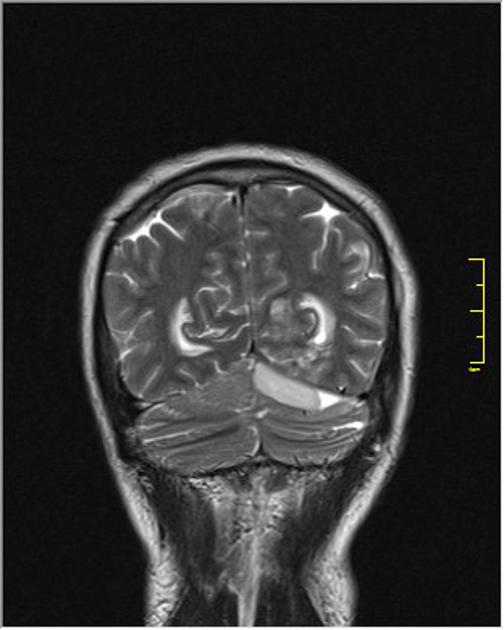
[[MRI]] is the preferred imaging method to investigate intracranial epidural abscess because it has higher accuracy defining intracranial lesions, compared to [[CT scan]]. On MRI, intracranial epidural abscess is characterized appears as a lentiform or crescent-shaped fluid collection. On T2-weighted images, epidural abscesses appear hyperintense compared to the [[cerebrospinal fluid]]. On T1-weighted images, epidural abscesses appear isointense or hypointense when compared to the [[brain]]. Following administration of gadolinium contrast, the dura mater is enhanced on T1-weighted images.<ref name=Harris>{{Cite book | last1 = Longo | first1 = Dan L. (Dan Louis) | title = Harrison's principles of internal medici | date = 2012 | publisher = McGraw-Hill | location = New York | isbn = 978-0-07-174889-6 | pages = }}</ref> | |||
[[Image:Intracranial epidural abscess.JPG|thumb|left|200px|thumb|Intracranial epidural abscess in the left [[infratentorial]] region<ref name=ICEAMRI> Image courtesy of Dr Bita Abbasi. [http://www.radiopaedia.org Radiopaedia] (original file [http://radiopaedia.org/cases/otomastoiditis-complicated-with-brain-abscess-and-epidural-empyema "here"]). [http://radiopaedia.org/licence Creative Commons BY-SA-NC]</ref>]] | |||
<br><br><br><br><br><br><br><br><br><br><br><br><br><br><br> | |||
===Spinal Epidural Abscess=== | |||
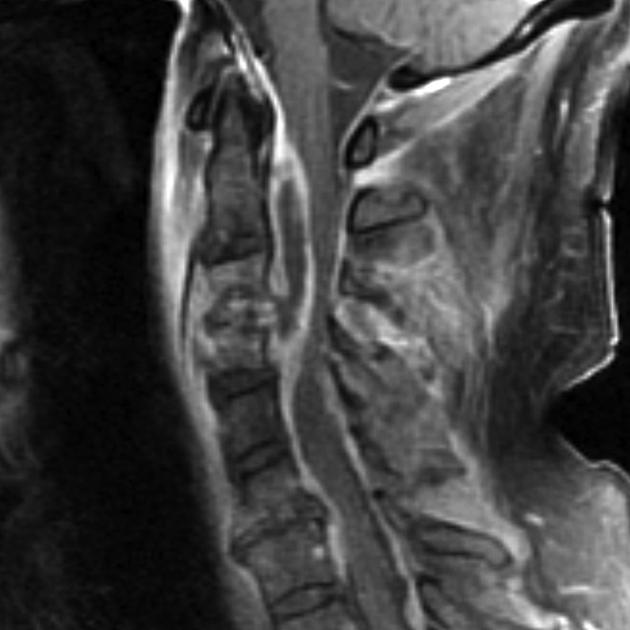
[[MRI]] with [[gadolinium]] [[contrast]] is the preferred method to aid in the [[diagnosis]] of spinal epidural abscess, as it distinguishes the longitudinal and paraspinal extensions of the abscess, allowing for an improved [[neurosurgery|neurosurgical]] approach. On [[MRI]], spinal epidural abscess is characterized by the following:<ref name="pmid7614792">{{cite journal |vauthors=Lang IM, Hughes DG, Jenkins JP, St Clair Forbes W, McKenna F |title=MR imaging appearances of cervical epidural abscess |journal=Clinical Radiology |volume=50 |issue=7 |pages=466–71 |year=1995 |pmid=7614792 |doi= |url=}}</ref><ref name="pmid11996416">{{cite journal |vauthors=Chao D, Nanda A |title=Spinal epidural abscess: a diagnostic challenge |journal=American Family Physician |volume=65 |issue=7 |pages=1341–6 |year=2002 |pmid=11996416 |doi= |url=}}</ref><ref name=SEARadio> Radiopaedia.org (2015) http://radiopaedia.org/articles/spinal-epidural-abscess Accessed on November 20, 2015</ref> | |||
*On T1-weighted MR sequences: | |||
**Low or intermediate intensity | |||
**Fluid portion of an abscess is usually hypointense | |||
**Liquid pus is associated with low signal intensity | |||
**Granulated tissue is enhanced following gadolinium injection | |||
*On T2-weighted images: | |||
**High or intermediate intensity | |||
**Fluid portion of an abscess is usually hyperintense | |||
Additionally, Gd-enhanced MR images can aid in the definition of the age and consistency of the abscess.<ref name="pmid7614792">{{cite journal |vauthors=Lang IM, Hughes DG, Jenkins JP, St Clair Forbes W, McKenna F |title=MR imaging appearances of cervical epidural abscess |journal=Clinical Radiology |volume=50 |issue=7 |pages=466–71 |year=1995 |pmid=7614792 |doi= |url=}}</ref><ref name="pmid11996416">{{cite journal |vauthors=Chao D, Nanda A |title=Spinal epidural abscess: a diagnostic challenge |journal=American Family Physician |volume=65 |issue=7 |pages=1341–6 |year=2002 |pmid=11996416 |doi= |url=}}</ref> It is also helpful in differentiating an abscess from [[malignancy]].<ref name="Grewal2006">{{cite journal|last1=Grewal|first1=S.|title=Epidural abscesses|journal=British Journal of Anaesthesia|volume=96|issue=3|year=2006|pages=292–302|issn=0007-0912|doi=10.1093/bja/ael006}}</ref><ref name="Darouiche2006">{{cite journal|last1=Darouiche|first1=Rabih O.|title=Spinal Epidural Abscess|journal=New England Journal of Medicine|volume=355|issue=19|year=2006|pages=2012–2020|issn=0028-4793|doi=10.1056/NEJMra055111}}</ref> Spinal epidural abscess is frequently associated with evidence of spinal cord compression on MR imaging.<ref name="pmid8079871">{{cite journal |vauthors=Friedmand DP, Hills JR |title=Cervical epidural spinal infection: MR imaging characteristics |journal=AJR. American Journal of Roentgenology |volume=163 |issue=3 |pages=699–704 |year=1994 |pmid=8079871 |doi=10.2214/ajr.163.3.8079871 |url=}}</ref> More information regarding the appearance of spinal epidural abscess can be found [http://eradiology.bidmc.harvard.edu/LearningLab/central/Tukey.pdf here]. | |||
[[Image:Spinal epidural abscess(MRI).jpg|thumb|left|200px|thumb|Spinal Epidural Abscess accompanied by C3/C4 level [[discitis]]/[[osteomyelitis]]<ref name=SEAMRI> Image courtesy of Dr Frank Gaillard. [http://www.radiopaedia.org Radiopaedia] (original file [http://radiopaedia.org/cases/epidural-abscess-of-the-cervical-spine "here"]). [http://radiopaedia.org/licence Creative Commons BY-SA-NC]</ref>]] | |||
<br><br><br><br><br><br><br><br><br><br><br><br><br> | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Neurology]] | [[Category:Neurology]] | ||
Latest revision as of 21:36, 29 July 2020
|
Epidural abscess Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Epidural abscess MRI On the Web |
|
American Roentgen Ray Society Images of Epidural abscess MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [2]; Anthony Gallo, B.S. [3]
Overview
MRI may be helpful in the diagnosis of epidural abscess, as it is the preferred imaging study. Epidural abscess appearance varies depending on the location of the disease. On MRI, intracranial epidural abscess appears as a lentiform or crescent-shaped fluid collection. On T2-weighted images, epidural abscesses appear hyperintense compared to the cerebrospinal fluid. On T1-weighted images, epidural abscesses appear isointense or hypointense when compared to the brain. Following administration of gadolinium contrast, the dura mater is enhanced on T1-weighted images.[1] On MRI, spinal epidural abscess is characterized by low or intermediate intensity on T1-weighted MR sequences and high or intermediate intensity on T2-weighted images.
MRI
MRI is the preferred imaging study in the diagnosis of epidural abscess. MRI is considered to be as effective as myelography in the diagnosis of epidural abscess, however MRI is superior, particularly in emergency situations, as it allows for visualization of the spinal cord in all planes without having to move the patient, who might have a neurological injury.[2]
Intracranial Epidural Abscess
MRI is the preferred imaging method to investigate intracranial epidural abscess because it has higher accuracy defining intracranial lesions, compared to CT scan. On MRI, intracranial epidural abscess is characterized appears as a lentiform or crescent-shaped fluid collection. On T2-weighted images, epidural abscesses appear hyperintense compared to the cerebrospinal fluid. On T1-weighted images, epidural abscesses appear isointense or hypointense when compared to the brain. Following administration of gadolinium contrast, the dura mater is enhanced on T1-weighted images.[1]
Spinal Epidural Abscess
MRI with gadolinium contrast is the preferred method to aid in the diagnosis of spinal epidural abscess, as it distinguishes the longitudinal and paraspinal extensions of the abscess, allowing for an improved neurosurgical approach. On MRI, spinal epidural abscess is characterized by the following:[4][5][6]
- On T1-weighted MR sequences:
- Low or intermediate intensity
- Fluid portion of an abscess is usually hypointense
- Liquid pus is associated with low signal intensity
- Granulated tissue is enhanced following gadolinium injection
- On T2-weighted images:
- High or intermediate intensity
- Fluid portion of an abscess is usually hyperintense
Additionally, Gd-enhanced MR images can aid in the definition of the age and consistency of the abscess.[4][5] It is also helpful in differentiating an abscess from malignancy.[2][7] Spinal epidural abscess is frequently associated with evidence of spinal cord compression on MR imaging.[8] More information regarding the appearance of spinal epidural abscess can be found here.
References
- ↑ 1.0 1.1 Longo, Dan L. (Dan Louis) (2012). Harrison's principles of internal medici. New York: McGraw-Hill. ISBN 978-0-07-174889-6.
- ↑ 2.0 2.1 Grewal, S. (2006). "Epidural abscesses". British Journal of Anaesthesia. 96 (3): 292–302. doi:10.1093/bja/ael006. ISSN 0007-0912.
- ↑ Image courtesy of Dr Bita Abbasi. Radiopaedia (original file "here"). Creative Commons BY-SA-NC
- ↑ 4.0 4.1 Lang IM, Hughes DG, Jenkins JP, St Clair Forbes W, McKenna F (1995). "MR imaging appearances of cervical epidural abscess". Clinical Radiology. 50 (7): 466–71. PMID 7614792.
- ↑ 5.0 5.1 Chao D, Nanda A (2002). "Spinal epidural abscess: a diagnostic challenge". American Family Physician. 65 (7): 1341–6. PMID 11996416.
- ↑ Radiopaedia.org (2015) http://radiopaedia.org/articles/spinal-epidural-abscess Accessed on November 20, 2015
- ↑ Darouiche, Rabih O. (2006). "Spinal Epidural Abscess". New England Journal of Medicine. 355 (19): 2012–2020. doi:10.1056/NEJMra055111. ISSN 0028-4793.
- ↑ Friedmand DP, Hills JR (1994). "Cervical epidural spinal infection: MR imaging characteristics". AJR. American Journal of Roentgenology. 163 (3): 699–704. doi:10.2214/ajr.163.3.8079871. PMID 8079871.
- ↑ Image courtesy of Dr Frank Gaillard. Radiopaedia (original file "here"). Creative Commons BY-SA-NC