Entecavir
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: SEVERE ACUTE EXACERBATIONS OF HEPATITIS B, PATIENTS CO-INFECTED WITH HIV AND HBV, and LACTIC ACIDOSIS AND HEPATOMEGALY
See full prescribing information for complete Boxed Warning.
|
Overview
Entecavir is a reverse transcriptase inhibitor that is FDA approved for the {{{indicationType}}} of chronic hepatitis B virus infection in adults and children at least 2 years of age. There is a Black Box Warning for this drug as shown here. Common adverse reactions include headache, fatigue, dizziness, and nausea.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Chronic Hepatitis B Virus
- Dosing Information
- Compensated Liver Disease
- The recommended dose of BARACLUDE for chronic hepatitis B virus infection in nucleoside-inhibitor-treatment-naïve adults and adolescents 16 years of age and older is 0.5 mg once daily.
- The recommended dose of BARACLUDE in adults and adolescents (at least 16 years of age) with a history of hepatitis B viremia while receiving lamivudine or known lamivudine or telbivudine resistance substitutions rtM204I/V with or without rtL180M, rtL80I/V, or rtV173L is 1 mg once daily.
- Compensated Liver Disease
- Decompensated Liver Disease
- The recommended dose of BARACLUDE for chronic hepatitis B virus infection in adults with decompensated liver disease is 1 mg once daily.
- Decompensated Liver Disease
- Renal Impairment
- In adult subjects with renal impairment, the apparent oral clearance of entecavir decreased as creatinine clearance decreased. Dosage adjustment is recommended for patients with creatinine clearance less than 50 mL/min, including patients on hemodialysis or continuous ambulatory peritoneal dialysis (CAPD), as shown in Table 2. The once-daily dosing regimens are preferred.
- Renal Impairment
- Duration of Therapy
- The optimal duration of treatment with BARACLUDE for patients with chronic hepatitis B virus infection and the relationship between treatment and long-term outcomes such as cirrhosis and hepatocellular carcinoma are unknown.
- Duration of Therapy
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Entecavir in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Entecavir in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Chronic Hepatitis B Virus
- Dosing Information
- Table 1 describes the recommended dose of BARACLUDE for pediatric patients 2 years of age or older and weighing at least 10 kg. The oral solution should be used for patients with body weight up to 30 kg.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Entecavir in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Entecavir in pediatric patients.
Contraindications
- None.
Warnings
|
WARNING: SEVERE ACUTE EXACERBATIONS OF HEPATITIS B, PATIENTS CO-INFECTED WITH HIV AND HBV, and LACTIC ACIDOSIS AND HEPATOMEGALY
See full prescribing information for complete Boxed Warning.
|
Precautions
- Severe Acute Exacerbations of Hepatitis B
- Severe acute exacerbations of hepatitis B have been reported in patients who have discontinued anti-hepatitis B therapy, including entecavir. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who discontinue anti-hepatitis B therapy. If appropriate, initiation of anti-hepatitis B therapy may be warranted.
- Patients Co-infected with HIV and HBV
- BARACLUDE has not been evaluated in HIV/HBV co-infected patients who were not simultaneously receiving effective HIV treatment. Limited clinical experience suggests there is a potential for the development of resistance to HIV nucleoside reverse transcriptase inhibitors if BARACLUDE is used to treat chronic hepatitis B virus infection in patients with HIV infection that is not being treated. Therefore, therapy with BARACLUDE is not recommended for HIV/HBV co-infected patients who are not also receiving HAART. Before initiating BARACLUDE therapy, HIV antibody testing should be offered to all patients. BARACLUDE has not been studied as a treatment for HIV infection and is not recommended for this use.
- Lactic Acidosis and Severe Hepatomegaly with Steatosis
- Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogue inhibitors, including BARACLUDE, alone or in combination with antiretrovirals. A majority of these cases have been in women. Obesity and prolonged nucleoside inhibitor exposure may be risk factors. Particular caution should be exercised when administering nucleoside analogue inhibitors to any patient with known risk factors for liver disease; however, cases have also been reported in patients with no known risk factors.
- Lactic acidosis with BARACLUDE use has been reported, often in association with hepatic decompensation, other serious medical conditions, or drug exposures. Patients with decompensated liver disease may be at higher risk for lactic acidosis. Treatment with BARACLUDE should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations).
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- Compensated Liver Disease
- Assessment of adverse reactions is based on four studies (AI463014, AI463022, AI463026, and AI463027) in which 1720 subjects with chronic hepatitis B virus infection and compensated liver disease received double-blind treatment with BARACLUDE 0.5 mg/day (n=679), BARACLUDE 1 mg/day (n=183), or lamivudine (n=858) for up to 2 years. Median duration of therapy was 69 weeks for BARACLUDE-treated subjects and 63 weeks for lamivudine-treated subjects in Studies AI463022 and AI463027 and 73 weeks for BARACLUDE-treated subjects and 51 weeks for lamivudine-treated subjects in Studies AI463026 and AI463014. The safety profiles of BARACLUDE and lamivudine were comparable in these studies.
- The most common adverse reactions of any severity (≥3%) with at least a possible relation to study drug for BARACLUDE-treated subjects were headache, fatigue, dizziness, and nausea. The most common adverse reactions among lamivudine-treated subjects were headache, fatigue, and dizziness. One percent of BARACLUDE-treated subjects in these four studies compared with 4% of lamivudine-treated subjects discontinued for adverse events or abnormal laboratory test results.
- Clinical adverse reactions of moderate-severe intensity and considered at least possibly related to treatment occurring during therapy in four clinical studies in which BARACLUDE was compared with lamivudine are presented in Table 3.
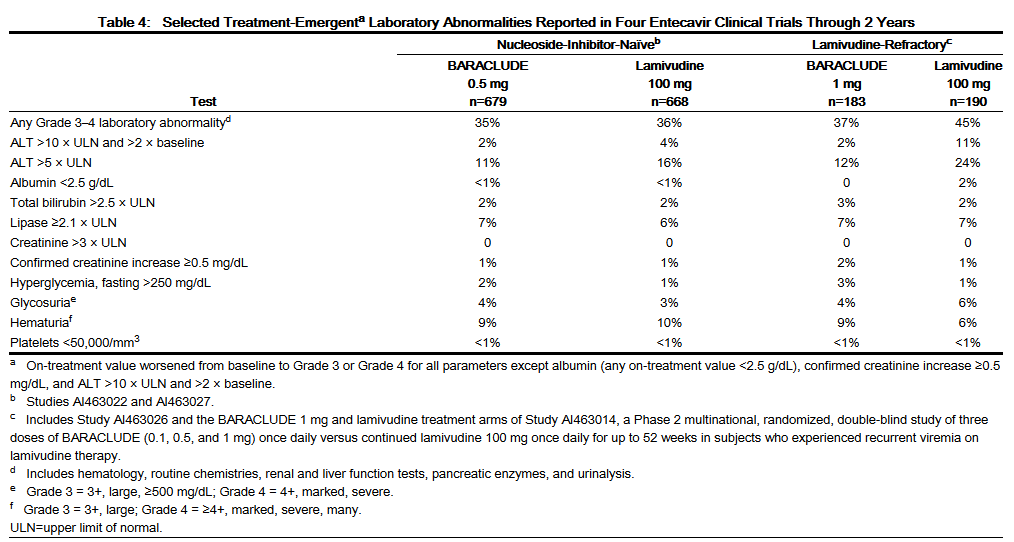
- Laboratory Abnormalities
- Frequencies of selected treatment-emergent laboratory abnormalities reported during therapy in four clinical trials of BARACLUDE compared with lamivudine are listed in Table 4.
- Among BARACLUDE-treated subjects in these studies, on-treatment ALT elevations greater than 10 times the upper limit of normal (ULN) and greater than 2 times baseline generally resolved with continued treatment. A majority of these exacerbations were associated with a ≥2 log10/mL reduction in viral load that preceded or coincided with the ALT elevation. Periodic monitoring of hepatic function is recommended during treatment.
- Exacerbations of Hepatitis after Discontinuation of Treatment
- An exacerbation of hepatitis or ALT flare was defined as ALT greater than 10 times ULN and greater than 2 times the subject’s reference level (minimum of the baseline or last measurement at end of dosing). For all subjects who discontinued treatment (regardless of reason), Table 5 presents the proportion of subjects in each study who experienced post-treatment ALT flares. In these studies, a subset of subjects was allowed to discontinue treatment at or after 52 weeks if they achieved a protocol-defined response to therapy. If BARACLUDE is discontinued without regard to treatment response, the rate of post-treatment flares could be higher.
- Decompensated Liver Disease
- Study AI463048 was a randomized, open-label study of BARACLUDE 1 mg once daily versus adefovir dipivoxil 10 mg once daily given for up to 48 weeks in adult subjects with chronic HBV infection and evidence of hepatic decompensation, defined as a Child-Turcotte-Pugh (CTP) score of 7 or higher. Among the 102 subjects receiving BARACLUDE, the most common treatment-emergent adverse events of any severity, regardless of causality, occurring through Week 48 were peripheral edema (16%), ascites (15%), pyrexia (14%), hepatic encephalopathy (10%), and upper respiratory infection (10%). Clinical adverse reactions not listed in Table 3 that were observed through Week 48 include blood bicarbonate decreased (2%) and renal failure (<1%).
- Eighteen of 102 (18%) subjects treated with BARACLUDE and 18/89 (20%) subjects treated with adefovir dipivoxil died during the first 48 weeks of therapy. The majority of deaths (11 in the BARACLUDE group and 16 in the adefovir dipivoxil group) were due to liver-related causes such as hepatic failure, hepatic encephalopathy, hepatorenal syndrome, and upper gastrointestinal hemorrhage. The rate of hepatocellular carcinoma (HCC) through Week 48 was 6% (6/102) for subjects treated with BARACLUDE and 8% (7/89) for subjects treated with adefovir dipivoxil. Five percent of subjects in either treatment arm discontinued therapy due to an adverse event through Week 48.
- No subject in either treatment arm experienced an on-treatment hepatic flare (ALT >2 × baseline and >10 × ULN) through Week 48. Eleven of 102 (11%) subjects treated with BARACLUDE and 11/89 (13%) subjects treated with adefovir dipivoxil had a confirmed increase in serum creatinine of 0.5 mg/dL through Week 48.
- HIV/HBV Co-infected
- The safety profile of BARACLUDE 1 mg (n=51) in HIV/HBV co-infected subjects enrolled in Study AI463038 was similar to that of placebo (n=17) through 24 weeks of blinded treatment and similar to that seen in non-HIV infected subjects.
- Liver Transplant Recipients
- Among 65 subjects receiving BARACLUDE in an open-label, post-liver transplant trial, the frequency and nature of adverse events were consistent with those expected in patients who have received a liver transplant and the known safety profile of BARACLUDE.
- Clinical Trial Experience in Pediatric Subjects
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The safety of BARACLUDE in pediatric subjects 2 to less than 18 years of age is based on two ongoing clinical trials in subjects with chronic HBV infection (one Phase 2 pharmacokinetic trial [AI463028] and one Phase 3 trial [AI463189]). These trials provide experience in 168 HBeAg-positive subjects treated with BARACLUDE for a median duration of 72 weeks. The adverse reactions observed in pediatric subjects who received treatment with BARACLUDE were consistent with those observed in clinical trials of BARACLUDE in adults. Adverse drug reactions reported in greater than 1% of pediatric subjects included abdominal pain, rash events, poor palatability (“product taste abnormal”), nausea, diarrhea, and vomiting.
Postmarketing Experience
- The following adverse reactions have been reported during postmarketing use of BARACLUDE. Because these reactions were reported voluntarily from a population of unknown size, it is not possible to reliably estimate their frequency or establish a causal relationship to BARACLUDE exposure.
- Immune system disorders: Anaphylactoid reaction.
- Metabolism and nutrition disorders: Lactic acidosis.
- Hepatobiliary disorders: Increased transaminases.
Drug Interactions
- Since entecavir is primarily eliminated by the kidneys, coadministration of BARACLUDE with drugs that reduce renal function or compete for active tubular secretion may increase serum concentrations of either entecavir or the coadministered drug. Coadministration of entecavir with lamivudine, adefovir dipivoxil, or tenofovir disoproxil fumarate did not result in significant drug interactions. The effects of coadministration of BARACLUDE with other drugs that are renally eliminated or are known to affect renal function have not been evaluated, and patients should be monitored closely for adverse events when BARACLUDE is coadministered with such drugs.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- There are no adequate and well-controlled studies of BARACLUDE in pregnant women. Because animal reproduction studies are not always predictive of human response, BARACLUDE should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Antiretroviral Pregnancy Registry: To monitor fetal outcomes of pregnant women exposed to BARACLUDE, an Antiretroviral Pregnancy Registry has been established. Healthcare providers are encouraged to register patients by calling 1-800-258-4263.
- Animal Data
- Animal reproduction studies with entecavir in rats and rabbits revealed no evidence of teratogenicity. Developmental toxicity studies were performed in rats and rabbits. There were no signs of embryofetal or maternal toxicity when pregnant animals received oral entecavir at approximately 28 (rat) and 212 (rabbit) times the human exposure achieved at the highest recommended human dose of 1 mg/day. In rats, maternal toxicity, embryofetal toxicity (resorptions), lower fetal body weights, tail and vertebral malformations, reduced ossification (vertebrae, sternebrae, and phalanges), and extra lumbar vertebrae and ribs were observed at exposures 3100 times those in humans. In rabbits, embryofetal toxicity (resorptions), reduced ossification (hyoid), and an increased incidence of 13th rib were observed at exposures 883 times those in humans. In a peri-postnatal study, no adverse effects on offspring occurred when rats received oral entecavir at exposures greater than 94 times those in humans.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Entecavir in women who are pregnant.
Labor and Delivery
- There are no studies in pregnant women and no data on the effect of BARACLUDE on transmission of HBV from mother to infant. Therefore, appropriate interventions should be used to prevent neonatal acquisition of HBV.
Nursing Mothers
- It is not known whether BARACLUDE is excreted into human milk; however, entecavir is excreted into the milk of rats. Because many drugs are excreted into human milk and because of the potential for serious adverse reactions in nursing infants from BARACLUDE, a decision should be made to discontinue nursing or to discontinue BARACLUDE taking into consideration the importance of continued hepatitis B therapy to the mother and the known benefits of breastfeeding.
Pediatric Use
- BARACLUDE was evaluated in two clinical trials of pediatric subjects 2 years of age and older with HBeAg-positive chronic HBV infection and compensated liver disease. The exposure of BARACLUDE in nucleoside-inhibitor-treatment-naïve and lamivudine-experienced pediatric subjects 2 years of age and older with HBeAg-positive chronic HBV infection and compensated liver disease receiving 0.015 mg/kg (up to 0.5 mg once daily) or 0.03 mg/kg (up to 1 mg once daily), respectively, was evaluated in Study AI463028. Safety and efficacy of the selected dose in treatment-naïve pediatric subjects were confirmed in Study AI463189, a randomized, placebo-controlled treatment trial.
- There are limited data available on the use of BARACLUDE in lamivudine-experienced pediatric patients; BARACLUDE should be used in these patients only if the potential benefit justifies the potential risk to the child. Since some pediatric patients may require long-term or even lifetime management of chronic active hepatitis B, consideration should be given to the impact of BARACLUDE on future treatment options.
- The efficacy and safety of BARACLUDE have not been established in patients less than 2 years of age. Use of BARACLUDE in this age group has not been evaluated because treatment of HBV in this age group is rarely required.
Geriatic Use
- Clinical studies of BARACLUDE did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects. Entecavir is substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Gender
There is no FDA guidance on the use of Entecavir with respect to specific gender populations.
Race
- There are no significant racial differences in entecavir pharmacokinetics. The safety and efficacy of BARACLUDE 0.5 mg once daily were assessed in a single-arm, open-label trial of HBeAg-positive or -negative, nucleoside-inhibitor-naïve, Black/African American (n=40) and Hispanic (n=6) subjects with chronic HBV infection. In this trial, 76% of subjects were male, the mean age was 42 years, 57% were HBeAg-positive, the mean baseline HBV DNA was 7.0 log10 IU/mL, and the mean baseline ALT was 162 U/L. At Week 48 of treatment, 32 of 46 (70%) subjects had HBV DNA <50 IU/mL (approximately 300 copies/mL), 31 of 46 (67%) subjects had ALT normalization (≤1 × ULN), and 12 of 26 (46%) HBeAg-positive subjects had HBe seroconversion. Safety data were similar to those observed in the larger controlled clinical trials.
Renal Impairment
- Dosage adjustment of BARACLUDE is recommended for patients with creatinine clearance less than 50 mL/min, including patients on hemodialysis or CAPD.
Hepatic Impairment
There is no FDA guidance on the use of Entecavir in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Entecavir in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Entecavir in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Entecavir in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Entecavir in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- There is limited experience of entecavir overdosage reported in patients. Healthy subjects who received single entecavir doses up to 40 mg or multiple doses up to 20 mg/day for up to 14 days had no increase in or unexpected adverse events.
Management
- If overdose occurs, the patient must be monitored for evidence of toxicity, and standard supportive treatment applied as necessary.
- Following a single 1 mg dose of entecavir, a 4-hour hemodialysis session removed approximately 13% of the entecavir dose.
Chronic Overdose
There is limited information regarding Chronic Overdose of Entecavir in the drug label.
Pharmacology
Mechanism of Action
- Entecavir, a guanosine nucleoside analogue with activity against HBV reverse transcriptase (rt), is efficiently phosphorylated to the active triphosphate form, which has an intracellular half-life of 15 hours. By competing with the natural substrate deoxyguanosine triphosphate, entecavir triphosphate functionally inhibits all three activities of the HBV reverse transcriptase: (1) base priming, (2) reverse transcription of the negative strand from the pregenomic messenger RNA, and (3) synthesis of the positive strand of HBV DNA. Entecavir triphosphate is a weak inhibitor of cellular DNA polymerases α, β, and δ and mitochondrial DNA polymerase γ with Ki values ranging from 18 to >160 μM.
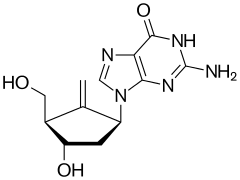
Structure
- BARACLUDE® is the tradename for entecavir, a guanosine nucleoside analogue with selective activity against HBV. The chemical name for entecavir is 2-amino-1,9-dihydro-9-[(1S,3R,4S)-4-hydroxy-3-(hydroxymethyl)-2-methylenecyclopentyl]-6H-purin-6-one, monohydrate. Its molecular formula is C12H15N5O3∙H2O, which corresponds to a molecular weight of 295.3. Entecavir has the following structural formula:
- Entecavir is a white to off-white powder. It is slightly soluble in water (2.4 mg/mL), and the pH of the saturated solution in water is 7.9 at 25° C ± 0.5° C.
- BARACLUDE film-coated tablets are available for oral administration in strengths of 0.5 mg and 1 mg of entecavir. BARACLUDE 0.5 mg and 1 mg film-coated tablets contain the following inactive ingredients: lactose monohydrate, microcrystalline cellulose, crospovidone, povidone, and magnesium stearate. The tablet coating contains titanium dioxide, hypromellose, polyethylene glycol 400, polysorbate 80 (0.5 mg tablet only), and iron oxide red (1 mg tablet only). BARACLUDE Oral Solution is available for oral administration as a ready-to-use solution containing 0.05 mg of entecavir per milliliter. BARACLUDE Oral Solution contains the following inactive ingredients: maltitol, sodium citrate, citric acid, methylparaben, propylparaben, and orange flavor.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Entecavir in the drug label.
Pharmacokinetics
- The single- and multiple-dose pharmacokinetics of entecavir were evaluated in healthy subjects and subjects with chronic hepatitis B virus infection.
- Absorption
- Following oral administration in healthy subjects, entecavir peak plasma concentrations occurred between 0.5 and 1.5 hours. Following multiple daily doses ranging from 0.1 to 1 mg, Cmax and area under the concentration-time curve (AUC) at steady state increased in proportion to dose. Steady state was achieved after 6 to 10 days of once-daily administration with approximately 2-fold accumulation. For a 0.5 mg oral dose, Cmax at steady state was 4.2 ng/mL and trough plasma concentration (Ctrough) was 0.3 ng/mL. For a 1 mg oral dose, Cmax was 8.2 ng/mL and Ctrough was 0.5 ng/mL.
- In healthy subjects, the bioavailability of the tablet was 100% relative to the oral solution. The oral solution and tablet may be used interchangeably.
- Effects of food on oral absorption: Oral administration of 0.5 mg of entecavir with a standard high-fat meal (945 kcal, 54.6 g fat) or a light meal (379 kcal, 8.2 g fat) resulted in a delay in absorption (1.0–1.5 hours fed vs. 0.75 hours fasted), a decrease in Cmax of 44%–46%, and a decrease in AUC of 18%–20%.
- Distribution
- Based on the pharmacokinetic profile of entecavir after oral dosing, the estimated apparent volume of distribution is in excess of total body water, suggesting that entecavir is extensively distributed into tissues.
- Binding of entecavir to human serum proteins in vitro was approximately 13%.
- Metabolism and Elimination
- Following administration of 14C-entecavir in humans and rats, no oxidative or acetylated metabolites were observed. Minor amounts of phase II metabolites (glucuronide and sulfate conjugates) were observed. Entecavir is not a substrate, inhibitor, or inducer of the cytochrome P450 (CYP450) enzyme system.
- After reaching peak concentration, entecavir plasma concentrations decreased in a bi-exponential manner with a terminal elimination half-life of approximately 128–149 hours. The observed drug accumulation index is approximately 2-fold with once-daily dosing, suggesting an effective accumulation half-life of approximately 24 hours.
- Entecavir is predominantly eliminated by the kidney with urinary recovery of unchanged drug at steady state ranging from 62% to 73% of the administered dose. Renal clearance is independent of dose and ranges from 360 to 471 mL/min suggesting that entecavir undergoes both glomerular filtration and net tubular secretion.
- Special Populations
- Gender: There are no significant gender differences in entecavir pharmacokinetics.
- Race: There are no significant racial differences in entecavir pharmacokinetics.
- Elderly: The effect of age on the pharmacokinetics of entecavir was evaluated following administration of a single 1 mg oral dose in healthy young and elderly volunteers. Entecavir AUC was 29.3% greater in elderly subjects compared to young subjects. The disparity in exposure between elderly and young subjects was most likely attributable to differences in renal function. Dosage adjustment of BARACLUDE should be based on the renal function of the patient, rather than age.
- Pediatrics: The steady-state pharmacokinetics of entecavir were evaluated in nucleoside-inhibitor-naïve and lamivudine-experienced HBeAg-positive pediatric subjects 2 to less than 18 years of age with compensated liver disease. Results are shown in Table 6. Entecavir exposure among nucleoside-inhibitor-naïve subjects was similar to the exposure achieved in adults receiving once-daily doses of 0.5 mg. Entecavir exposure among lamivudine-experienced subjects was similar to the exposure achieved in adults receiving once-daily doses of 1 mg.
- Renal impairment: The pharmacokinetics of entecavir following a single 1 mg dose were studied in subjects (without chronic hepatitis B virus infection) with selected degrees of renal impairment, including subjects whose renal impairment was managed by hemodialysis or continuous ambulatory peritoneal dialysis (CAPD). Results are shown in Table 7.
- Following a single 1 mg dose of entecavir administered 2 hours before the hemodialysis session, hemodialysis removed approximately 13% of the entecavir dose over 4 hours. CAPD removed approximately 0.3% of the dose over 7 days.
- Hepatic impairment: The pharmacokinetics of entecavir following a single 1 mg dose were studied in adult subjects (without chronic hepatitis B virus infection) with moderate or severe hepatic impairment (Child-Turcotte-Pugh Class B or C). The pharmacokinetics of entecavir were similar between hepatically impaired and healthy control subjects; therefore, no dosage adjustment of BARACLUDE is recommended for patients with hepatic impairment. The pharmacokinetics of entecavir have not been studied in pediatric subjects with hepatic impairment.
- Post-liver transplant: Limited data are available on the safety and efficacy of BARACLUDE in liver transplant recipients. In a small pilot study of entecavir use in HBV-infected liver transplant recipients on a stable dose of cyclosporine A (n=5) or tacrolimus (n=4), entecavir exposure was approximately 2-fold the exposure in healthy subjects with normal renal function. Altered renal function contributed to the increase in entecavir exposure in these subjects. The potential for pharmacokinetic interactions between entecavir and cyclosporine A or tacrolimus was not formally evaluated.
- Drug Interactions
- The metabolism of entecavir was evaluated in in vitro and in vivo studies. Entecavir is not a substrate, inhibitor, or inducer of the cytochrome P450 (CYP450) enzyme system. At concentrations up to approximately 10,000-fold higher than those obtained in humans, entecavir inhibited none of the major human CYP450 enzymes 1A2, 2C9, 2C19, 2D6, 3A4, 2B6, and 2E1. At concentrations up to approximately 340-fold higher than those observed in humans, entecavir did not induce the human CYP450 enzymes 1A2, 2C9, 2C19, 3A4, 3A5, and 2B6. The pharmacokinetics of entecavir are unlikely to be affected by coadministration with agents that are either metabolized by, inhibit, or induce the CYP450 system. Likewise, the pharmacokinetics of known CYP substrates are unlikely to be affected by coadministration of entecavir.
- The steady-state pharmacokinetics of entecavir and coadministered drug were not altered in interaction studies of entecavir with lamivudine, adefovir dipivoxil, and tenofovir disoproxil fumarate.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenesis
- Long-term oral carcinogenicity studies of entecavir in mice and rats were carried out at exposures up to approximately 42 times (mice) and 35 times (rats) those observed in humans at the highest recommended dose of 1 mg/day. In mouse and rat studies, entecavir was positive for carcinogenic findings.
- In mice, lung adenomas were increased in males and females at exposures 3 and 40 times those in humans. Lung carcinomas in both male and female mice were increased at exposures 40 times those in humans. Combined lung adenomas and carcinomas were increased in male mice at exposures 3 times and in female mice at exposures 40 times those in humans. Tumor development was preceded by pneumocyte proliferation in the lung, which was not observed in rats, dogs, or monkeys administered entecavir, supporting the conclusion that lung tumors in mice may be a species-specific event. Hepatocellular carcinomas were increased in males and combined liver adenomas and carcinomas were also increased at exposures 42 times those in humans. Vascular tumors in female mice (hemangiomas of ovaries and uterus and hemangiosarcomas of spleen) were increased at exposures 40 times those in humans. In rats, hepatocellular adenomas were increased in females at exposures 24 times those in humans; combined adenomas and carcinomas were also increased in females at exposures 24 times those in humans. Brain gliomas were induced in both males and females at exposures 35 and 24 times those in humans. Skin fibromas were induced in females at exposures 4 times those in humans.
- It is not known how predictive the results of rodent carcinogenicity studies may be for humans.
- Mutagenesis
- Entecavir was clastogenic to human lymphocyte cultures. Entecavir was not mutagenic in the Ames bacterial reverse mutation assay using S. typhimurium and E. coli strains in the presence or absence of metabolic activation, a mammalian-cell gene mutation assay, and a transformation assay with Syrian hamster embryo cells. Entecavir was also negative in an oral micronucleus study and an oral DNA repair study in rats.
- Impairment of Fertility
- In reproductive toxicology studies, in which animals were administered entecavir at up to 30 mg/kg for up to 4 weeks, no evidence of impaired fertility was seen in male or female rats at systemic exposures greater than 90 times those achieved in humans at the highest recommended dose of 1 mg/day. In rodent and dog toxicology studies, seminiferous tubular degeneration was observed at exposures 35 times or greater than those achieved in humans. No testicular changes were evident in monkeys.
Clinical Studies
Outcomes in Adults
- At 48 Weeks
- The safety and efficacy of BARACLUDE in adults were evaluated in three Phase 3 active-controlled trials. These studies included 1633 subjects 16 years of age or older with chronic hepatitis B virus infection (serum HBsAg-positive for at least 6 months) accompanied by evidence of viral replication (detectable serum HBV DNA, as measured by the bDNA hybridization or PCR assay). Subjects had persistently elevated ALT levels at least 1.3 times ULN and chronic inflammation on liver biopsy compatible with a diagnosis of chronic viral hepatitis. The safety and efficacy of BARACLUDE were also evaluated in a study of 191 HBV-infected subjects with decompensated liver disease and in a study of 68 subjects co-infected with HBV and HIV.
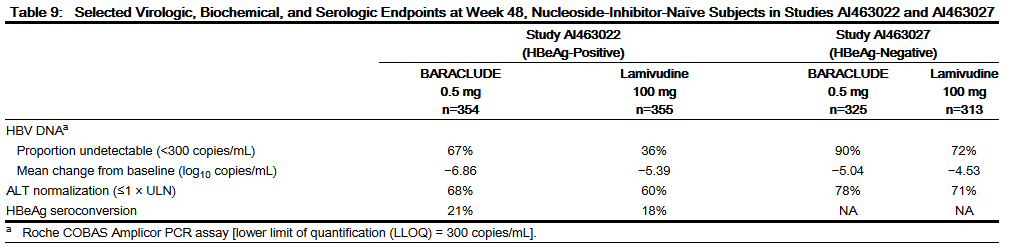
- Nucleoside-inhibitor-naïve Subjects with Compensated Liver Disease
- HBeAg-positive: Study AI463022 was a multinational, randomized, double-blind study of BARACLUDE 0.5 mg once daily versus lamivudine 100 mg once daily for a minimum of 52 weeks in 709 (of 715 randomized) nucleoside-inhibitor-naïve subjects with chronic hepatitis B virus infection, compensated liver disease, and detectable HBeAg. The mean age of subjects was 35 years, 75% were male, 57% were Asian, 40% were Caucasian, and 13% had previously received interferon-α. At baseline, subjects had a mean Knodell Necroinflammatory Score of 7.8, mean serum HBV DNA as measured by Roche COBAS Amplicor® PCR assay was 9.66 log10 copies/mL, and mean serum ALT level was 143 U/L. Paired, adequate liver biopsy samples were available for 89% of subjects.
- HBeAg-negative (anti-HBe-positive/HBV DNA-positive): Study AI463027 was a multinational, randomized, double-blind study of BARACLUDE 0.5 mg once daily versus lamivudine 100 mg once daily for a minimum of 52 weeks in 638 (of 648 randomized) nucleoside-inhibitor-naïve subjects with HBeAg-negative (HBeAb-positive) chronic hepatitis B virus infection and compensated liver disease. The mean age of subjects was 44 years, 76% were male, 39% were Asian, 58% were Caucasian, and 13% had previously received interferon-α. At baseline, subjects had a mean Knodell Necroinflammatory Score of 7.8, mean serum HBV DNA as measured by Roche COBAS Amplicor PCR assay was 7.58 log10 copies/mL, and mean serum ALT level was 142 U/L. Paired, adequate liver biopsy samples were available for 88% of subjects.
- In Studies AI463022 and AI463027, BARACLUDE was superior to lamivudine on the primary efficacy endpoint of Histologic Improvement, defined as a 2-point or greater reduction in Knodell Necroinflammatory Score with no worsening in Knodell Fibrosis Score at Week 48, and on the secondary efficacy measures of reduction in viral load and ALT normalization. Histologic Improvement and change in Ishak Fibrosis Score are shown in Table 8. Selected virologic, biochemical, and serologic outcome measures are shown in Table 9.
- Histologic Improvement was independent of baseline levels of HBV DNA or ALT.
- Lamivudine-refractory Subjects with Compensated Liver Disease
- Study AI463026 was a multinational, randomized, double-blind study of BARACLUDE in 286 (of 293 randomized) subjects with lamivudine-refractory chronic hepatitis B virus infection and compensated liver disease. Subjects receiving lamivudine at study entry either switched to BARACLUDE 1 mg once daily (with neither a washout nor an overlap period) or continued on lamivudine 100 mg for a minimum of 52 weeks. The mean age of subjects was 39 years, 76% were male, 37% were Asian, 62% were Caucasian, and 52% had previously received interferon-α. The mean duration of prior lamivudine therapy was 2.7 years, and 85% had lamivudine resistance substitutions at baseline by an investigational line probe assay. At baseline, subjects had a mean Knodell Necroinflammatory Score of 6.5, mean serum HBV DNA as measured by Roche COBAS Amplicor PCR assay was 9.36 log10 copies/mL, and mean serum ALT level was 128 U/L. Paired, adequate liver biopsy samples were available for 87% of subjects.
- BARACLUDE was superior to lamivudine on a primary endpoint of Histologic Improvement (using the Knodell Score at Week 48). These results and change in Ishak Fibrosis Score are shown in Table 10. Table 11 shows selected virologic, biochemical, and serologic endpoints.
- Histologic Improvement was independent of baseline levels of HBV DNA or ALT.
- Subjects with Decompensated Liver Disease
- Study AI463048 was a randomized, open-label study of BARACLUDE 1 mg once daily versus adefovir dipivoxil 10 mg once daily in 191 (of 195 randomized) adult subjects with HBeAg-positive or -negative chronic HBV infection and evidence of hepatic decompensation, defined as a Child-Turcotte-Pugh (CTP) score of 7 or higher. Subjects were either HBV-treatment-naïve or previously treated, predominantly with lamivudine or interferon-α.
- In Study AI463048, 100 subjects were randomized to treatment with BARACLUDE and 91 subjects to treatment with adefovir dipivoxil. Two subjects randomized to treatment with adefovir dipivoxil actually received treatment with BARACLUDE for the duration of the study. The mean age of subjects was 52 years, 74% were male, 54% were Asian, 33% were Caucasian, and 5% were Black/African American. At baseline, subjects had a mean serum HBV DNA by PCR of 7.83 log10 copies/mL and mean ALT level of 100 U/L; 54% of subjects were HBeAg-positive; 35% had genotypic evidence of lamivudine resistance. The baseline mean CTP score was 8.6. Results for selected study endpoints at Week 48 are shown in Table 12.
- Subjects Co-infected with HIV and HBV
- Study AI463038 was a randomized, double-blind, placebo-controlled study of BARACLUDE versus placebo in 68 subjects co-infected with HIV and HBV who experienced recurrence of HBV viremia while receiving a lamivudine-containing highly active antiretroviral (HAART) regimen. Subjects continued their lamivudine-containing HAART regimen (lamivudine dose 300 mg/day) and were assigned to add either BARACLUDE 1 mg once daily (51 subjects) or placebo (17 subjects) for 24 weeks followed by an open-label phase for an additional 24 weeks where all subjects received BARACLUDE. At baseline, subjects had a mean serum HBV DNA level by PCR of 9.13 log10 copies/mL. Ninety-nine percent of subjects were HBeAg-positive at baseline, with a mean baseline ALT level of 71.5 U/L. Median HIV RNA level remained stable at approximately 2 log10 copies/mL through 24 weeks of blinded therapy. Virologic and biochemical endpoints at Week 24 are shown in Table 13. There are no data in patients with HIV/HBV co-infection who have not received prior lamivudine therapy. BARACLUDE has not been evaluated in HIV/HBV co-infected patients who were not simultaneously receiving effective HIV treatment.
- For subjects originally assigned to BARACLUDE, at the end of the open-label phase (Week 48), 8% of subjects had HBV DNA <300 copies/mL by PCR, the mean change from baseline HBV DNA by PCR was −4.20 log10 copies/mL, and 37% of subjects with abnormal ALT at baseline had ALT normalization (≤1 × ULN).
- Beyond 48 Weeks
- The optimal duration of therapy with BARACLUDE is unknown. According to protocol-mandated criteria in the Phase 3 clinical trials, subjects discontinued BARACLUDE or lamivudine treatment after 52 weeks according to a definition of response based on HBV virologic suppression (<0.7 MEq/mL by bDNA assay) and loss of HBeAg (in HBeAg-positive subjects) or ALT <1.25 × ULN (in HBeAg-negative subjects) at Week 48. Subjects who achieved virologic suppression but did not have serologic response (HBeAg-positive) or did not achieve ALT <1.25 × ULN (HBeAg-negative) continued blinded dosing through 96 weeks or until the response criteria were met. These protocol-specified subject management guidelines are not intended as guidance for clinical practice.
- Nucleoside-inhibitor-naïve Subjects
- Among nucleoside-inhibitor-naïve, HBeAg-positive subjects (Study AI463022), 243 (69%) BARACLUDE-treated subjects and 164 (46%) lamivudine-treated subjects continued blinded treatment for up to 96 weeks. Of those continuing blinded treatment in Year 2, 180 (74%) BARACLUDE subjects and 60 (37%) lamivudine subjects achieved HBV DNA <300 copies/mL by PCR at the end of dosing (up to 96 weeks). 193 (79%) BARACLUDE subjects achieved ALT ≤1 × ULN compared to 112 (68%) lamivudine subjects, and HBeAg seroconversion occurred in 26 (11%) BARACLUDE subjects and 20 (12%) lamivudine subjects.
- Among nucleoside-inhibitor-naïve, HBeAg-positive subjects, 74 (21%) BARACLUDE subjects and 67 (19%) lamivudine subjects met the definition of response at Week 48, discontinued study drugs, and were followed off treatment for 24 weeks. Among BARACLUDE responders, 26 (35%) subjects had HBV DNA <300 copies/mL, 55 (74%) subjects had ALT ≤1 × ULN, and 56 (76%) subjects sustained HBeAg seroconversion at the end of follow-up. Among lamivudine responders, 20 (30%) subjects had HBV DNA <300 copies/mL, 41 (61%) subjects had ALT ≤1 × ULN, and 47 (70%) subjects sustained HBeAg seroconversion at the end of follow-up.
- Among nucleoside-inhibitor-naïve, HBeAg-negative subjects (Study AI463027), 26 (8%) BARACLUDE-treated subjects and 28 (9%) lamivudine-treated subjects continued blinded treatment for up to 96 weeks. In this small cohort continuing treatment in Year 2, 22 BARACLUDE and 16 lamivudine subjects had HBV DNA <300 copies/mL by PCR, and 7 and 6 subjects, respectively, had ALT ≤1 × ULN at the end of dosing (up to 96 weeks).
- Among nucleoside-inhibitor-naïve, HBeAg-negative subjects, 275 (85%) BARACLUDE subjects and 245 (78%) lamivudine subjects met the definition of response at Week 48, discontinued study drugs, and were followed off treatment for 24 weeks. In this cohort, very few subjects in each treatment arm had HBV DNA <300 copies/mL by PCR at the end of follow-up. At the end of follow-up, 126 (46%) BARACLUDE subjects and 84 (34%) lamivudine subjects had ALT ≤1 × ULN.
- Lamivudine-refractory Subjects
- Among lamivudine-refractory subjects (Study AI463026), 77 (55%) BARACLUDE-treated subjects and 3 (2%) lamivudine subjects continued blinded treatment for up to 96 weeks. In this cohort of BARACLUDE subjects, 31 (40%) subjects achieved HBV DNA <300 copies/mL, 62 (81%) subjects had ALT ≤1 × ULN, and 8 (10%) subjects demonstrated HBeAg seroconversion at the end of dosing.
Outcomes in Pediatric Subjects
- The pharmacokinetics, safety and antiviral activity of BARACLUDE in pediatric subjects were initially assessed in Study AI463028. Twenty-four treatment-naïve and 19 lamivudine-experienced HBeAg-positive pediatric subjects 2 to less than 18 years of age with compensated CHB and elevated ALT were treated with BARACLUDE 0.015 mg/kg (up to 0.5 mg) or 0.03 mg/kg (up to 1 mg) once daily. Fifty-eight percent (14/24) of treatment-naïve subjects and 47% (9/19) of lamivudine-experienced subjects achieved HBV DNA <50 IU/mL at Week 48 and ALT normalized in 83% (20/24) of treatment-naïve and 95% (18/19) of lamivudine-experienced subjects.
- Safety and antiviral efficacy were confirmed in Study AI463189, an ongoing study of BARACLUDE among 180 nucleoside-inhibitor-treatment-naïve pediatric subjects 2 to less than 18 years of age with HBeAg-positive chronic hepatitis B infection, compensated liver disease, and elevated ALT. Subjects were randomized 2:1 to receive blinded treatment with BARACLUDE 0.015 mg/kg up to 0.5 mg/day (N=120) or placebo (N=60). The randomization was stratified by age group (2 to 6 years; >6 to 12 years; and >12 to <18 years). Baseline demographics and HBV disease characteristics were comparable between the 2 treatment arms and across age cohorts. At study entry, the mean HBV DNA was 8.1 log10 IU/mL and mean ALT was 103 U/L. The primary efficacy endpoint was a composite of HBeAg seroconversion and serum HBV DNA <50 IU/mL at Week 48 assessed in the first 123 subjects reaching 48 weeks of blinded treatment. Twenty-four percent (20/82) of subjects in the BARACLUDE-treated group and 2% (1/41) of subjects in the placebo-treated group met the primary endpoint. Forty-six percent (38/82) of BARACLUDE-treated subjects and 2% (1/41) of placebo-treated subjects achieved HBV DNA <50 IU/mL at Week 48. ALT normalization occurred in 67% (55/82) of BARACLUDE-treated subjects and 22% (9/41) of placebo-treated subjects; 24% (20/82) of BARACLUDE-treated subjects and 12% (5/41) of placebo-treated subjects had HBeAg seroconversion.
How Supplied
- BARACLUDE® (entecavir) Tablets and Oral Solution are available in the following strengths and configurations of plastic bottles with child-resistant closures:
- BARACLUDE Oral Solution is a ready-to-use product; dilution or mixing with water or any other solvent or liquid product is not recommended. Each bottle of the oral solution is accompanied by a dosing spoon that is calibrated in 0.5 mL increments up to 10 mL.
- Storage
- BARACLUDE Tablets should be stored in a tightly closed container at 25°C (77°F); excursions permitted between 15°C and 30°C (59° and 86°F). Store in the outer carton to protect from light.
- BARACLUDE Oral Solution should be stored in the outer carton at 25°C (77°F); excursions permitted between 15°C and 30°C (59° and 86°F). Protect from light. After opening, the oral solution can be used up to the expiration date on the bottle. The bottle and its contents should be discarded after the expiration date.
Storage
There is limited information regarding Entecavir Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Entecavir |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Entecavir |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Information about Treatment
- Physicians should inform their patients of the following important points when initiating BARACLUDE treatment:
- Patients should remain under the care of a physician while taking BARACLUDE. They should discuss any new symptoms or concurrent medications with their physician.
- Patients should be advised that treatment with BARACLUDE has not been shown to reduce the risk of transmission of HBV to others through sexual contact or blood contamination.
- Patients should be advised to take BARACLUDE on an empty stomach (at least 2 hours after a meal and 2 hours before the next meal).
- Patients using the oral solution should be instructed to hold the dosing spoon in a vertical position and fill it gradually to the mark corresponding to the prescribed dose. Rinsing of the dosing spoon with water is recommended after each daily dose. Some patients may find it difficult to accurately measure the prescribed dose using the provided dosing spoon; therefore, patients/caregivers should refer to the steps in the Patient Information section that demonstrate the correct technique of using the provided dosing spoon to measure the prescribed BARACLUDE dose.
- Patients should be advised to take a missed dose as soon as remembered unless it is almost time for the next dose. Patients should not take two doses at the same time.
- Patients should be advised that treatment with BARACLUDE will not cure HBV.
- Patients should be informed that BARACLUDE may lower the amount of HBV in the body, may lower the ability of HBV to multiply and infect new liver cells, and may improve the condition of the liver.
- Patients should be informed that it is not known whether BARACLUDE will reduce their chances of getting liver cancer or cirrhosis.
- Post-treatment Exacerbation of Hepatitis
- Patients should be informed that deterioration of liver disease may occur in some cases if treatment is discontinued, and that they should discuss any change in regimen with their physician.
- HIV/HBV Co-infection
- Patients should be offered HIV antibody testing before starting BARACLUDE therapy. They should be informed that if they have HIV infection and are not receiving effective HIV treatment, BARACLUDE may increase the chance of HIV resistance to HIV medication.
Precautions with Alcohol
- Alcohol-Entecavir interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Baraclude®[2]
Look-Alike Drug Names
There is limited information regarding Entecavir Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ “BARACLUDE® (entecavir) Tablets for Oral Use & Oral Solution. U.S. Full Prescribing Information.” Bristol-Myers Squibb Company, 2005. Revised December 2013. [1]
- ↑ "BARACLUDE (entecavir) tablet, film coated BARACLUDE (entecavir) solution [E.R. Squibb & Sons, L.L.C.]".
{{#subobject:
|Page Name=Entecavir |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Entecavir |Label Name=Entecavir16.png
}}
{{#subobject:
|Label Page=Entecavir |Label Name=Entecavir17.png
}}
{{#subobject:
|Label Page=Entecavir |Label Name=Entecavir18.png
}}
{{#subobject:
|Label Page=Entecavir |Label Name=Entecavir19.png
}}