Endoscopic retrograde cholangiopancreatography
Overview
Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain biliary or pancreatic ductal diseases. ERCP was first introduced in 1968 and was later on accepted as a safe diagnostic and therapeutic tool [1]. Nowadays, as other imaging techniques are evolving and becoming widely used for the diagnosis of diseases of the biliary and pancreatic systems, the use of ERCP became mainly targeted towards therapeutic rather than diagnostic purposes.
ERCP is indicated in biliary tract diseases including choledecholithiasis and benign and malignant biliary strictures, as well as pancreatic diseases including recurrent acute pancreatitis, chronic pancreatitis, pancreatic duct leaks, pancreatic fluid collections and obstructive pancreatic malignancies[2]. There is a variation in the reported rates of complications associated with ERCP, which are mainly pancreatitis, hemorrhage and infection[3].
Procedure
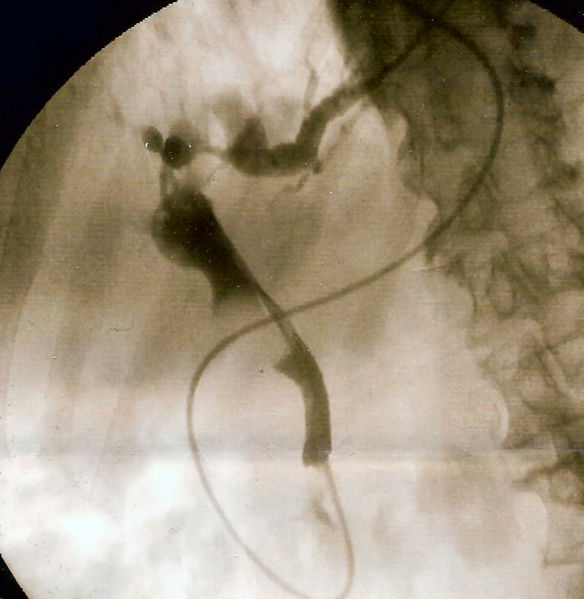
- ERCP is a technique that combines video endoscopy and fluoroscopy. It is usually done in an outpatient setting and the patient is often sedated or anaesthetized. A flexible side viewing camera (endoscope) is inserted through the mouth, down the esophagus, into the stomach, through the pylorus into the duodenum. The ampulla of Vater, which is the opening of the common bile duct and pancreatic duct, is identified. This region can be directly visualized with the endoscopic camera while various procedures are performed.
- Once the ampulla is ientified, a plastic catheter or cannula is inserted through the ampulla, and radiocontrast is injected into the bile ducts, and/or, pancreatic duct.Fluoroscopy, which uses X-rays, is used to locate strictures, blockages, or leakage of bile into the peritoneum (the abdominal cavity) as well as to guide therapeutic procedures.
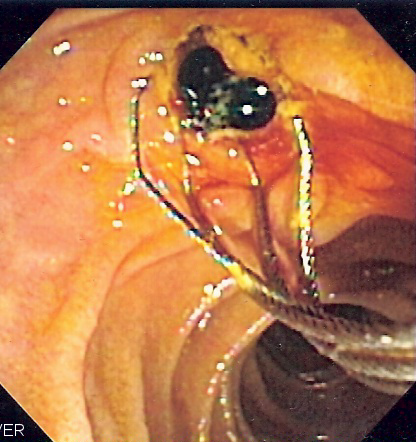
- A wire and balloon may be passed into the bile duct, then inflated in order to expand the opening of the bile duct to allow passage of gallstones. When needed, the opening of the ampulla can be enlarged with an electrified wire (sphincterotome) and access into the bile duct obtained so that gallstones may be removed or other therapy performed.
- Other procedures associated with ERCP include the trawling of the common bile duct with a basket or balloon to remove gallstones and the insertion of a plastic stent to assist the drainage of bile. Also, the pancreatic duct can be cannulated and stents be inserted.
Indications
Biliary Tract Diseases
Choledecholithiasis
- ERCP is the treatment of choice for choledecholithiasis (or gallstones in the common bile duct).
- Role of ERCP:
- Dilatation of the sphincter of Oddi by endoscopic sphincterectomy and subsequent stone extraction.
- Stone removal is done by sofogarty type balloons or wire baskets.
- When the stones are too large to be extracted, lithotripsy can be done to fragment the stones.
- Balloon sphincteroplasty is an alternative for sphincterectomy in patients with coagulopathies.[2]
- Dilatation of the sphincter of Oddi by endoscopic sphincterectomy and subsequent stone extraction.
Biliary strictures or leak
- ERCP is indicated in the treatment of biliary strictures and leak secondary to primary sclerosing cholangitis, chronic pancreatitis, congenital bile duct anomalies and pancreatic transplantation.
- Role of ERCP:
- Endoscopic dilatation by:
- Graduated dilatation
- Balloon
- Stent placement
- Combination of more than one of the previously listed techniques
- Endoscopic brushing and biopsies to rule one malignancy in selected cases.
- Endoscopic dilatation by:
Pancreatic Diseases
Recurrent acute pancreatitis
- ERCP allows the assessment for possible underlying anatomic etiologies causing recurrent pancreatitis. Underlying causes include abnormal ductal anatomy, pancreas divisum, increased tone of the sphincter of Oddi or microlithiasis.
- Role of ERCP:
- Stent placement
- Sphincterctomy
- Analysis of the bile looking for microlithiasis.
Chronic pancreatitis
- Chronic pancreatitis is associated with pancreatic duct stones, strictures and pseudocysts.
- Role of ERCP :
- Pancreatic sphincterectomy and stone removal with/without lithotripsy
- Dilatation and stent placement for the strictures
- Pseucdocyst drainage
Pancreatic duct leaks
- Pancreatic duct leaks are seen in acute pancreatitis, chronic pancreatitis, trauma or after surgery. If left untreated, pancreatic leaks lead to ascites and formation of pseudocysts.
- Role of ERCP:
- Transpapillary stent
- "Bridging" by reconnecting segments of the pancreatic parenchyma
Pancreatic fluid collection
- Pancreatic flui collection can be either in the form of acute pseudocyst, chronic pseudocyst or pancreatic necrosis.
- Role of ERCP:
- Drainage by transpapillary therapy in communicable fluid collections
- Drainage by transgastric or transduodenal therapy in non communicable fluid collections[2]
Pancreatic malignancies
- ERCP is an adjunctive technique to contrast enhanced imaging in the the diagnosis of pancreatic malignancy.
- Role of ERCP:
- Palliative relief of obstruction
- Brush cytology
- Biopsy[2]
Diseases of the Ampulla of Vater
Ampullary adenoma
- Role of ERCP:
- Snare ampillectomy with biliary or pancreatic sphincterectomy.
Dysfunction of the Sphincter of Oddi
Hypertonic Sphincter of Oddi
- Increased tone of the sphincter of Oddi leads to obstruction of the bile and pancreatic secretion pathway and subsequent symptoms of biliary colic.
- Role of ERCP:
- Biliary manometry (diagnostic)
- Biliary sphincterectomy (therapeutic)[2]
Contraindications
Absolute Contraindications
- The uncooperative patient
- Recent attack of acute pancreatitis, within the past several weeks
- Recent myocardial infarction
- Inadequate surgical back-up
- History of contrast dye anaphylaxis
Relative Contraindications
- Poor health condition for surgery
- Severe cardiopulmonary disease
- Ascites
Complications
Pancreatitis
Criteria
- New or worsened abdominal pain, or
- New or prolongation of hospitalization for two or more days, or
- Increase in the serum amylase level at least three times the normal within 24 hours after ERCP[3]
Incidence
- Pancreatitis is the most common complication associated with ERCP.
- The incidence of pancreatitis is estimated to be around 3.5%, however 75 % of patients have elevated pancreatic enzymes in the absence of pancreatitis.[4]
Risk factors
In alphabetical order
- Balloon dilation of biliary sphincter
- History of post-ERCP pancreatitis
- Normal bilirubin
- Pancreatic duct injection
- Precut sphincterotomy
- Suspected sphincter of Oddi dysfunction
- Young age[5]
Prevention
- Substitution of ERCP with an alternative procedure in high risk patients when the chances of therapeutic benefits are low
- Decrease the inflammation induced by ERCP by prophylactic administration of indomethacin and diclofenac before ERCP
- Placement of duct stents in high ridk patients
- The use of wire guided cannulation before injection of the dye to avoid the dye reaching the pancreas[3]
Hemorrhage
Criteria
- Hemorrhage post-ERCP can be immediate or delayed (within two weeks).
- Severity of post-ERCP is classified as follows:
- Mild hemorrhage: endoscopic and clinical evidence of bleeding in the absence of need to transfusion and in the context of a drop in hemoglobin that does not exceed 3 g/dL.
- Moderate hemorrhage: endoscopic and clinical evidence of bleeding that requires transfusion of 4 units or less, but not angiographic intervention or surgery.
- Severe hemorrhage: endoscopic and clinical evidence of bleeding that requires transfusion of 5 units or more, or intervention angiographic or surgical) interventions.[6]
Incidence
- The incidence of post-ERCP hemorrhage is around 1.3%. [7]
Risk factors
In alphabetical order
- Acute cholangitis
- Anticoagulation use within 72 hours
- Coagulopathy
- Papillary Stenosis
- Sphincterectomy
The most important risk factor for post-ERCP hemorrhage is sphincterectomy . The length of incision as well as the use of antiplatelets and NSAIDS do not increase the risk of bleeding following ERCP.[3]
Treatment
- Injection with epinephrine
- Thermal therapy
- Endoscopic clips[3]
Perforation
Criteria
- Guidewire induced perforation, or
- Luminal perforation at a site remote from the papilla
- The perforation of the ampulla during sphincterectomy
Incidence
- The incidence of post-ERCP perforation is between 0.1% and 0.6%.[8]
Risk factors
- Sphincterectomy
- Billroth II anatomy
- Intramural injection of contrast
- Prolonged duration of procedure
- Dilatation of biliary stricture
Prevention
- Biliary and duodenal drainage
- Broad spectrum antibiotics[3]
Infection
Incidence
The incidence of cholangitis is less than 1%[9] and that of cholecystitis is between 0.2 and 0.6%[10]following ERCP.
Risk factors
- Cholangitis:
- Use of combined percutaneous-endoscopic procedures
- Stent placement in malignant strictures
- Presence of jaundice
- Primary sclerosing cholangitis[11]
Cholecystitis:
- Presence of stones in the gallbladder and possibly filling of the gallbladder with contrast during the examination
- Use of self-expandable metal stents
- Incomplete biliary drainage ref name="Fumex">Fumex F, Coumaros D, Napoleon B, et al. Similar performance but higher cholecystitis rate with covered biliary stents: results from a prospective multicenter evaluation. Endoscopy 2006;38:787-92.</ref>
Prevention
- Antibiotic prophylaxis covering gram negative bacteria and enterococci should be considered before an ERCP in patients with known or suspected biliary obstruction in which there is a risk of incomplete drainage by ERCP. This is usually the case of patients with primary sclerosing cholangitis.[3]
Cardiopulmonary Complications
Criteria
- Cardiac arrhythmia
- Hypoxemia
- Aspiration[3]
Incidence
The incidence of cardiovascular complications is approximately 1%.
Risk factors
- Advanced age
- Procedures lasting more than 30 minutes[12]
- Medications used for sedation and analgesia[3]
Prevention
- Use of propofol in anesthesia[13]
Mortality
Antibiotic Prophylaxis
ERCP in Special Situations
ERCP in Pregnancy
ERCP in Children
ERCP in Bariatric Patients
ERCP Versus MRCP
See also
References
- ↑ McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of Vater: a preliminary report. Ann Surg 1968;167:752-6.
- ↑ 2.0 2.1 2.2 2.3 2.4 Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA; et al. (2005). "ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas". Gastrointest Endosc. 62 (1): 1–8. doi:10.1016/j.gie.2005.04.015. PMID 15990812.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 ASGE Standards of Practice Committee. Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V; et al. (2012). "Complications of ERCP". Gastrointest Endosc. 75 (3): 467–73. doi:10.1016/j.gie.2011.07.010. PMID 22341094.
- ↑ AndriulliA,LoperfidoS,NapolitanoG,etal.Incidenceratesofpost-ERCP complications: a systematic survey of prospective studies. Am J Gastro- enterol 2007;102:1781-8.
- ↑ FreemanML.AdverseoutcomesofERCP.GastrointestEndosc2002;56(6 Suppl):S273-82.
- ↑ Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC; et al. (1991). "Endoscopic sphincterotomy complications and their management: an attempt at consensus". Gastrointest Endosc. 37 (3): 383–93. PMID 2070995.
- ↑ AndriulliA,LoperfidoS,NapolitanoG,etal.Incidenceratesofpost-ERCP complications: a systematic survey of prospective studies. Am J Gastro- enterol 2007;102:1781-8.
- ↑ FreemanML.AdverseoutcomesofERCP.GastrointestEndosc2002;56(6 Suppl):S273-82.
- ↑ FreemanML.AdverseoutcomesofERCP.GastrointestEndosc2002;56(6 Suppl):S273-82.
- ↑ Fumex F, Coumaros D, Napoleon B, et al. Similar performance but higher cholecystitis rate with covered biliary stents: results from a prospective multicenter evaluation. Endoscopy 2006;38:787-92.
- ↑ FreemanML.AdverseoutcomesofERCP.GastrointestEndosc2002;56(6 Suppl):S273-82.
- ↑ Fisher L, Fisher A, Thomson A. Cardiopulmonary complications of ERCP in older patients. Gastrointest Endosc 2006;63:948-55
- ↑ Cote GA, Hovis RM, Ansstas MA, et al. Incidence of sedation-related complications with propofol use during advanced endoscopic proce- dures. Clin Gastroenterol Hepatol 2010;8:137-42.
de:Endoskopisch retrograde Cholangiopankreatikographie
nl:Endoscopische retrograde cholangiopancreatografie
fi:Endoskooppinen retrogradinen kolangiopankreatikografia
sv:ERCP