Endoscopic retrograde cholangiopancreatography
Overview
Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain biliary or pancreatic ductal diseases. ERCP was first introduced in 1968 and was later on accepted as a safe diagnostic and therapeutic tool [1]. Nowadays, as other imaging techniques are evolving and becoming widely used for the diagnosis of diseases of the biliary and pancreatic systems, the use of ERCP became mainly targeted towards therapeutic rather than diagnostic purposes.
ERCP is indicated in biliary tract diseases including choledecholithiasis and benign and malignant biliary strictures, as well as pancreatic diseases including recurrent acute pancreatitis, chronic pancreatitis, pancreatic duct leaks, pancreatic fluid collections and obstructive pancreatic malignancies[2]. There is a variation in the reported rates of complications associated with ERCP, which are mainly pancreatitis, hemorrhage and infection[3].
Procedure
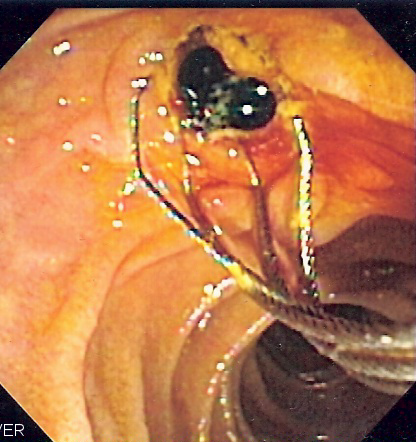
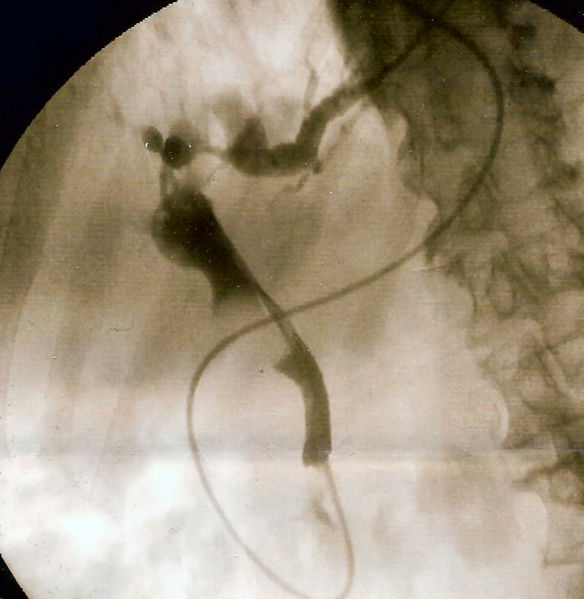
The patient is often sedated or anaesthetized. Then a flexible camera (endoscope) is inserted through the mouth, down the esophagus, into the stomach, through the pylorus into the duodenum where the ampulla of Vater (the opening of the common bile duct and pancreatic duct) exists. The sphincter of Oddi is a muscular valve that controls the opening of the ampulla. The region can be directly visualized with the endoscopic camera while various procedures are performed. A plastic catheter or cannula is inserted through the ampulla, and radiocontrast is injected into the bile ducts, and/or, pancreatic duct. Fluoroscopy is used to look for blockages, or leakage of bile into the peritoneum (the abdominal cavity).
A wire and balloon may be passed into the bile duct, then inflated in order to expand the opening of the bile duct to allow passage of gallstones. When needed, the opening of the ampulla can be enlarged with an electrified wire (sphincterotome) and access into the bile duct obtained so that gallstones may be removed or other therapy performed.
Other procedures associated with ERCP include the trawling of the common bile duct with a basket or balloon to remove gallstones and the insertion of a plastic stent to assist the drainage of bile. Also, the pancreatic duct can be cannulated and stents be inserted. The pancreatic duct requires visualisation in cases of pancreatitis.
Indications
Biliary Tract Diseases
Choledecholithiasis
- ERCP is the treatment of choice for choledecholithiasis (or gallstones in the common bile duct).
- Role of ERCP:
- Dilatation of the sphincter of Oddi by endoscopic sphincterectomy and subsequent stone extraction.
- Stone removal is done by sofogarty type balloons or wire baskets.
- When the stones are too large to be extracted, lithotripsy can be done to fragment the stones.
- Balloon sphincteroplasty is an alternative for sphincterectomy in patients with coagulopathies.
- Dilatation of the sphincter of Oddi by endoscopic sphincterectomy and subsequent stone extraction.
Biliary strictures or leak
- ERCP is indicated in the treatment of biliary strictures and leak secondary to primary sclerosing cholangitis, chronic pancreatitis, congenital bile duct anomalies and pancreatic transplantation.
- Role of ERCP:
- Endoscopic dilatation by:
- Graduated dilatation
- Balloon
- Stent placement
- Combination of more than one of the previously listed techniques
- Endoscopic brushing and biopsies to rule one malignancy in selected cases.
- Endoscopic dilatation by:
Pancreatic Diseases
Recurrent acute pancreatitis
- ERCP allows the assessment for possible underlying anatomic etiologies causing recurrent pancreatitis. Underlying causes include abnormal ductal anatomy, pancreas divisum, increased tone of the sphincter of Oddi or microlithiasis.
- Role of ERCP:
- Stent placement
- Sphincterctomy
- Analysis of the bile looking for microlithiasis.
Chronic pancreatitis
- Chronic pancreatitis is associated with pancreatic duct stones, strictures and pseudocysts.
- Role of ERCP :
- Pancreatic sphincterectomy and stone removal with/without lithotripsy
- Dilatation and stent placement for the strictures
- Pseucdocyst drainage
Pancreatic duct leaks
- Pancreatic duct leaks are seen in acute pancreatitis, chronic pancreatitis, trauma or after surgery. If left untreated, pancreatic leaks lead to ascites and formation of pseudocysts.
- Role of ERCP:
- Transpapillary stent
- "Bridging" by reconnecting segments of the pancreatic parenchyma
Pancreatic fluid collection
- Pancreatic flui collection can be either in the form of acute pseudocyst, chronic pseudocyst or pancreatic necrosis.
- Role of ERCP:
- Drainage by transpapillary therapy in communicable fluid collections
- Drainage by transgastric or transduodenal therapy in non communicable fluid collections
Pancreatic malignancies
- ERCP is an adjunctive technique to contrast enhanced imaging in the the diagnosis of pancreatic malignancy.
- Role of ERCP:
- Palliative relief of obstruction
- Brush cytology
- Biopsy
Diseases of the Ampulla of Vater
Ampullary adenoma
- Role of ERCP:
- Snare ampillectomy with biliary or pancreatic sphincterectomy.
Dysfunction of the Sphincter of Oddi
Hypertonic Sphincter of Oddi
- Increased tone of the sphincter of Oddi leads to obstruction of the bile and pancreatic secretion pathway and subsequent symptoms of biliary colic.
- Role of ERCP:
- Biliary manometry (diagnostic)
- Biliary sphincterectomy (therapeutic)
Contraindications
Absolute Contraindications
- The uncooperative patient
- Recent attack of acute pancreatitis, within the past several weeks
- Recent myocardial infarction
- Inadequate surgical back-up
- History of contrast dye anaphylaxis
Relative Contraindications
- Poor health condition for surgery
- Severe cardiopulmonary disease
- Ascites
Complications
Gut perforation is a risk of any endoscopic procedure as well as the ERCP holding a 5% risk of developing acute pancreatitis.
Dyes: Dyes used to allow the physician to image the organs can cause allergic reactions. Iodine is a component of one of these dyes, and if you are allergic to shellfish, you will be at risk with the dye. Also, the dyes can be harmful to the kidneys. If your kidneys have poor function, the dye could cause renal failure ( called Contrast Nephropathy)[[4]]. If you are at such risk, then ask the physician, ask about how to promote flushing the dye from your system and how to recover from kidney damage. If you are on dialysis, you should be dialyzed after the procedure to flush out the dyes.
Sedation: Experienced anesthesia providers will provide you sedation only in an "as needed" amount to keep you comfortable. Oversedation can result in dangerously low blood pressure and nausea and vomiting. Nausea and vomiting are especially dangerous, as these prevent you from drinking to flush the dyes out of your kidneys.
Antibiotic Prophylaxis
ERCP in Special Situations
ERCP in Pregnancy
ERCP in Children
ERCP in Bariatric Patients
ERCP Versus MRCP
See also
de:Endoskopisch retrograde Cholangiopankreatikographie
nl:Endoscopische retrograde cholangiopancreatografie
fi:Endoskooppinen retrogradinen kolangiopankreatikografia
sv:ERCP
- ↑ McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of Vater: a preliminary report. Ann Surg 1968;167:752-6.
- ↑ Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA; et al. (2005). "ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas". Gastrointest Endosc. 62 (1): 1–8. doi:10.1016/j.gie.2005.04.015. PMID 15990812.
- ↑ ASGE Standards of Practice Committee. Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V; et al. (2012). "Complications of ERCP". Gastrointest Endosc. 75 (3): 467–73. doi:10.1016/j.gie.2011.07.010. PMID 22341094.
- ↑ www.edoctor.co.in/ercp/4522505088