Endoscopic retrograde cholangiopancreatography
Overview
Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain biliary or pancreatic ductal diseases. ERCP was first introduced in 1968 and was later on accepted as a safe diagnostic and therapeutic tool [1]. Nowadays, as other imaging techniques are evolving and becoming widely used for the diagnosis of diseases of the biliary and pancreatic systems, the use of ERCP became mainly targeted towards therapeutic rather than diagnostic purposes.
ERCP is indicated in biliary tract diseases including choledecholithiasis and benign and malignant biliary strictures, as well as pancreatic diseases including recurrent acute pancreatitis, chronic pancreatitis, pancreatic duct leaks, pancreatic fluid collections and obstructive pancreatic malignancies[2]. There is a variation in the reported rates of complications associated with ERCP, which are mainly pancreatitis, hemorrhage and infection[3].
Procedure
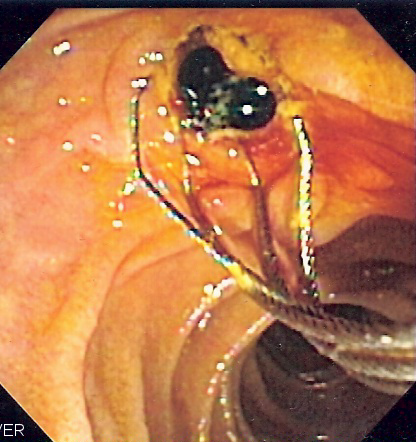
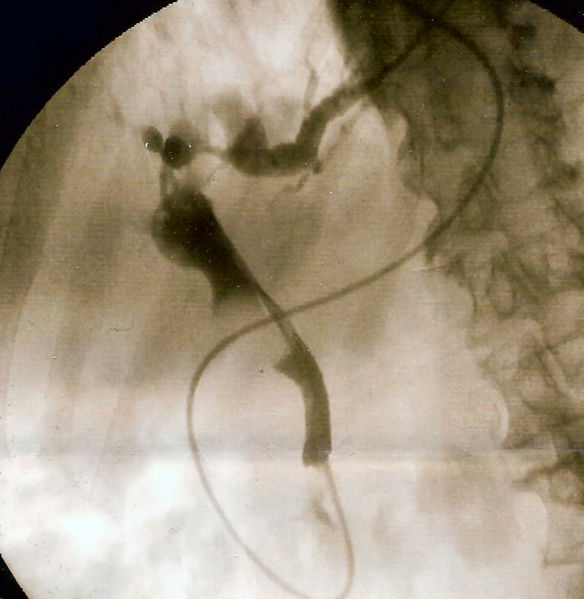
The patient is often sedated or anaesthetized. Then a flexible camera (endoscope) is inserted through the mouth, down the esophagus, into the stomach, through the pylorus into the duodenum where the ampulla of Vater (the opening of the common bile duct and pancreatic duct) exists. The sphincter of Oddi is a muscular valve that controls the opening of the ampulla. The region can be directly visualized with the endoscopic camera while various procedures are performed. A plastic catheter or cannula is inserted through the ampulla, and radiocontrast is injected into the bile ducts, and/or, pancreatic duct. Fluoroscopy is used to look for blockages, or leakage of bile into the peritoneum (the abdominal cavity).
A wire and balloon may be passed into the bile duct, then inflated in order to expand the opening of the bile duct to allow passage of gallstones. When needed, the opening of the ampulla can be enlarged with an electrified wire (sphincterotome) and access into the bile duct obtained so that gallstones may be removed or other therapy performed.
Other procedures associated with ERCP include the trawling of the common bile duct with a basket or balloon to remove gallstones and the insertion of a plastic stent to assist the drainage of bile. Also, the pancreatic duct can be cannulated and stents be inserted. The pancreatic duct requires visualisation in cases of pancreatitis.
Indications
Contraindications:
- Absolute contraindication:
- The uncooperative patient.
- Contraindication
- Recent attack of acute pancreatitis, within the past several weeks.
- Recent myocardial infarction.
- Inadequate surgical back-up
- History of contrast dye anaphylaxis
- Relative contraindications:
- Poor health condition for surgery.
- Severe cardiopulmonary disease.
- Ascites.
Complications
Gut perforation is a risk of any endoscopic procedure as well as the ERCP holding a 5% risk of developing acute pancreatitis.
Dyes: Dyes used to allow the physician to image the organs can cause allergic reactions. Iodine is a component of one of these dyes, and if you are allergic to shellfish, you will be at risk with the dye. Also, the dyes can be harmful to the kidneys. If your kidneys have poor function, the dye could cause renal failure ( called Contrast Nephropathy)[[4]]. If you are at such risk, then ask the physician, ask about how to promote flushing the dye from your system and how to recover from kidney damage. If you are on dialysis, you should be dialyzed after the procedure to flush out the dyes.
Sedation: Experienced anesthesia providers will provide you sedation only in an "as needed" amount to keep you comfortable. Oversedation can result in dangerously low blood pressure and nausea and vomiting. Nausea and vomiting are especially dangerous, as these prevent you from drinking to flush the dyes out of your kidneys.
Antibiotic Prophylaxis
ERCP in Special Situations
ERCP in Pregnancy
ERCP in Children
ERCP in Bariatric Patients
ERCP Versus MRCP
See also
de:Endoskopisch retrograde Cholangiopankreatikographie
nl:Endoscopische retrograde cholangiopancreatografie
fi:Endoskooppinen retrogradinen kolangiopankreatikografia
sv:ERCP
- ↑ McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of Vater: a preliminary report. Ann Surg 1968;167:752-6.
- ↑ Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA; et al. (2005). "ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas". Gastrointest Endosc. 62 (1): 1–8. doi:10.1016/j.gie.2005.04.015. PMID 15990812.
- ↑ ASGE Standards of Practice Committee. Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V; et al. (2012). "Complications of ERCP". Gastrointest Endosc. 75 (3): 467–73. doi:10.1016/j.gie.2011.07.010. PMID 22341094.
- ↑ www.edoctor.co.in/ercp/4522505088