Endometrial cancer natural history, complications and prognosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 7: | Line 7: | ||
==Natural history== | ==Natural history== | ||
*Endometrial cancer forms when there are errors in normal endometrial cell growth. Development of an [[endometrial hyperplasia]] (overgrowth of endometrial cells) is a significant risk factor because hyperplasias can and often do develop into adenocarcinoma, though cancer can develop without the presence of a hyperplasia. Within ten years, 8–30% of atypical endometrial hyperplasias develop into cancer, whereas 1–3% of non-atypical hyperplasias do so. | *Endometrial cancer forms when there are errors in normal endometrial cell growth. Development of an [[endometrial hyperplasia]] (overgrowth of endometrial cells) is a significant risk factor because hyperplasias can and often do develop into [[adenocarcinoma]], though cancer can develop without the presence of a hyperplasia. Within ten years, 8–30% of atypical endometrial hyperplasias develop into cancer, whereas 1–3% of non-atypical hyperplasias do so. | ||
*Development of endometrial cancer is the result of multiple genetic mutations. | *Development of endometrial cancer is the result of multiple genetic mutations. | ||
*Patient has early symptoms like,abnormal uterine bleeding, abnormal menstrual periods, bleeding between normal periods in premenopausal women.Vaginal bleeding and/or spotting in postmenopausal women | *Patient has early symptoms like,abnormal uterine bleeding, abnormal menstrual periods, bleeding between normal periods in premenopausal women.Vaginal bleeding and/or spotting in postmenopausal women | ||
| Line 28: | Line 28: | ||
Another factor found to correlate with extrauterine and nodal spread of tumor is involvement of the capillary-lymphatic space on histopathologic examination. | Another factor found to correlate with extrauterine and nodal spread of tumor is involvement of the capillary-lymphatic space on histopathologic examination. | ||
Three prognostic groupings of clinical stage I disease become possible by careful operative staging. | Three prognostic groupings of clinical stage I disease become possible by careful operative staging. | ||
1. Patients with grade 1 tumors involving only endometrium and no evidence of intraperitoneal disease (i.e., adnexal spread) have a low risk (<5%) of nodal involvement. | 1. Patients with grade 1 tumors involving only [[endometrium]] and no evidence of intraperitoneal disease (i.e., adnexal spread) have a low risk (<5%) of nodal involvement. | ||
2. Patients with grade 2 or 3 tumors and invasion of less than 50% of the myometrium and no intraperitoneal disease have a 5% to 9% incidence of pelvic node involvement and a 4% incidence of positive para-aortic nodes. | 2. Patients with grade 2 or 3 tumors and invasion of less than 50% of the myometrium and no intraperitoneal disease have a 5% to 9% incidence of pelvic node involvement and a 4% incidence of positive para-aortic nodes. | ||
3. Patients with deep muscle invasion and high-grade tumors and/or intraperitoneal disease have a significant risk of nodal spread, 20% to 60% to pelvic nodes and 10% to 30% to para-aortic nodes. | 3. Patients with deep muscle invasion and high-grade tumors and/or intraperitoneal disease have a significant risk of nodal spread, 20% to 60% to pelvic nodes and 10% to 30% to para-aortic nodes. | ||
The following four are statistically significant adverse prognostic factors: | The following four are statistically significant adverse prognostic factors: | ||
:* Myometrial invasion. | :* Myometrial invasion. | ||
:* Vascular invasion. | :* [[Vascular]] invasion. | ||
:* Eight or more mitoses per ten high-power fields. | :* Eight or more mitoses per ten high-power fields. | ||
:* An absence of progesterone receptors. | :* An absence of progesterone receptors. | ||
* Based on Gynecologic Oncology Group (GOG) study following are the other prognostic indicators of clinical outcome | * Based on Gynecologic Oncology Group (GOG) study following are the other prognostic indicators of clinical outcome | ||
:* Oncogene expression. | :* Oncogene expression. | ||
:* DNA ploidy. | :* [[DNA]] ploidy. | ||
:* The fraction of cells in S-phase. | :* The fraction of cells in S-phase. | ||
Revision as of 21:05, 2 September 2015
|
Endometrial cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Endometrial cancer natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Endometrial cancer natural history, complications and prognosis |
|
FDA on Endometrial cancer natural history, complications and prognosis |
|
CDC on Endometrial cancer natural history, complications and prognosis |
|
Endometrial cancer natural history, complications and prognosis in the news |
|
Blogs on Endometrial cancer natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
If left untreated, 8–30% of patients with atypical endometrial hyperplasia may progress to develop endometrial cancer. Common complications of endometrial cancer include vaginal bleeding and metastasis. Depending on the extent of the tumor at the time of diagnosis, the prognosis may vary. However, the prognosis is generally regarded as good.
Natural history
- Endometrial cancer forms when there are errors in normal endometrial cell growth. Development of an endometrial hyperplasia (overgrowth of endometrial cells) is a significant risk factor because hyperplasias can and often do develop into adenocarcinoma, though cancer can develop without the presence of a hyperplasia. Within ten years, 8–30% of atypical endometrial hyperplasias develop into cancer, whereas 1–3% of non-atypical hyperplasias do so.
- Development of endometrial cancer is the result of multiple genetic mutations.
- Patient has early symptoms like,abnormal uterine bleeding, abnormal menstrual periods, bleeding between normal periods in premenopausal women.Vaginal bleeding and/or spotting in postmenopausal women
- As the tumor grows larger, patient may notice symptoms like, trouble urinating, pelvic pain and pain during intercourse
- If the diseases advances and spreads to other organs, the patient may present with dyspnea, cough with blood-stained sputum, persistent pain or discomfort in the chest, swelling in hands/feet, itchiness, jaundice, and/or dark-colored urine
- Once the cancer spreads to the other organs, it is most likely fatal.
Complications
Complications of endometrial cancer include:
- Vaginal bleeding
- Metastasis - usually in the liver and lungs but may occur in other sites
- Cancer recurrence - local (site of the original tumor), regional (in the lymph nodes near the primary tumor) or distal (in another part of the body)
- Common radiation therapy adverse effects - skin discoloration, skin burns, headache, fatigue, hair loss, nausea, vomiting, and/or confusion
- Common chemotherapy adverse effects - hair loss, fatigue, weakness, nausea, vomiting, risk of infection, and/or diarrhea
- A perforation (hole) of the uterus may occur during a D&C or an endometrial biopsy.
- Common post-surgical complications -hematoma, bleeding, infection
- Death
Prognosis
Another factor found to correlate with extrauterine and nodal spread of tumor is involvement of the capillary-lymphatic space on histopathologic examination. Three prognostic groupings of clinical stage I disease become possible by careful operative staging. 1. Patients with grade 1 tumors involving only endometrium and no evidence of intraperitoneal disease (i.e., adnexal spread) have a low risk (<5%) of nodal involvement. 2. Patients with grade 2 or 3 tumors and invasion of less than 50% of the myometrium and no intraperitoneal disease have a 5% to 9% incidence of pelvic node involvement and a 4% incidence of positive para-aortic nodes. 3. Patients with deep muscle invasion and high-grade tumors and/or intraperitoneal disease have a significant risk of nodal spread, 20% to 60% to pelvic nodes and 10% to 30% to para-aortic nodes. The following four are statistically significant adverse prognostic factors:
- Myometrial invasion.
- Vascular invasion.
- Eight or more mitoses per ten high-power fields.
- An absence of progesterone receptors.
- Based on Gynecologic Oncology Group (GOG) study following are the other prognostic indicators of clinical outcome
- Oncogene expression.
- DNA ploidy.
- The fraction of cells in S-phase.
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with uterine cancer was 83.2%.[1]
- When stratified by age, the 5-year relative survival of patients with uterine cancer was 86.6% and 73.1% for patients <65 and ≥ 65 years of age respectively.[1]
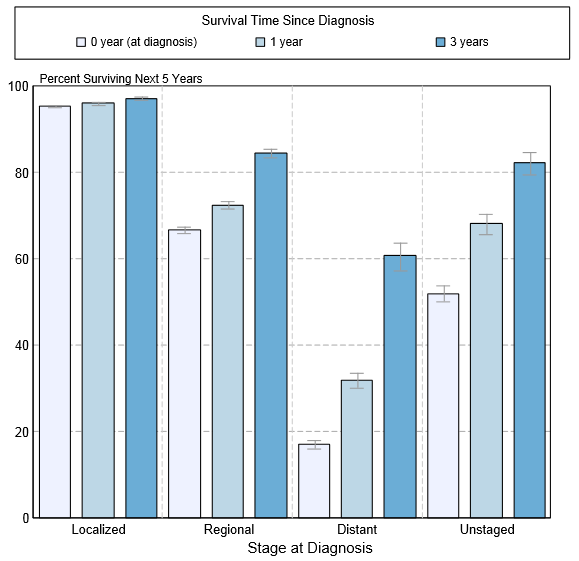
- The survival of patients with uterine cancer varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of uterine cancer:[1]
| Stage | 5-year relative survival (%), (2004-2010) |
| All stages | 81.5% |
| Localized | 95.1% |
| Regional | 67.7% |
| Distant | 17,5% |
| Unstaged | 47.9% |
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of uterine cancer by stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[1]
References
- ↑ 1.0 1.1 1.2 1.3 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.