Elagolix
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Zach Leibowitz [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Elagolix is a gonadotropin-releasing hormone (GnRH) receptor antagonist that is FDA approved for the management of moderate to severe pain associated with endometriosis. Common adverse reactions include hot flushes and night sweats, headache, nausea, insomnia, amenorrhea, anxiety, arthralgia, depression-related adverse reactions and mood changes.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- Elagolix is indicated for the management of moderate to severe pain associated with endometriosis.
Dosage
- Normal liver function or mild hepatic impairment: 150 mg once daily for up to 24 months or 200 mg twice daily for up to 6 months.
- Moderate hepatic impairment: 150 mg once daily for up to 6 months.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding elagolix Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding elagolix Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and effectiveness of elagolix in patients less than 18 years of age have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding elagolix Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding elagolix Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Elagolix is contraindicated in women:
- Who are pregnant. Exposure to elagolix early in pregnancy may increase the risk of early pregnancy loss.
- With known osteoporosis because of the risk of further bone loss.
- With severe hepatic impairment because of the risk of bone loss.
- With concomitant use of strong organic anion transporting polypeptide (OATP) 1B1 inhibitors (e.g., cyclosporine and gemfibrozil).
Warnings
Bone Loss
- Elagolix causes a dose-dependent decrease in bone mineral density (BMD). BMD loss is greater with increasing duration of use and may not be completely reversible after stopping treatment. The impact of these BMD decreases on long-term bone health and future fracture risk are unknown. Consider assessment of BMD in patients with a history of a low-trauma fracture or other risk factors for osteoporosis or bone loss, and do not use in women with known osteoporosis. Limit the duration of use to reduce the extent of bone loss.
- Although the effect of supplementation with calcium and vitamin D was not studied, such supplementation may be beneficial for all patients.
Change in Menstrual Bleeding Pattern and Reduced Ability to Recognize Pregnancy
- Women who take elagolix may experience a reduction in the amount, intensity or duration of menstrual bleeding, which may reduce the ability to recognize the occurrence of a pregnancy in a timely manner. Perform pregnancy testing if pregnancy is suspected, and discontinue elagolix if pregnancy is confirmed.
Suicidal Ideation, Suicidal Behavior, and Exacerbation of Mood Disorders
- Suicidal ideation and behavior, including one completed suicide, occurred in subjects treated with elagolix in the endometriosis clinical trials. Elagolix subjects had a higher incidence of depression and mood changes compared to placebo, and elagolix subjects with a history of suicidality or depression had a higher incidence of depression compared to subjects without such a history. Promptly evaluate patients with depressive symptoms to determine whether the risks of continued therapy outweigh the benefits. Patients with new or worsening depression, anxiety or other mood changes should be referred to a mental health professional, as appropriate. Advise patients to seek immediate medical attention for suicidal ideation and behavior. Reevaluate the benefits and risks of continuing elagolix if such events occur.
Hepatic Transaminase Elevations
- In clinical trials, dose-dependent elevations of serum alanine aminotransferase (ALT) at least 3-times the upper limit of the reference range occurred with elagolix. Use the lowest effective dose of elagolix and instruct patients to promptly seek medical attention in case of symptoms or signs that may reflect liver injury, such as jaundice. Promptly evaluate patients with elevations in liver tests to determine whether the benefits of continued therapy outweigh the risks.
Reduced Efficacy with Estrogen-Containing Contraceptives
- Based on the mechanism of action of elagolix, estrogen containing contraceptives are expected to reduce the efficacy of elagolix. The effect of progestin-only contraceptives on the efficacy of elagolix is unknown. Advise women to use non-hormonal contraceptives during treatment with elagolix and for one week after discontinuing elagolix.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
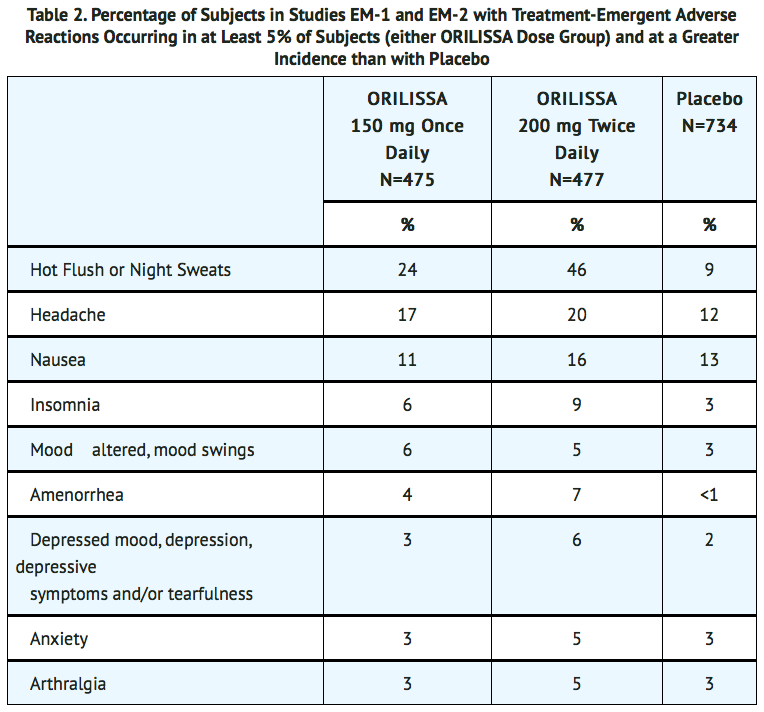
- The safety of elagolix was evaluated in two six-month, randomized, double-blind, placebo-controlled clinical trials [EM-1 (NCT01620528) and EM-2 (NCT01931670)] in which a total of 952 adult women with moderate to severe pain associated with endometriosis were treated with elagolix (475 with 150 mg once daily and 477 with 200 mg twice daily) and 734 were treated with placebo. The population age range was 18-49 years old. Women who completed six months of treatment and met eligibility criteria continued treatment in two uncontrolled, blinded six-month extension trials [EM-3 (NCT01760954) and EM-4 (NCT02143713)], for a total treatment duration of up to 12 months.
Serious Adverse Events
- Overall, the most common serious adverse events reported for subjects treated with elagolix in the two placebo-controlled clinical trials (Studies EM-1 and EM-2) included appendicitis (0.3%), abdominal pain (0.2%), and back pain (0.2%). In these trials, 0.2% of subjects treated with elagolix 150 mg once daily and 0.2% of subjects treated with elagolix 200 mg twice daily discontinued therapy due to serious adverse reactions compared to 0.5% of those given placebo.
Adverse Reactions Leading to Study Discontinuation
- In the two placebo-controlled clinical trials (Studies EM-1 and EM-2), 5.5% of subjects treated with elagolix 150 mg once daily and 9.6% of subjects treated with elagolix 200 mg twice daily discontinued therapy due to adverse reactions compared to 6.0% of those given placebo. Discontinuations were most commonly due to hot flushes or night sweats (1.1% with 150 mg once daily and 2.5% with 200 mg twice daily) and nausea (0.8% with 150 mg once daily and 1.5% with 200 mg twice daily) and were dose-related. The majority of discontinuations due to hot flushes or night sweats (10 of 17, 59%) and nausea (7 of 11, 64%) occurred within the first 2 months of therapy.
- In the two extension trials (Studies EM-3 and EM-4), discontinuations were most commonly due to decreased bone mineral density and were dose-related. In these trials, 0.3% of subjects treated with elagolix 150 mg once daily and 3.6% of subjects treated with elagolix 200 mg twice daily discontinued therapy due to decreased BMD.
Common Adverse Reactions: Adverse reactions reported in ≥ 5% of women in the two placebo-controlled trials in either elagolix dose group and at a greater frequency than placebo are noted in the following table.
Less Common Adverse Reactions:
- In Study EM-1 and Study EM-2, adverse reactions reported in ≥ 3% and < 5% in either elagolix dose group and greater than placebo included: decreased libido, diarrhea, abdominal pain, weight gain, dizziness, constipation and irritability.
- The most commonly reported adverse reactions in the extension trials (EM-3 and EM-4) were similar to those in the placebo-controlled trials.
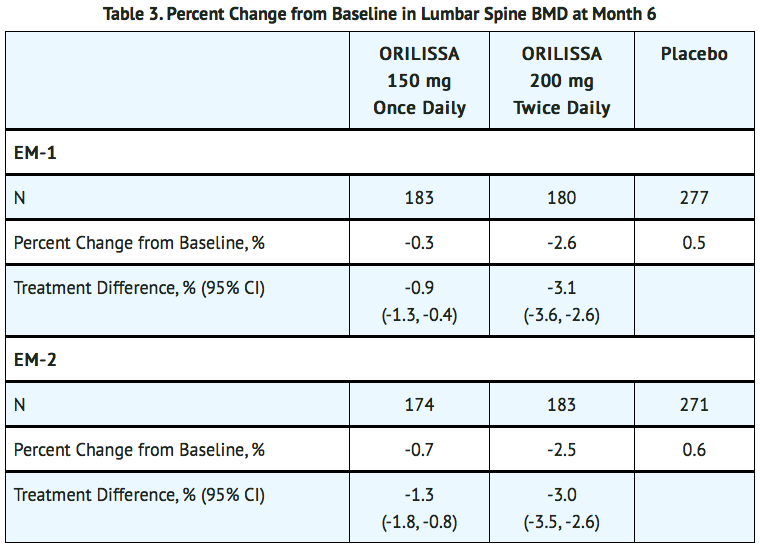
Bone Loss
- The effect of elagolix on bone mineral density was assessed by dual energy X-ray absorptiometry (DXA).
- In Studies EM-1 and EM-2, there was a dose-dependent decrease in BMD in elagolix-treated subjects compared to an increase in placebo-treated subjects.
- In Study EM-1, compared to placebo, the mean change from baseline in lumbar spine BMD at 6 months was -0.9% (95% CI: -1.3, -0.4) with elagolix 150 mg once daily and -3.1% (95% CI: -3.6, -2.6) with elagolix 200 mg twice daily (TABLE 3). The percentage of subjects with greater than 8% BMD decrease in lumbar spine, total hip or femoral neck at any time point during the placebo-controlled treatment period was 2% with elagolix 150 mg once daily, 7% with elagolix 200 mg twice daily and < 1% with placebo. In the blinded extension Study EM-3, continued bone loss was observed with 12 months of continuous treatment with elagolix. The percentage of subjects with greater than 8% BMD decrease in lumbar spine, total hip or femoral neck at any time point during the extension treatment period was 8% with continuous elagolix 150 mg once daily and 21% with continuous elagolix 200 mg twice daily.
- In Study EM-2, compared to placebo, the mean change from baseline in lumbar spine BMD at 6 months was -1.3% (95% CI: -1.8, -0.8) with elagolix 150 mg once daily and -3.0% (95% CI: -3.5, -2.6) with elagolix 200 mg twice daily (TABLE 3). The percentage of subjects with greater than 8% BMD decrease in lumbar spine, total hip or femoral neck at any time point during the placebo-controlled treatment period was < 1% with elagolix 150 mg once daily, 6% with elagolix 200 mg twice daily and 0% with placebo. In the blinded extension Study EM-4, continued bone loss was observed with 12 months of continuous treatment with elagolix. The percentage of subjects with greater than 8% BMD decrease in lumbar spine, total hip or femoral neck at any time point during the extension treatment period was 2% with continuous elagolix 150 mg once daily and 21% with continuous elagolix 200 mg twice daily.
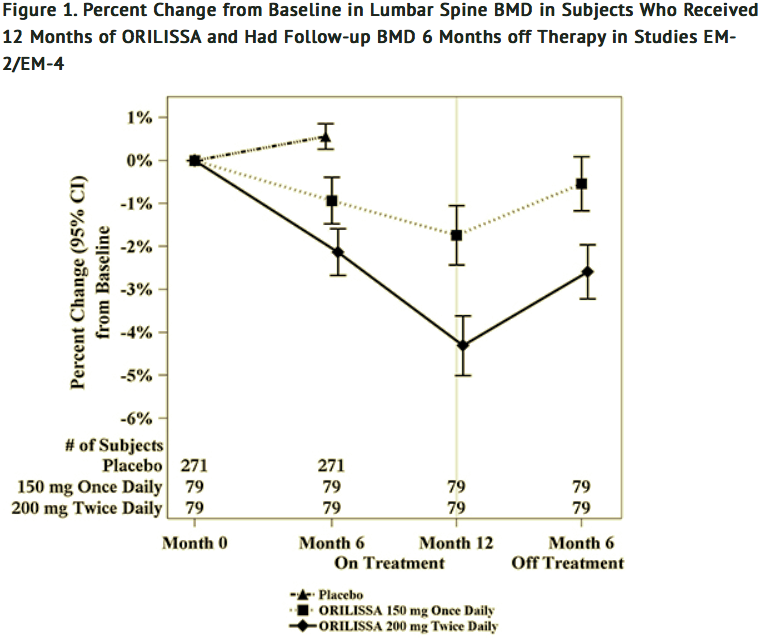
- To assess for recovery, the change in lumbar spine BMD over time was analyzed for subjects who received continuous treatment with elagolix 150 mg once daily or elagolix 200 mg twice daily for up to 12 months and who were then followed after cessation of therapy for an additional 6 months. Partial recovery of BMD was seen in these subjects (Figure 1).
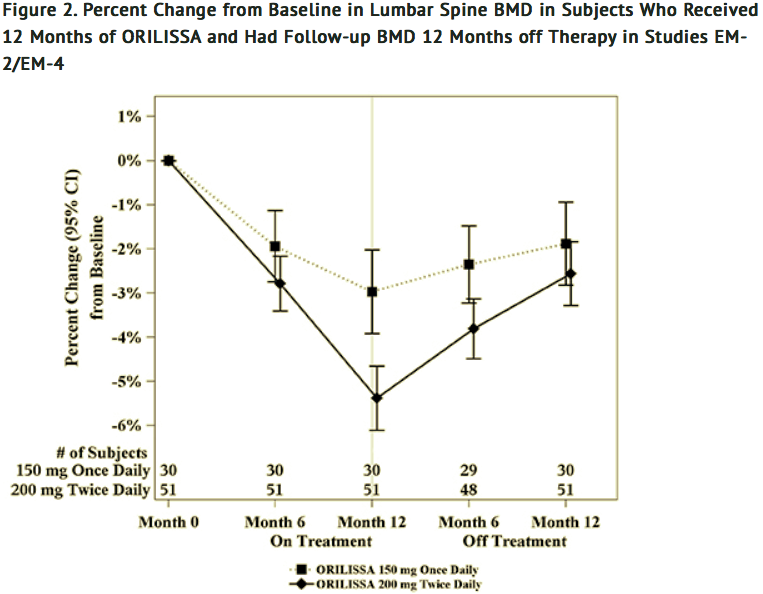
- In Study EM-3, if a subject had BMD loss of more than 1.5% at the lumbar spine or more than 2.5% at the total hip at the end of treatment, follow-up DXA was required after 6 months off-treatment. In Study EM-4, all subjects were required to have a follow-up DXA 6 months off treatment regardless of change in BMD and if a subject had BMD loss of more than 1.5% at the lumbar spine or more than 2.5% at the total hip after 6 months off treatment, follow-up DXA was required after 12 months off-treatment. Figure 2 shows the change in lumbar spine BMD for the subjects in Study EM-2/EM-4 who completed 12 months of treatment with elagolix and who had a follow-up DXA 12-months off treatment.
Suicidal Ideation, Suicidal Behavior and Exacerbation of Mood Disorders
- In the placebo-controlled trials (Studies EM-1 and EM-2), elagolix was associated with adverse mood changes (see Table 2 and Table 4), particularly in those with a history of depression.
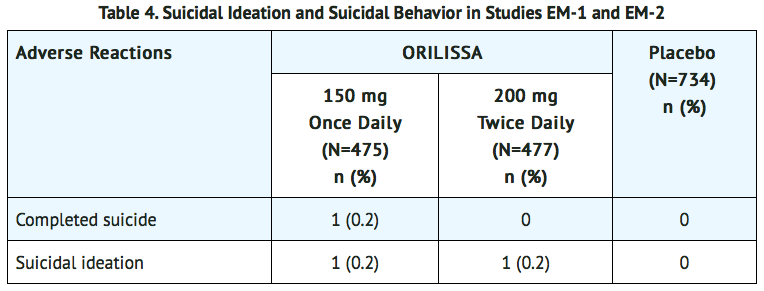
- A 44-year-old woman received 31 days of elagolix 150 mg once daily then completed suicide 2 days after elagolix discontinuation. She had no relevant past medical history; life stressors were noted.
- Among the 2090 subjects exposed to elagolix in the endometriosis Phase 2 and Phase 3 studies, there were four reports of suicidal ideation. In addition to the two subjects in Table 4, there were two additional reports of suicidal ideation: one subject in EM-3 (150 mg once daily) and one in a Phase 2 study (75 mg once daily, an unapproved dose). Three of these subjects had a history of depression. Two subjects discontinued elagolix and two completed the clinical trial treatment periods.
Hepatic Transaminase Elevations
- In the placebo-controlled clinical trials (Studies EM-1 and EM-2), dose-dependent asymptomatic elevations of serum ALT to at least 3-times the upper limit of the reference range occurred during treatment with elagolix (150 mg once daily – 1/450, 0.2%; 200 mg twice daily – 5/443, 1.1%; placebo – 1/696, 0.1%). Similar increases were seen in the extension trials (Studies EM-3 and EM-4).
Changes in Lipid Parameters
- Dose-dependent increases in total cholesterol, low-density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C), and serum triglycerides were noted during elagolix treatment in EM-1 and EM-2. In EM-1 and EM-2, 12% and 1% of subjects with mildly elevated LDL-C (130-159 mg/dL) at baseline had an increase in LDL-C concentrations to 190 mg/dL or higher during treatment with elagolix and placebo, respectively. In EM-1 and EM-2, 4% and 1% of subjects with mildly elevated serum triglycerides (150-300 mg/dL) at baseline had an increase in serum triglycerides to at least 500 mg/dL during treatment with elagolix and placebo, respectively. The highest measured serum triglyceride concentration during treatment with elagolix was 982 mg/dL.
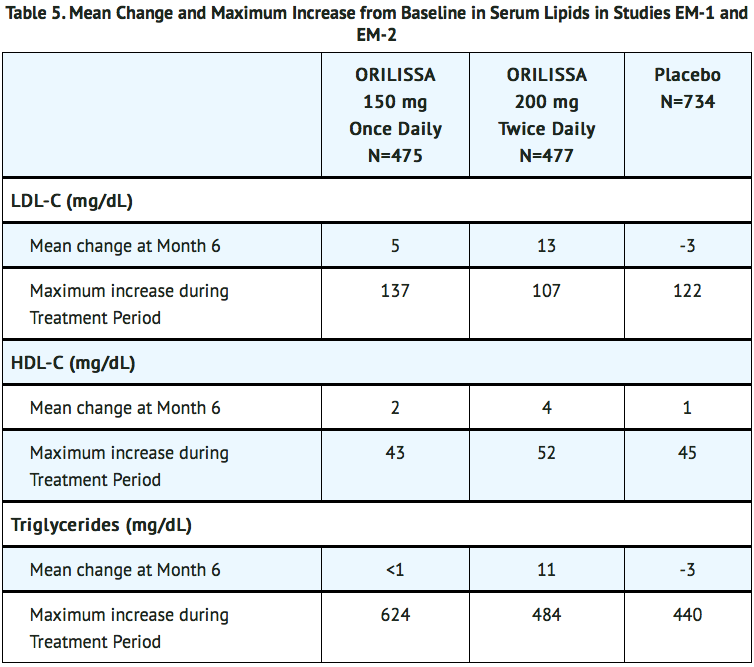
- Lipid increases occurred within 1 to 2 months after the start of elagolix and remained stable thereafter over 12 months.
Hypersensitivity Reactions
- In Studies EM-1 and EM-2, non-serious hypersensitivity reactions including rash occurred in 5.8% of elagolix treated-subjects and 6.1% of placebo-treated subjects. These events led to study drug discontinuation in 0.4% of elagolix-treated subjects and 0.5% of placebo-treated subjects.
Endometrial Effects
- Endometrial biopsies were performed in subjects in Study EM-1 and its extension at Month 6 and Month 12. These biopsies showed a dose-dependent decrease in proliferative and secretory biopsy patterns and an increase in quiescent/minimally stimulated biopsy patterns. There were no abnormal biopsy findings on treatment, such as endometrial hyperplasia or cancer.
- Based on transvaginal ultrasound, during the course of a 3-menstrual cycle study in healthy women, elagolix 150 mg once daily and 200 mg twice daily resulted in a dose-dependent decrease from baseline in mean endometrial thickness.
Effects on menstrual bleeding patterns
- The effects of elagolix on menstrual bleeding were evaluated for up to 12 months using an electronic daily diary where subjects classified their flow of menstrual bleeding (if present in the last 24 hours) as spotting, light, medium, or heavy. Elagolix led to a dose-dependent reduction in mean number of bleeding and spotting days and bleeding intensity in those subjects who reported menstrual bleeding.
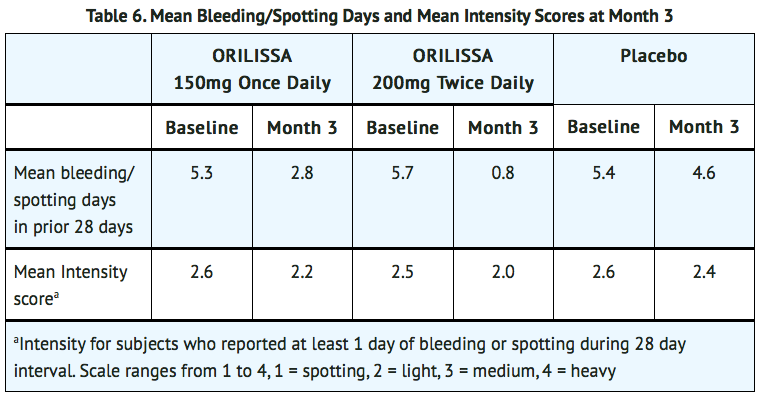
- Elagolix also demonstrated a dose-dependent increase in the percentage of women with amenorrhea (defined as no bleeding or spotting in a 56-day interval) over the treatment period. The incidence of amenorrhea during the first six months of treatment ranged from 6-17% for elagolix 150 mg once daily, 13-52% for elagolix 200 mg twice daily and less than 1% for placebo. During the second 6 months of treatment, the incidence of amenorrhea ranged from 11-15% for elagolix 150 mg once daily and 46-57% for elagolix 200 mg twice daily.
- After 6 months of therapy with elagolix 150 mg once daily, resumption of menses after stopping treatment was reported by 59%, 87% and 95% of women within 1, 2, and 6 months, respectively. After 6 months of therapy with elagolix 200 mg twice daily, resumption of menses after stopping treatment was reported by 60%, 88%, and 97% of women within 1, 2, and 6 months, respectively.
- After 12 months of therapy with elagolix 150 mg once daily resumption of menses after stopping treatment was reported by 77%, 95% and 98% of women within 1, 2, and 6 months respectively. After 12 months of therapy with elagolix 200 mg twice daily resumption of menses after stopping treatment was reported by 55%, 91% and 96% of women within 1, 2, and 6 months respectively.
Postmarketing Experience
There is limited information regarding Elagolix Postmarketing Experience in the drug label.
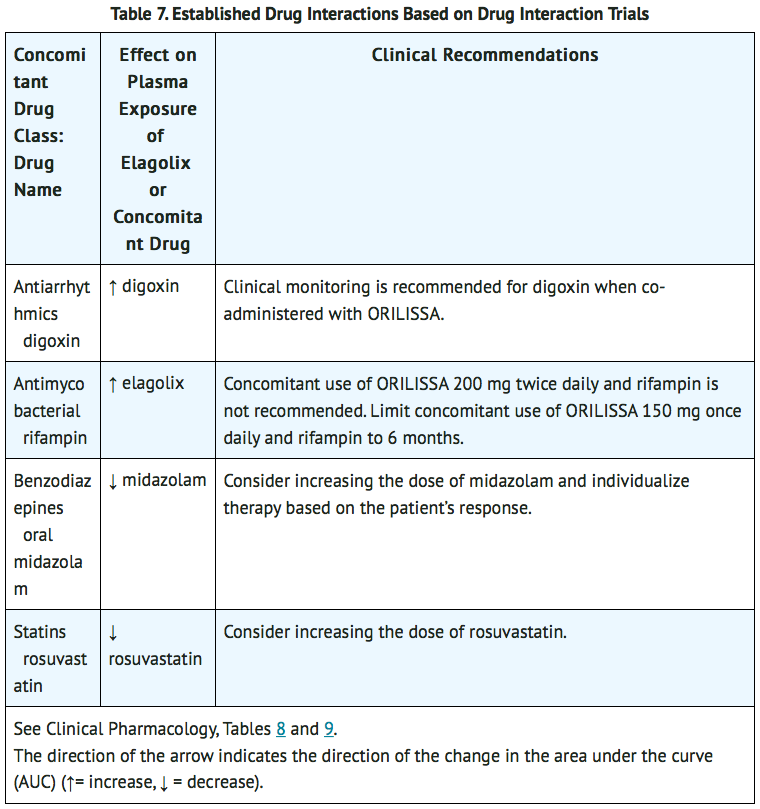
Drug Interactions
Potential for Elagolix to Affect Other Drugs
- Elagolix is a weak to moderate inducer of cytochrome P450 (CYP) 3A. Co-administration with elagolix may decrease plasma concentrations of drugs that are substrates of CYP3A.
- Elagolix is an inhibitor of efflux transporter P-glycoprotein (P-gp). Co-administration with elagolix may increase plasma concentrations of drugs that are substrates of P-gp (e.g., digoxin).
Potential for Other Drugs to Affect elagolix
- Elagolix is a substrate of CYP3A, P-gp, and OATP1B1.
- Concomitant use of elagolix 200 mg twice daily and strong CYP3A inhibitors for more than 1 month is not recommended. Limit concomitant use of elagolix 150 mg once daily and strong CYP3A inhibitors to 6 months.
- Co-administration of elagolix with drugs that induce CYP3A may decrease elagolix plasma concentrations.
- The effect of concomitant use of P-gp inhibitors or inducers on the pharmacokinetics of elagolix is unknown. Co-administration of elagolix with drugs that inhibit OATP1B1 may increase elagolix plasma concentrations. Concomitant use of elagolix and strong OATP1B1 inhibitors (e.g., cyclosporine and gemfibrozil) is contraindicated.
Drug Interactions- Examples and Clinical Management
- TABLE 7 summarizes the effect of co-administration of elagolix on concentrations of concomitant drugs and the effect of concomitant drugs on elagolix.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Risk Summary
- Exposure to elagolix early in pregnancy may increase the risk of early pregnancy loss. Use of elagolix is contraindicated in pregnant women. Discontinue elagolix if pregnancy occurs during treatment.
- The limited human data with the use of elagolix in pregnant women are insufficient to determine whether there is a risk for major birth defects or miscarriage. Although two cases of congenital malformations were reported in clinical trials with elagolix, no pattern was identified and miscarriages were reported at a similar incidence across treatment groups.
- When pregnant rats and rabbits were orally dosed with elagolix during the period of organogenesis, postimplantation loss was observed in pregnant rats at doses 20 times the maximum recommended human dose (MRHD). Spontaneous abortion and total litter loss was observed in rabbits at doses 7 and 12 times the MRHD. There were no structural abnormalities in the fetuses at exposures up to 40 and 12 times the MRHD for the rat and rabbit, respectively.
- The background risk for major birth defects and miscarriage in the indicated population are unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
- There were 49 pregnancies reported in clinical trials of more than 3,500 women (of whom more than 2,000 had endometriosis) treated with elagolix for up to 12 months. These pregnancies occurred while the women were receiving elagolix or within 30 days after stopping elagolix. Among these 49 pregnancies, two major congenital malformations were reported. In one case of infant cleft palate, the mother was treated with elagolix 150 mg daily and the estimated fetal exposure to elagolix occurred during the first 30 days of pregnancy. In one case of infant tracheoesophageal fistula, the mother was treated with elagolix 150 mg daily and the estimated fetal exposure to elagolix occurred during the first 15 days of pregnancy.
- Among these 49 pregnancies, there were five cases of spontaneous abortion (miscarriage) compared to five cases among the 20 pregnancies that occurred in more than 1100 women treated with placebo. Although the duration of fetal exposure was limited in elagolix clinical trials, there were no apparent decreases in birth weights associated with elagolix in comparison to placebo.
Animal Data
- Embryofetal development studies were conducted in the rat and rabbit. Elagolix was administered by oral gavage to pregnant rats (25 animals/dose) at doses of 0, 300, 600 and 1200 mg/kg/day and to rabbits (20 animals/dose) at doses of 0, 100, 150, and 200 mg/kg/day, during the period of organogenesis (gestation day 6-17 in the rat and gestation day 7-20 in the rabbit).
- In rats, maternal toxicity was present at all doses and included six deaths and decreases in body weight gain and food consumption. Increased postimplantation losses were present in the mid dose group, which was 20 times the MRHD based on AUC. In rabbits, three spontaneous abortions and a single total litter loss were observed at the highest, maternally toxic dose, which was 12 times the MRHD based on AUC. A single total litter loss occurred at a lower non-maternally toxic dose of 150 mg/kg/day, which was 7 times the MRHD.
- No fetal malformations were present at any dose level tested in either species even in the presence of maternal toxicity. At the highest doses tested, the exposure margins were 40 and 12 times the MRHD for the rat and rabbit, respectively. However, because elagolix binds poorly to the rat gonadotropin-releasing hormone (GnRH) receptor (~1000 fold less than to the human GnRH receptor), the rat study is unlikely to identify pharmacologically mediated effects of elagolix on embryofetal development. The rat study is still expected to provide information on potential non-target-related effects of elagolix.
- In a pre- and postnatal development study in rats, elagolix was given in the diet to achieve doses of 0, 100 and 300 mg/kg/day (25 per dose group) from gestation day 6 to lactation day 20. There was no evidence of maternal toxicity. At the highest dose, two dams had total litter loss, and one failed to deliver. Pup survival was decreased from birth to postnatal day 4. Pups had lower birth weights and lower body weight gains were observed throughout the pre-weaning period at 300 mg/kg/day. Smaller body size and effect on startle response were associated with lower pup weights at 300 mg/kg/day. Post-weaning growth, development and behavioral endpoints were unaffected.
- Maternal plasma concentrations in rats on lactation day 21 at 100 and 300 mg/kg/day (47 and 125 ng/mL) were 0.06-fold and 0.16-fold the maximal elagolix concentration (Cmax) in humans at the MRHD. Because the exposures achieved in rats were much lower than the human MRHD, this study is not predictive of potentially higher lactational exposure in humans.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Elagolix in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Elagolix during labor and delivery.
Nursing Mothers
Risk Summary
- There is no information on the presence of elagolix or its metabolites in human milk, the effects on the breastfed child, or the effects on milk production. There are no adequate animal data on the excretion of elagolix in milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for elagolix and any potential adverse effects on the breastfed child from elagolix.
Data
- There are no adequate animal data on excretion of elagolix in milk.
Pediatric Use
- Safety and effectiveness of elagolix in patients less than 18 years of age have not been established.
Geriatic Use
There is no FDA guidance on the use of Elagolix in geriatric settings.
Gender
There is no FDA guidance on the use of Elagolix with respect to specific gender populations.
Race
There is no FDA guidance on the use of Elagolix with respect to specific racial populations.
Renal Impairment
- No dose adjustment of elagolix is required in women with any degree of renal impairment or end-stage renal disease (including women on dialysis).
Hepatic Impairment
- No dosage adjustment of elagolix is required for women with mild hepatic impairment (Child-Pugh A). Only the 150 mg once daily regimen is recommended for women with moderate hepatic impairment (Child-Pugh B) and the duration of treatment should be limited to 6 months.
- Elagolix is contraindicated in women with severe hepatic impairment (Child-Pugh C).
Females of Reproductive Potential and Males
- Based on the mechanism of action, there is a risk of early pregnancy loss if elagolix is administered to a pregnant woman.
Pregnancy Testing
- Exclude pregnancy before initiating treatment with elagolix. Perform pregnancy testing if pregnancy is suspected during treatment with elagolix.
Contraception
- Advise women to use effective non-hormonal contraception during treatment with elagolix and for one week after discontinuing elagolix.
Immunocompromised Patients
There is no FDA guidance one the use of Elagolix in patients who are immunocompromised.
Administration and Monitoring
Administration
Important Dosing Information
- Exclude pregnancy before starting elagolix or start elagolix within 7 days from the onset of menses.
- Take elagolix at approximately the same time each day, with or without food.
- Use the lowest effective dose, taking into account the severity of symptoms and treatment objectives.
- Limit the duration of use because of bone loss (Table 1).
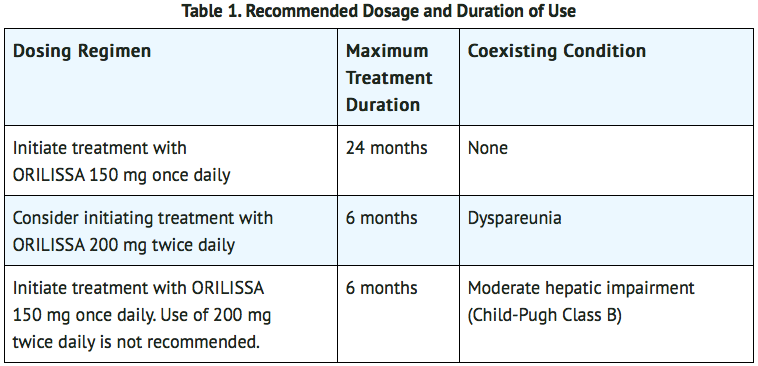
Hepatic Impairment
- No dosage adjustment of elagolix is required in women with mild hepatic impairment (Child-Pugh A).
- Compared to women with normal liver function, those with moderate hepatic impairment had approximately 3-fold higher elagolix exposures and those with severe hepatic impairment had approximately 7-fold higher elagolix exposures. Because of these increased exposures and risk for bone loss:
- Elagolix 150 mg once daily is recommended for women with moderate hepatic impairment (Child-Pugh B) with the duration of treatment limited to 6 months. Use of elagolix 200 mg twice daily is not recommended for women with moderate hepatic impairment.
- Elagolix is contraindicated in women with severe hepatic impairment (Child-Pugh C).
Missed Dose
- Instruct the patient to take a missed dose of elagolix on the same day as soon as she remembers and then resume the regular dosing schedule.
- 150 mg once daily: take no more than 1 tablet each day.
- 200 mg twice daily: take no more than 2 tablets each day.
Monitoring
There is limited information regarding Elagolix Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Elagolix and IV administrations.
Overdosage
- In case of overdose, monitor the patient for any signs or symptoms of adverse reactions and initiate appropriate symptomatic treatment, as needed.
Pharmacology
Mechanism of Action
- Elagolix is a GnRH receptor antagonist that inhibits endogenous GnRH signaling by binding competitively to GnRH receptors in the pituitary gland. Administration of elagolix results in dose-dependent suppression of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), leading to decreased blood concentrations of the ovarian sex hormones, estradiol and progesterone.
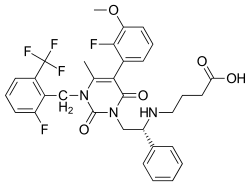
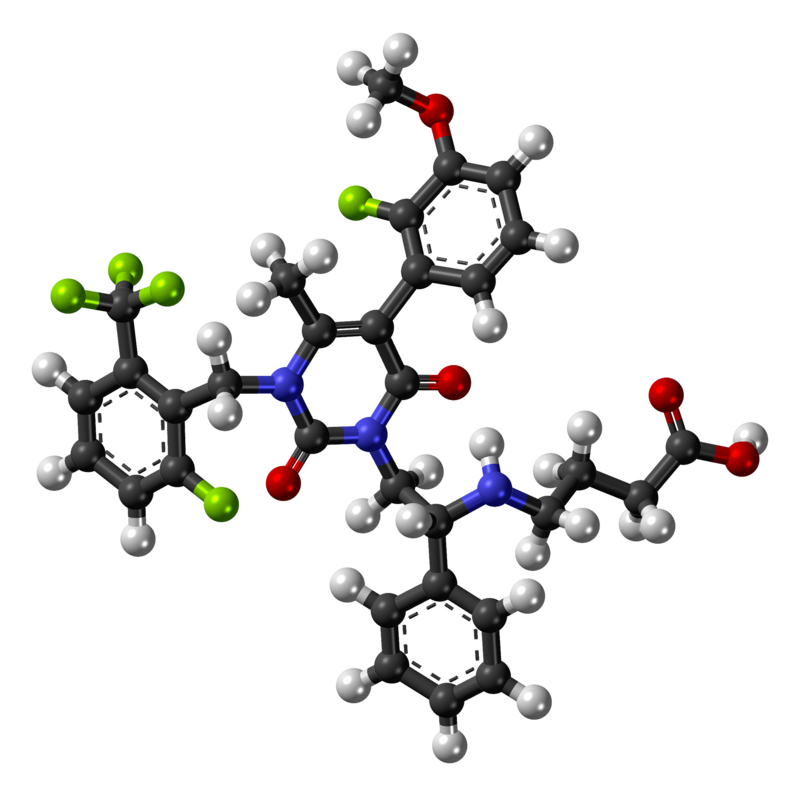
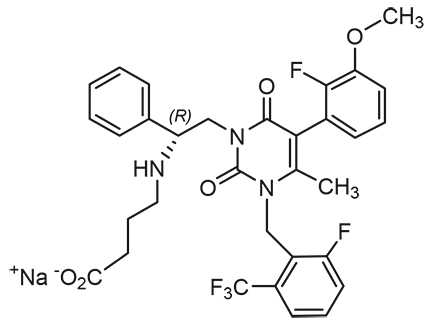
Structure
- Elagolix sodium has a molecular formula of C32H29F5N3O5Na and a molecular weight of 653.58. Elagolix free acid has a molecular weight of 631.60.
- Elagolix sodium has the following structural formula:
Pharmacodynamics
Effect on Ovulation and Estradiol
- In a 3-menstrual cycle study in healthy women, elagolix 150 mg once daily and 200 mg twice daily resulted in an ovulation rate of approximately 50% and 32%, respectively. In the Phase 3 trials in women with endometriosis, elagolix caused a dose-dependent reduction in median estradiol concentrations to approximately 42 pg/mL for 150 mg once daily regimen and 12 pg/mL for the 200 mg twice daily regimen.
Cardiac Electrophysiology
- The effect of elagolix on the QTc interval was evaluated in a randomized, placebo- and positive-controlled, open-label, single-dose, crossover thorough QTc study in 48 healthy adult premenopausal women. Elagolix concentrations in subjects given a single dose of 1200 mg was 17-times higher than the concentration in subjects given elagolix 200 mg twice daily. There was no clinically relevant prolongation of the QTc interval.
Pharmacokinetics
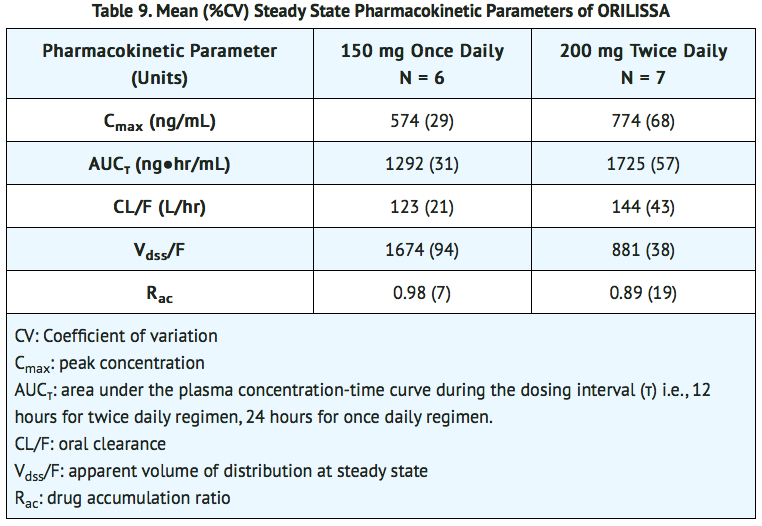
- The pharmacokinetic properties of elagolix in healthy subjects are summarized in TABLE 8. The steady state pharmacokinetic parameters under fasting conditions are summarized in TABLE 9.
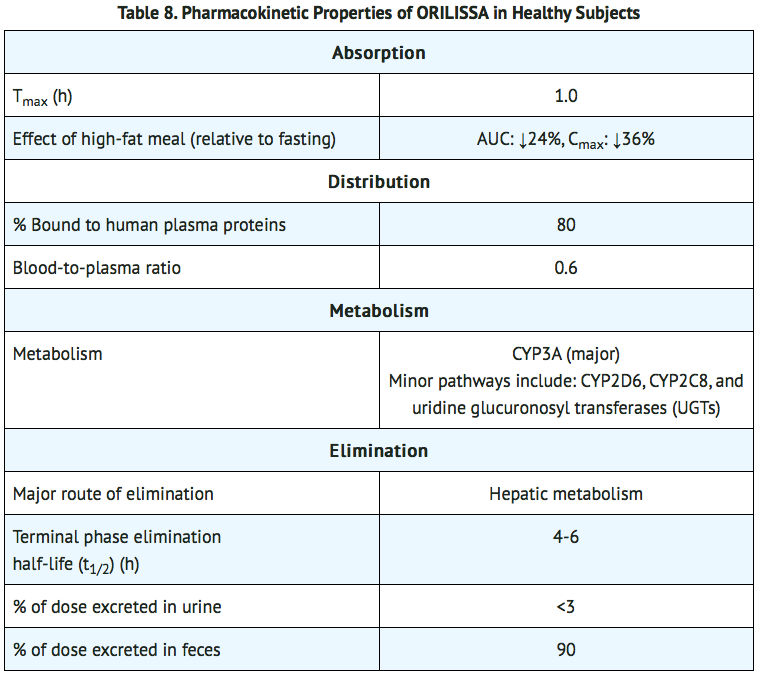
Specific Populations Renal Impairment
- Elagolix exposures (Cmax and AUC) are not altered by renal impairment. The mean exposures are similar for women with moderate to severe or end stage renal disease (including women on dialysis) compared to women with normal renal function.
Hepatic Impairment
- Elagolix exposures (Cmax and AUC) are similar between women with normal hepatic function and women with mild hepatic impairment. Elagolix exposures in women with moderate and severe hepatic impairment are approximately 3-fold and 7-fold, respectively, higher than exposures from women with normal hepatic function.
Race/Ethnicity
- No clinically meaningful difference in the pharmacokinetics of elagolix between White and Black subjects or between Hispanics and others was observed. There is no clinically meaningful difference in the pharmacokinetics of elagolix between Japanese and Han Chinese subjects.
Body weight/Body mass index
- Body weight or body mass index does not affect the pharmacokinetics of elagolix.
Drug Interaction Studies
- Drug interaction studies were performed with elagolix and other drugs that are likely to be co-administered and with drugs commonly used as probes for pharmacokinetic interactions. Tables 10 and 11 summarize the pharmacokinetic effects when elagolix was co-administered with these drugs.
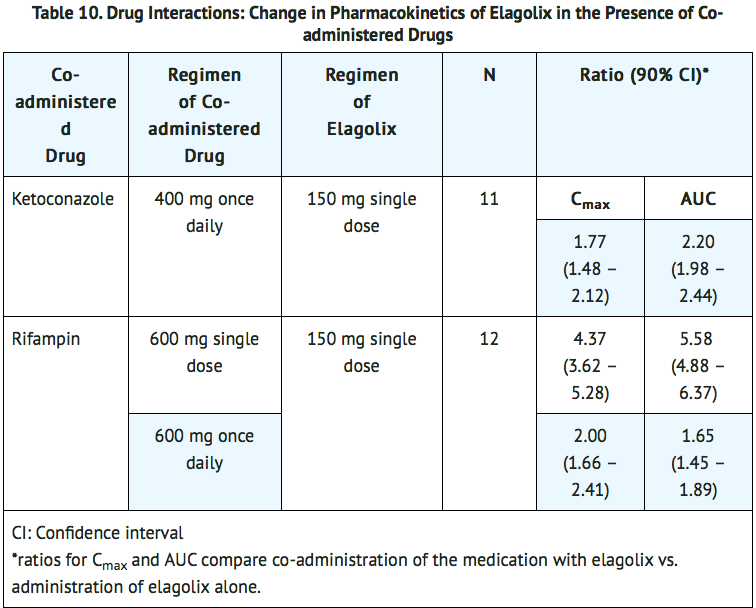
- No clinically significant changes in elagolix exposures were observed when co-administered with rosuvastatin (20 mg once daily), sertraline (25 mg once daily) or fluconazole (200 mg single dose).

- No clinically significant changes in sertraline or fluconazole exposures were observed when co-administered with elagolix.
Pharmacogenomics
- Disposition of elagolix involves the OATP 1B1 transporter protein. Higher plasma concentrations of elagolix have been observed in groups of patients who have two reduced function alleles of the gene that encodes OATP 1B1 (SLCO1B1 521T>C). The frequency of this SLCO1B1 521 C/C genotype is generally less than 5% in most racial/ethnic groups. Subjects with this genotype are expected to have a 78% mean increase in elagolix concentrations compared to subjects with normal transporter function (i.e., SLCO1B1 521T/T genotype).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Two-year carcinogenicity studies conducted in mice (50, 150, or 500 mg/kg/day) and rats (150, 300, or 800 mg/kg/day) that administered elagolix by the dietary route revealed no increase in tumors in mice at up to 19-fold the MRHD based on AUC. In the rat, there was an increase in thyroid (male and female) and liver (males only) tumors at the high dose (12 to 13-fold the MRHD). The rat tumors were likely species-specific and of negligible relevance to humans.
- Elagolix was not genotoxic or mutagenic in a battery of tests, including the in vitro bacterial reverse mutation assay, the in vitro mammalian cell forward mutation assay at the thymidine kinase (TK+/-) locus in L5178Y mouse lymphoma cells, and the in vivo mouse micronucleus assay.
- In a fertility study conducted in the rat, there was no effect of elagolix on fertility at any dose (50, 150, or 300 mg/kg/day). Based on AUC, the exposure multiple for the MRHD in women compared to the highest dose of 300 mg/kg/day in female rats is approximately 5-fold. However, because elagolix has low affinity for the GnRH receptor in the rat, and because effects on fertility are most likely to be mediated via the GnRH receptor, these data have low relevance to humans.
Clinical Studies
- The efficacy of elagolix 150 mg once daily and 200 mg twice daily for the management of moderate to severe pain associated with endometriosis was demonstrated in two multinational double-blind, placebo-controlled trials in 1686 premenopausal women [Study EM-1 (NCT01620528) and Study EM-2 (NCT01931670)]. The median age of women in the trials was 32 years; 88% were White, 9% were Black or African American and 3% were other races. Each placebo-controlled trial assessed the reduction in endometriosis-associated pain over 6 months of treatment.
- Moderate to severe pain associated with endometriosis was required for entry into the trials and was assessed during screening using the composite pelvic signs and symptoms score (CPSSS) and other baseline criteria.
- The CPSSS is based on a modified Biberoglu and Behrman scale with five elements: three responses reported by study subjects (dysmenorrhea, dyspareunia, and non-menstrual pelvic pain) and two findings based on investigator assessment during physical examination (rating of pelvic tenderness and induration). Each element is scored from 0 (absent) to 3 (severe) for a maximum total score of 15. A total score of at least 6, with a score of at least 2 for dysmenorrhea and at least 2 for non-menstrual pelvic pain was required to qualify for randomization. Subjects were also required to have non-menstrual pelvic pain for at least four days in the preceding calendar month, defined as 35 days. Other criteria to determine eligibility for randomization included subject responses in a daily electronic diary (Endometriosis Daily Pain Impact Scale, described below) for both dysmenorrhea and non-menstrual pelvic pain in the 35 days prior to randomization.
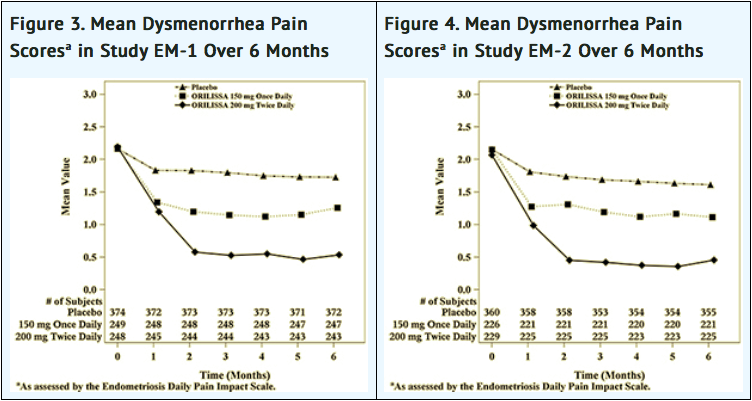
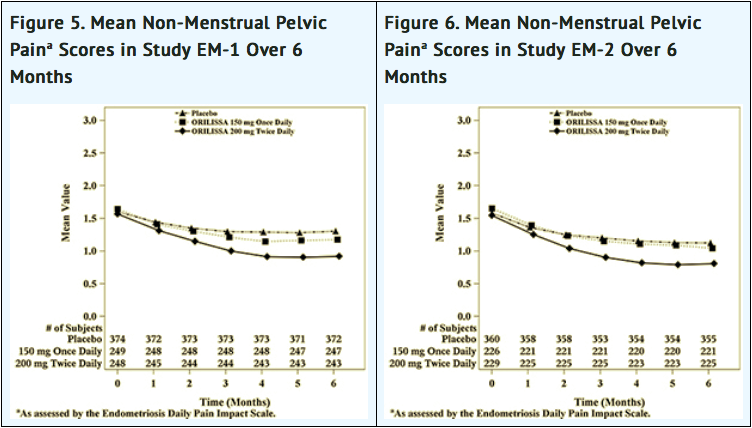
Dysmenorrhea and Non-Menstrual Pelvic Pain
- The co-primary efficacy endpoints were (1) the proportion of subjects whose dysmenorrhea responded to treatment at Month 3 and (2) the proportion of subjects whose pelvic pain not related to menses (also known as non-menstrual pelvic pain) responded to treatment at Month 3. Dysmenorrhea and non-menstrual pelvic pain were evaluated daily using the Endometriosis Daily Pain Impact Scale that asked subjects to rate their pain severity and its impact on daily activities during the prior 24 hours as none, mild, moderate or severe (correlating with a score of 0 to 3, respectively, where higher scores indicated greater severity). Scores at baseline and at each month were averaged over a 35-day interval.
- Women were defined as responders if they experienced a reduction in dysmenorrhea and non-menstrual pelvic pain as defined in Table 12 with no increase in analgesic use (nonsteroidal anti-inflammatory drug or opioid) for endometriosis-associated pain. The threshold for defining responders was based on a receiver operating characteristic (ROC) analysis using the patient global impression of change as an anchor. A higher proportion of women treated with elagolix 150 mg once daily or 200 mg twice daily were responders for dysmenorrhea and non-menstrual pelvic pain compared to placebo in a dose-dependent manner at Month 3 [see TABLE 12].
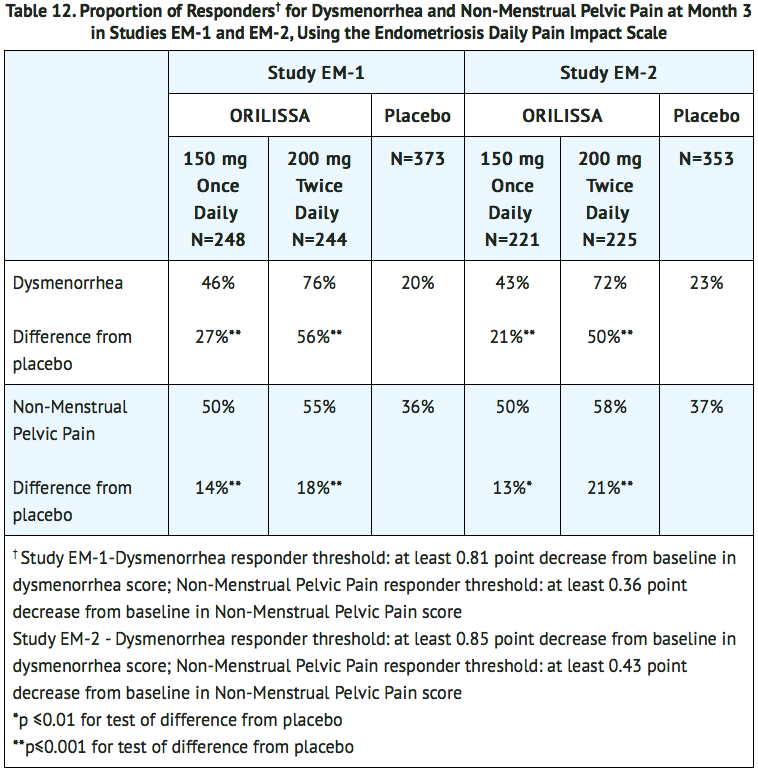
- Women in these studies also provided a daily self-assessment of their endometriosis pain using a numeric rating scale (NRS) that asked subjects to rate their endometriosis pain at its worst over the last 24 hours on a scale from 0 (no pain) to 10 (worst pain ever). In Study EM-1, baseline NRS scores were 5.7 for elagolix 150 mg once daily, 5.5 for elagolix 200 mg twice daily and 5.6 for placebo. In Study EM-2, baseline NRS scores were 5.7 for elagolix 150 mg once daily, 5.3 for elagolix 200 mg twice daily and 5.6 for placebo. Women taking elagolix 150 mg once daily and 200 mg twice daily reported a statistically (p <0.001) significant reduction from baseline in NRS scores compared to placebo at Month 3 in both Studies EM-1 and EM-2 (Study EM-1: 0.7 points for elagolix 150 mg once daily and 1.3 points for elagolix 200 mg twice daily; Study EM-2: 0.6 points for elagolix 150 mg once daily and 1.2 points for elagolix 200 mg twice daily).
- In addition, both elagolix treatment groups showed statistically significantly greater mean decreases from baseline compared to placebo in dysmenorrhea and non-menstrual pelvic pain scores at Month 6. Figures 3 through 6 show the mean scores for dysmenorrhea and non-menstrual pelvic pain over time for Study EM-1 and EM-2.
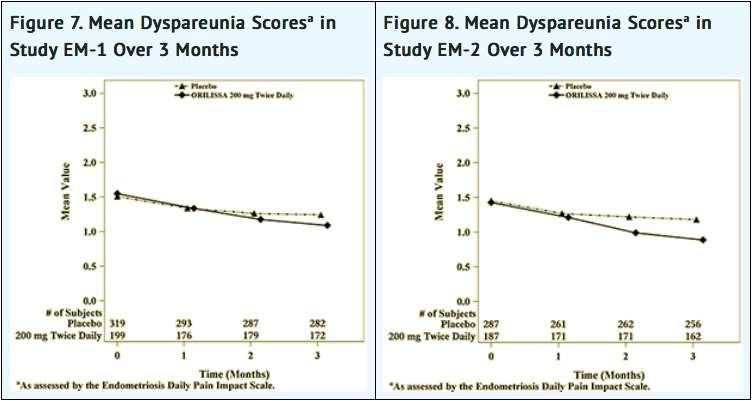
Dyspareunia
- Dyspareunia associated with endometriosis was evaluated as a secondary endpoint using the Endometriosis Daily Pain Impact Scale that asked subjects to rate their pain during sexual intercourse in the prior 24 hours as none, mild, moderate, severe (correlating with a score of 0 to 3, respectively, where higher scores indicated greater severity), or not applicable. In both Studies EM-1 and EM-2, women treated with elagolix 200 mg twice daily showed statistically significantly greater reduction in dyspareunia from baseline to Month 3 than women given placebo (Study EM-1: 0.2; Study EM-2: 0.3). Figures 7 and 8 show the mean scores over time for Study EM-1 and EM-2.
Use of rescue pain medication
- In EM-1 and EM-2, 59% and 60% of patients used an opioid rescue analgesic for pain at baseline. The opioid rescue analgesics used at baseline were predominantly hydrocodone/acetaminophen (HC/APAP) and codeine/APAP at strengths of 5/300-325 mg and 30/300-500 mg. In EM-1, of all patients on an opioid at baseline, 98% and 2% were on HC/APAP and codeine/APAP, respectively. In EM-2, of all patients on an opioid at baseline, 50% were on HC/APAP and 16% were on codeine/APAP.
- Other data related to opioid rescue analgesic use are summarized in TABLE 13.
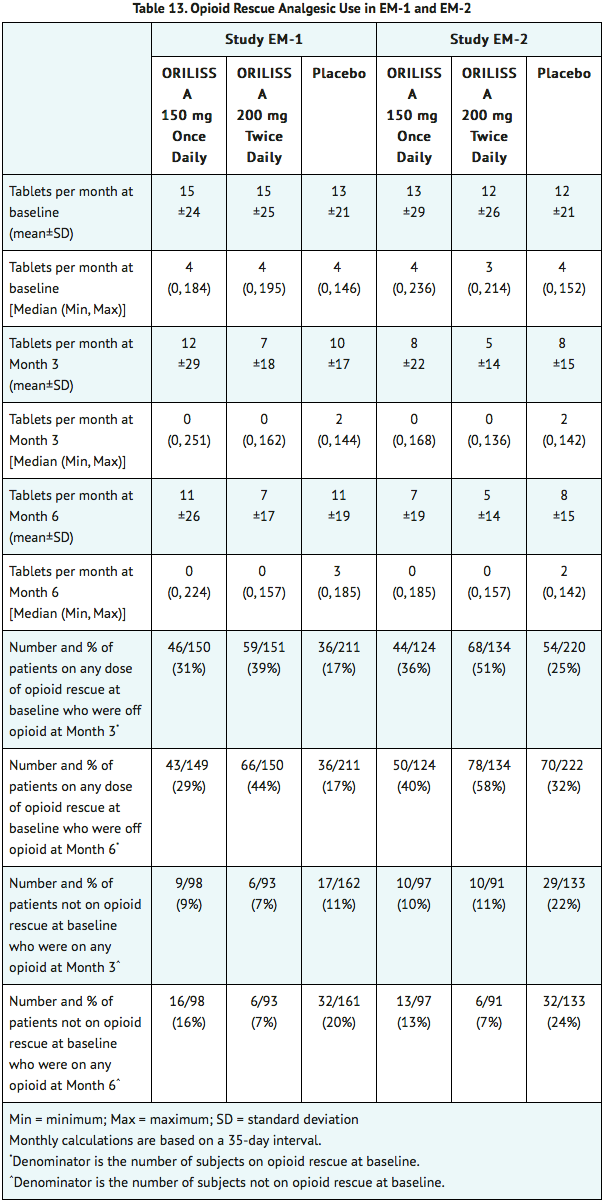
- The clinical relevance of these data has not been demonstrated.
How Supplied
- Elagolix tablets are available in two strengths: 150 mg and 200 mg, which are equivalent to 155.2 mg and 207.0 mg of elagolix sodium, respectively.
- Elagolix 150 mg tablets are light pink, oblong, film-coated tablets with “EL 150” debossed on one side. Elagolix 150 mg tablets are packaged in weekly blister packs. Each blister pack contains 7 tablets supplying the drug product for one week. Four blister packs (a total of 28 tablets) are packaged into a carton that provides the drug product for 4 weeks (NDC 0074-0038-28).
- Elagolix 200 mg tablets are light orange, oblong, film-coated tablets with “EL 200” debossed on one side. The 200 mg tablets are packaged in weekly blister packs. Each blister pack contains 14 tablets supplying the drug product for one week. Four blister packs (a total of 56 tablets) are packaged in a carton that provides the drug product for 4 weeks (NDC 0074-0039-56).
Storage
- Store at 2°C to 30°C (36°F to 86°F).
- Dispose unused medication via a take-back option if available. Otherwise, follow FDA instructions for disposing medication in the household trash, WWW.FDA.GOV/DRUGDISPOSAL. Do NOT flush down the toilet.
Images
Drug Images
{{#ask: Page Name::Elagolix |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Elagolix |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise patients to read the FDA-approved patient labeling (Medication Guide).
- Advise patients on contraceptive options, not to get pregnant while using elagolix, to be mindful that menstrual changes could reflect pregnancy and to discontinue elagolix if pregnancy occurs.
- Inform patients that estrogen containing contraceptives are expected to reduce the efficacy of elagolix.
- Inform patients about the risk of bone loss. Advise adequate intake of calcium and vitamin D.
- Advise patients to seek immediate medical attention for suicidal ideation and behavior. Instruct patients with new onset or worsening depression, anxiety, or other mood changes to promptly seek medical attention.
- Counsel patients on signs and symptoms of liver injury.
- Instruct patients who miss a dose of elagolix to take the missed dose on the same day as soon as she remembers and then resume the regular dosing schedule:
- 150 mg once daily: no more than 1 tablet each day should be taken.
- 200 mg twice daily: no more than 2 tablets each day should be taken.
- Instruct patients to dispose of unused medication via a take-back option if available or to otherwise follow FDA instructions for disposing of medication in the household trash, WWW.FDA.GOV/DRUGDISPOSAL, and not to flush down the toilet.
Medication Guide
Precautions with Alcohol
Alcohol-Elagolix interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Elagolix Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.