Ebola hospital preparedness
|
Ebola Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Postmortem Care |
|
Case Studies |
|
Ebola hospital preparedness On the Web |
|
American Roentgen Ray Society Images of Ebola hospital preparedness |
|
Risk calculators and risk factors for Ebola hospital preparedness |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
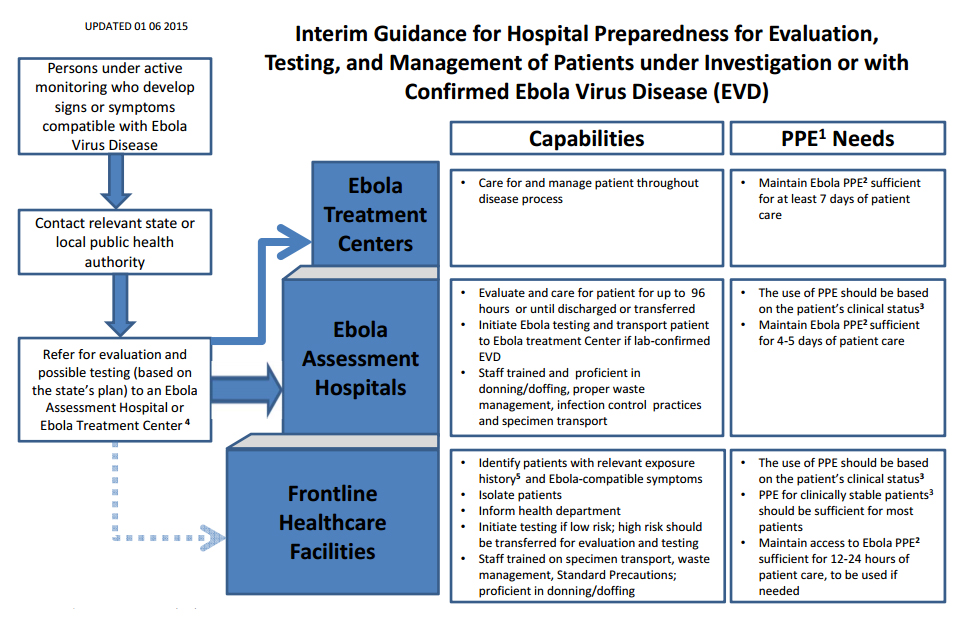
Acute healthcare facilities can serve one of three roles: frontline healthcare facilities, Ebola assessment hospitals, and Ebola treatment centers. To create a coordinated, networked approach, state and local health officials, in collaboration with hospital and healthcare facility executives, may designate healthcare facilities across the state to serve in one of three suggested roles outlined in this guidance document. Whereas a three-tiered approach is not obligatory, it strongly encouraged to identify Ebola assessment hospitals that can successfully manage PUIs until an EVD diagnosis is either confirmed or ruled out while awaiting transfer to an Ebola treatment center.[1]
Guidance for Hospital Preparedness
Frontline Healthcare Facilities
Most U.S. acute care facilities that are equipped for emergency care (such as hospital-based emergency departments and other emergency care settings including urgent care clinics and critical access hospitals) are in this tier. Frontline healthcare facilities do not include primary care offices and other nonemergent ambulatory care settings.
Specifically, frontline healthcare facilities should, in coordination with local and state health authorities, be able to:
- Rapidly identify and triage patients with relevant exposure history AND signs or symptoms compatible with EVD as outlined in CDC’s Emergency Department Evaluation and Management for Patients Under Investigation (PUIs) for Ebola Virus Disease(EVD).
- Immediately isolate any patient with relevant exposure history and signs or symptoms compatible with EVD and take appropriate steps to adequately protect staff caring for the patient, including appropriate use of personal protective equipment (PPE) as outlined in CDC’s Emergency Department Evaluation and Management of Patients Under Investigation (PUIs) for Ebola Virus Disease (EVD).
- Immediately notify the hospital/facility infection control program, other appropriate facility staff, and the state and local public health agencies that a patient has been identified with relevant exposure AND signs or symptoms compatible with EVD; discuss level of risk, clinical and epidemiologic factors, alternative diagnoses, and plan for EVD testing and further care. Patients who are deemed to have low likelihood of EVD on the basis of clinical and epidemiologic factors and have mild illness, but who nonetheless require EVD testing, may, in some circumstances, remain at the frontline healthcare facility while testing is conducted.
- Frontline healthcare facilities, in accordance with the state’s plan, should consider immediately transferring patients who have a higher probability of EVD or are more severely ill to either an Ebola assessment hospital or to an Ebola treatment center that can provide Ebola testing and care for the higher risk patients until an EVD diagnosis is either confirmed or ruled out. The state plan may include plans to transfer the patient out of state based on the patient’s risk and severity of illness and the geographic location of Ebola assessment hospitals and Ebola treatment centers. Such plans should ensure that transport providers are aware of the patient’s status and have appropriate training and PPE to safely transport a patient to a treatment center.[1]
Ebola Assessment Hospitals
Ebola assessment hospitals are facilities prepared to receive and isolate PUIs and care for the patient until a diagnosis of EVD can be confirmed or ruled out and until discharge or transfer is completed. All states, particularly those not planning to designate Ebola treatment centers, should strongly consider identifying Ebola assessment hospitals to ensure that people with symptoms and exposure history consistent with EVD can be cared for until the diagnosis of EVD is confirmed or ruled out. States should consider selecting enough hospitals to provide adequate geographic coverage across the state and avoid extended transport times of more than 1 to 2 hours from areas in which there are large populations of returning travelers, if possible.
Coordinated public health systems are in place to monitor people potentially exposed to EVD (i.e., active and direct active monitoring). Public health authorities may identify people under monitoring who need testing for EVD if they develop compatible signs or symptoms, and may refer them to Ebola assessment hospitals. These people are likely to have been previously identified as at some level of risk for EVD through airport screening and will be actively monitored by public health authorities during the 21 days following travel to an affected country or other potential EVD exposure. Therefore, patients at high risk for EVD should be referred primarily to Ebola assessment hospitals (or treatment centers) rather than frontline healthcare facilities. State and local public health authorities will coordinate closely with facilities when directing patients to a designated Ebola assessment hospital or Ebola treatment center.
- PUIs are likely to present for evaluation with mild symptoms such as isolated fever. Therefore, initial isolation and evaluation of these minimally symptomatic patients can be performed using PPE according to CDC’s Emergency Department Evaluation and Management for Patients Under Investigation (PUIs) for Ebola Virus Disease (EVD).
- In addition, Ebola assessment hospitals should be equipped with PPE needed for clinical care of patients with EVD with more severe symptoms and have staff trained in correct PPE use for PUIs who have vomiting, copious diarrhea, or obvious bleeding,
- Because it may take 72 hours or longer after symptom onset to definitively confirm or rule out an EVD diagnosis (with an additional 12 to 24 hours for specimen transport, testing, and identification of another facility for transfer if needed), Ebola assessment hospitals should be prepared to provide care for PUIs for up to 96 hours. Therefore, Ebola assessment hospitals should have PPE for Ebola sufficient for at least 4 to 5 days of patient care and ensure that staff members involved in or supporting patient care are appropriately trained for their roles. This includes demonstrated proficiency in donning and doffing (putting on and taking off) PPE, proper waste management, infection control practices, and specimen packaging and transport.
- In collaboration with public health officials, Ebola assessment hospitals also should be prepared to coordinate Ebola testing, which may involve transferring specimens to an LRN laboratory capable of EVD testing. Decisions about when to transport to an Ebola treament center a PUI for EVD or patient with confirmed EVD should be informed by discussions among public health authorities and the referring and receiving physicians on a case-by-case basis. When the decision has been made to transport a patient, preparations should ensure that transport providers are aware of the patient’s status and have appropriate training and PPE to safely transport a patient to a treatment center.
- Ensure there is no delay in the care of these patients by being prepared to test, manage, and treat alternative etiologies of febrile illness (e.g., malaria in travelers) as clinically indicated.[1]
Ebola Treatment Centers
Ebola treatment centers are facilities that plan to care for and manage a patient with confirmed EVD for the duration of the patient’s illness. State and local decisions to designate Ebola treatment centers are informed by the results of a CDC site visit conducted by an interdisciplinary team of subject matter experts. Site visits assess the hospitals’ ability to meet the minimum criteria (including infection control capacity, physical infrastructure, staffing resources, PPE supplies, waste management processes, worker safety training, environmental services, and laboratory set up). Staff must be trained in and have practiced putting on and taking off (donning and doffing) PPE for Ebola, as well as providing clinical care using PPE.[1]
References
- ↑ 1.0 1.1 1.2 1.3 "Interim Guidance for U.S. Hospital Preparedness for Patients Under Investigation (PUIs) or with Confirmed Ebola Virus Disease (EVD): A Framework for a Tiered Approach". www.cdc.gov. Centers for Disease Control and Prevention (CDC). February 20 2015. Retrieved March 2 2015. Check date values in:
|accessdate=, |date=(help)