EKG artifacts: Difference between revisions
Kashish Goel (talk | contribs) |
Kashish Goel (talk | contribs) |
||
| Line 101: | Line 101: | ||
** '''"Spike" sign''': Presence of regular or irregular tiny spikes among wide-QRS complexes. | ** '''"Spike" sign''': Presence of regular or irregular tiny spikes among wide-QRS complexes. | ||
** '''"Notch" sign''': Notches superimposed in the wide-QRS-like complex artifact, coinciding with the cycle length when sinus rhythm was recorded. | ** '''"Notch" sign''': Notches superimposed in the wide-QRS-like complex artifact, coinciding with the cycle length when sinus rhythm was recorded. | ||
===Electrode misplacement=== | ===Electrode misplacement=== | ||
Revision as of 18:17, 9 May 2012
|
WikiDoc Resources for EKG artifacts |
|
Articles |
|---|
|
Most recent articles on EKG artifacts Most cited articles on EKG artifacts |
|
Media |
|
Powerpoint slides on EKG artifacts |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on EKG artifacts at Clinical Trials.gov Trial results on EKG artifacts Clinical Trials on EKG artifacts at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on EKG artifacts NICE Guidance on EKG artifacts
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on EKG artifacts Discussion groups on EKG artifacts Patient Handouts on EKG artifacts Directions to Hospitals Treating EKG artifacts Risk calculators and risk factors for EKG artifacts
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for EKG artifacts |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
| Cardiology Network |
 Discuss EKG artifacts further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-in-Chief: Santosh Patel M.D., FRCA [1]; Associate Editor-In-Chief: Kashish Goel, M.D.; Cafer Zorkun, M.D., Ph.D. [2]
Overview
Electrocardiograph (EKG) artifacts are defined as EKG abnormalities, which are a measurement of cardiac potentials on the body surface and are not related to electrical activity of the heart. As a result of artifacts, normal components of the EKG can be distorted. It is very important to recognize these artifacts, otherwise they can lead to unnecessary testing and therapeutic interventions. In this chapter, we will present the common causes and ways to characterize EKG artifacts.
Causes
EKG artifacts can be generated by internal and external causes[1].
Internal
These are physiological causes that could be due to:
- Patient's motion: Does not allow electronic filtration (large swings, usually by epidermal stretching).
- Tremors and shivering cause motion artifacts.
- Simple movements such as brushing and combing the hair can produce EKG disturbances during ambulatory EKG monitoring.
- Muscular activity: Allows electronic filtration (small spikes).[1]
External
These are non-physiological causes associated with other electrical devices attached to or implanted (e.g. deep brain stimulator) in the body and includes the following[1]:
- Electromagnetic interference:
- Power line electrical disturbances/ Light fixtures
- Electrocautery
- Electrical devices in the room
- Radiofrequency based commercial (e.g. mobile phones) products
- Cable and electrode malfunction:
- Insufficient electrode gel
- Misplaced leads
- Inappropriate filter settings
- Broken wires
- Loose connections
- Accumulation of static energy
- Medical equipments: In operation theatres and intensive care unit various equipments can affect EKG monitoring system (e.g. electrodes, leads, amplifier, filters).
| Type of equipment | Artifact |
|---|---|
| IVAC intravenous infusion controller | Atrial or ventricular extrasystoles, pseudowaves (QRS) |
| Cardiopulmonary bypass pump | Uninterpretable tracing, non-specific |
| Pressure-controlled irrigation pump | Atrial flutter |
| COBE Prisma System for continuous venovenous hemofiltration | Atrial flutter |
| Flexible bronchoscope | Atrial fibrillation |
| Deep brain stimulator | Uninterpretable tracing |
| Straight shot microdebrider (nasal endoscopy) | Ventricular tachycardia |
| Intra-aortic balloon pump | Pseudowaves (P), premature atrial contraction |
| Somatosensory evoked potential monitoring units | Supraventricular tachycardia |
| High-frequency oscillatory ventilation | Atrial flutter, atrial fibrillation, ventricular tachycardia |
| Intraoperative high-field MRI | Ventricular tachycardia, ventricular fibrillation, non-specific |
| Transcutaneous electrical nerve stimulator | Spikes, runaway pacemaker, ventricular fibrillation, non-specific |
| Peripheral nerve stimulator | Spikes, loss of pacemaker spikes |
The table includes data from references[2][3]
Identification
Artifacts can distort individual or all components (P, QRS, T waves and PR and ST segments) on the EKG. Most of the time, they are easily identifiable and neglected as they do not resemble any specific pattern. It is important to differentiate these artifactual changes from genuine changes to prevent misdiagnosis. If ST segments are affected by artifacts, either ST segment depression or elevation can occur on the EKG. These changes can be misinterpreted as myocardial ischemia or infarction.
Differentiating an Artifact from Ventricular tachycardia
On occasions, changes may mimic specific arrhythmia like ventricular tachycardia and atrial flutter or fibrillation. It is important to differentiate these, as misdiagnosis can lead to inadvertent use of medications and procedures in such a patient[4][5].
- Characteristics that can help in differentiate an artifact from ventricular tachycardia include[4]:
- Absence of hemodynamic deterioration during the event.
- Normal QRS complexes within the artifact.
- An unstable baseline on the EKG before the event, after the event, or both.
- Association with bodily movement.
- Huang et al[5] also described 3 signs that may help in differentiating a tremor-induced pseudo-ventricular tachycardia from true ventricular tachycardia. Presence of any of these signs is suggestive of pseudo-ventricular tachycardia:
- "Sinus" sign: One of the frontal leads (I, II and III) may present with sinus rhythm showing normal P, QRS, and T waves. The reason is that one of the upper limbs may be free off tremor.
- "Spike" sign: Presence of regular or irregular tiny spikes among wide-QRS complexes.
- "Notch" sign: Notches superimposed in the wide-QRS-like complex artifact, coinciding with the cycle length when sinus rhythm was recorded.
Electrode misplacement
Electrode misplacements are a common artifact that can mimic life-threatening arrhythmias. Early identification and replacement of electrodes can help in avoiding unnecessary therapies. An algorithm has been described previously, which may help in recognizing these artifacts.
REVERSE mnemonic: Approach to EKG artifacts
| EKG findings | Explanation | |
|---|---|---|
| R | R wave is positive in lead aVR (P wave also positive) | Reversal of left arm and right arm electrodes |
| E | Extreme axis deviation: QRS axis between -90 and +180 | Reversal of left arm and right arm electrodes |
| V | Very low (<0.1 mV) voltage in an isolated limb lead | Reversal of right leg and left arm or right arm electrodes |
| E | Exchanged amplitude of P waves (P wave in lead I > lead II) | Reversal of left arm and left leg electrodes |
| R | R wave abnormal progression in precordial lead (pre-dominal R in V1 and S in V6) | Reversal of precordial electrodes (V1 through V6) |
| S | Suspect dextrocardia (negative P waves in lead I) | Reversal of left arm and right arm electrodes |
| E | Eliminate noise and interference (artifact mimicking tachycardias or ST-T changes |
Table adapted from Baranchul et al's work: Crit Care Nurse 2009;29:67-73 doi: 10.4037/ccn2009607
Consequences
Apart from the poor quality of EKG, artifacts can cause serious consequences particularly when they mimic like genuine changes. If EKG artifacts are not recognized by physician, anesthesiologist or intensivist unneccasry diagnostic and therapeutic measures could be taken. Such actions may subject patients to invasive investigations or they may receive unnecessary medications like antiarrythmics.
Correction
Attention to basic principles such as proper electrodes placement and lead connections is required during EKG measurement. Well designed and maintained EKG measurement devices can withstand routine internal or external electrical and motion-related disturbances. However, it is not always possible to eliminate artifacts completely. It is essential that physicians keep high vigilance and interpret EKG keeping EKG artifacts in differential diagnosis list.
Examples of Artifacts
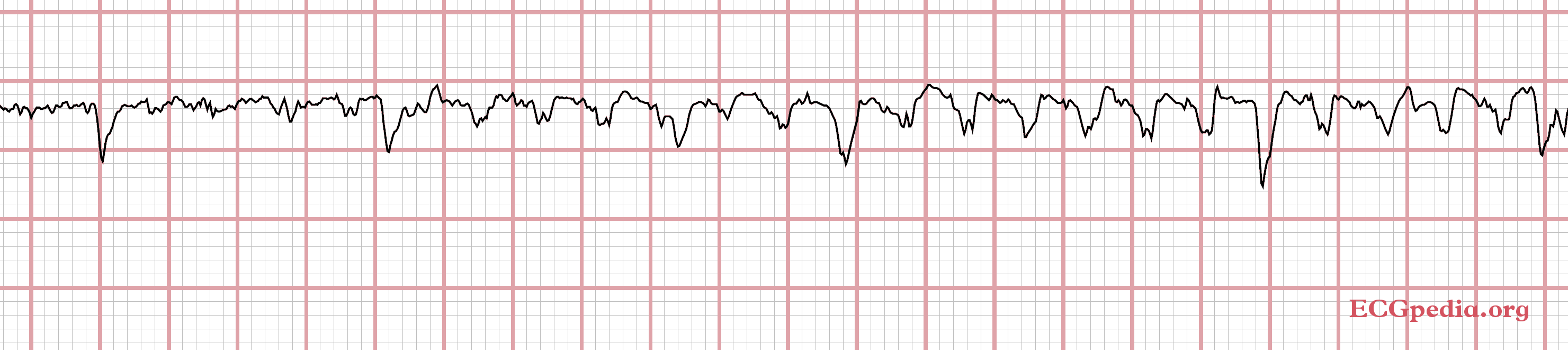
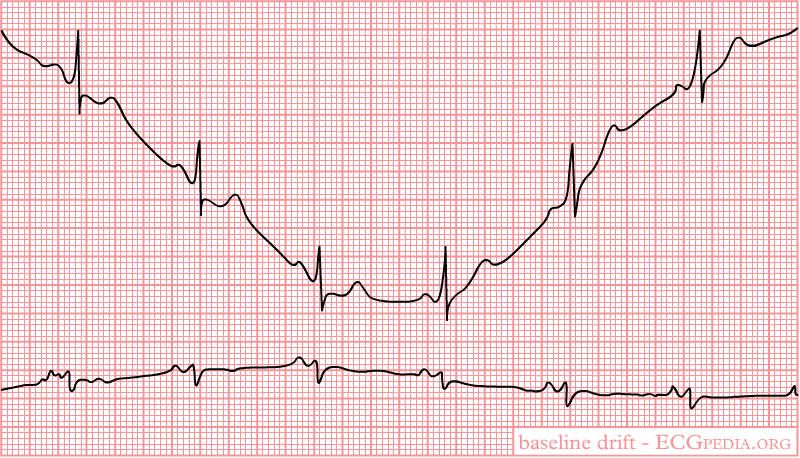
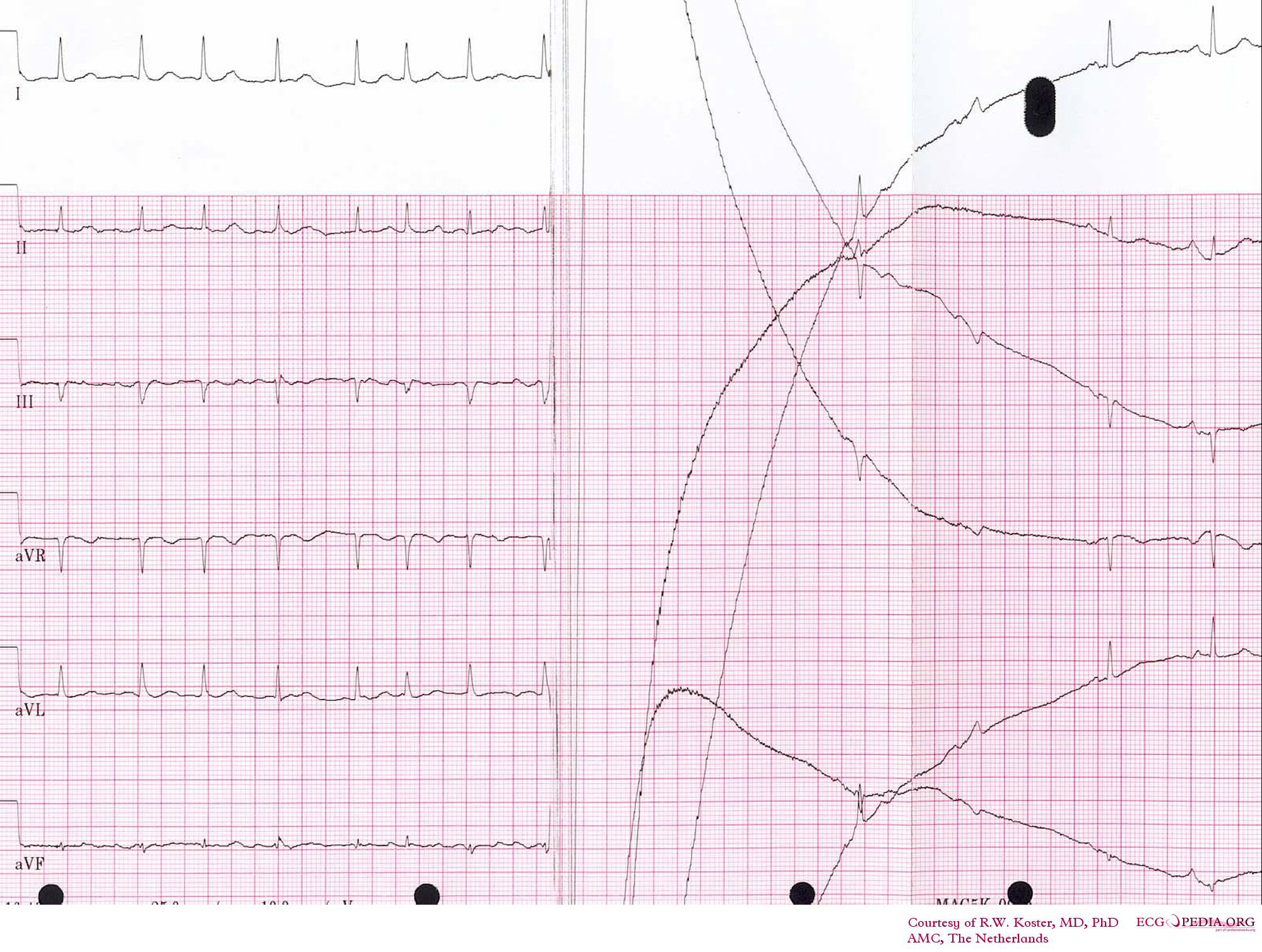
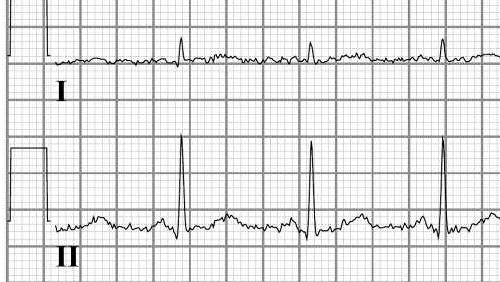
The gallery of images below shows a variety of EKG artifacts that are due to tremor, movement, movement disorders and electrical interference. These artifacts should not be confused with an abnormality in the patient's electrocardiogram. Atrial fibrillation can be confused with these artifacts.
-
Baseline drift. The amplifier in the ECG machine has to re-find the 'mean'. This often occurs right after lead connection and after electric cardioversion.
-
Cardioversion from atrial fibrillation to sinus rhythm, with clear baseline drift.
-
Electrical interference from a nearby electrical appliance. A typical example is a 100 Hz background distortion from fluorescent lights. Not to be confused with atrial fibrillation.
-
Another example of an artifact caused by an electrical appliance. The patients rhythm is regular. This strip shows 10 QRS complexes.
Video explaining ECG artifacts
{{#ev:youtube|LslIvYy2xUU}}
References
- Einthoven W. Le telecardiogramme. Arch Int de Physiol 1906;4:132-164
- Marquez PMID 12177632
- Hurst PMID 9799216
- Kligfield PMID 17322457
- Patel S, Souter M: PMID 18156892
- Patel S: PMID 19344913
- Patel S: PMID 16632773
- Patel S: PMID 19563573
- Patel S, Souter M: PMID 18648245
- Patel S: http://www.springerlink.com/content/w054881370x61802/
- ↑ 1.0 1.1 1.2 Baranchuk A, Shaw C, Alanazi H; et al. (2009). "Electrocardiography pitfalls and artifacts: the 10 commandments". Crit Care Nurse. 29 (1): 67–73. doi:10.4037/ccn2009607. PMID 19182282. Unknown parameter
|month=ignored (help) - ↑ Patel S (2006). "Electrocardiographic artifact mimicking ventricular tachycardia during high-frequency oscillatory ventilation: a case report". Am. J. Crit. Care. 15 (3): 310–1. PMID 16632773. Unknown parameter
|month=ignored (help) - ↑ Patel SI, Souter MJ (2008). "Equipment-related electrocardiographic artifacts: causes, characteristics, consequences, and correction". Anesthesiology. 108 (1): 138–48. doi:10.1097/01.anes.0000296537.62905.25. PMID 18156892. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 Knight BP, Pelosi F, Michaud GF, Strickberger SA, Morady F (1999). "Clinical consequences of electrocardiographic artifact mimicking ventricular tachycardia". N. Engl. J. Med. 341 (17): 1270–4. doi:10.1056/NEJM199910213411704. PMID 10528037. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Huang CY, Shan DE, Lai CH; et al. (2006). "An accurate electrocardiographic algorithm for differentiation of tremor-induced pseudo-ventricular tachycardia and true ventricular tachycardia". Int. J. Cardiol. 111 (1): 163–5. doi:10.1016/j.ijcard.2005.06.017. PMID 16026871. Unknown parameter
|month=ignored (help)