Ductal carcinoma
For patient information, click here
|
WikiDoc Resources for Ductal carcinoma |
|
Articles |
|---|
|
Most recent articles on Ductal carcinoma Most cited articles on Ductal carcinoma |
|
Media |
|
Powerpoint slides on Ductal carcinoma |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Ductal carcinoma at Clinical Trials.gov Trial results on Ductal carcinoma Clinical Trials on Ductal carcinoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Ductal carcinoma NICE Guidance on Ductal carcinoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Ductal carcinoma Discussion groups on Ductal carcinoma Patient Handouts on Ductal carcinoma Directions to Hospitals Treating Ductal carcinoma Risk calculators and risk factors for Ductal carcinoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Ductal carcinoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Maria Fernanda Villarreal, M.D. [2]
Synonyms and keywords: Intraductal hyperplasia; IDH; Atypical ductal hyperplasia; Comedocarcinoma; Duct cell carcinoma; Duct carcinoma
Overview
Ductal carcinoma is the most common type of breast cancer in women. Ductal carcinoma may be classified according to the Armed Forces Institute of Pathology (AFIP) into 2 groups: large cell carcinoma in situ and small cell carcinoma in situ. The pathogenesis of ductal carcinoma is characterized by the microinvasion of cancer cells limited to the ducts with no extension beyond the basement membrane. The mutation on HER2/neu has been associated with the development of ductal carcinoma. The most important cause of ductal carcinoma is mutations in the BRCA1/BRCA2 genes. On microscopic histopathological analysis, characteristic findings of ductal carcinoma, include: equal spacing of cells - "cookie cutter" look, cells line-up along lumen, and nuclear enlargement (key feature). Common risk factors in the development of ductal carcinoma, include: family history of breast cancer, mutations in BRCA1/BRCA2 gene, previous exposure to radiation therapy, increased breast density, and hormonal therapy. Surgical approaches for ductal carcinoma, include: mastectomy or breast-conserving therapy. Lumpectomy in conjunction with adjuvant chemotherapy or radiation is the most common approach to the treatment of ductal carcinoma (with negative margins). On the other hand, mastectomy is recommended for patients with extensive margins of ductal carcinoma. Effective measures for the secondary prevention of ductal carcinoma include: screening mammography for women between 50-74 years (or earlier if identified risk factors) and periodical breast self-examination (BSE).[1]
Historical Perspective
Ductal carcinoma was first described by MacCarthy in 1893.[2]
Classification
- Ductal carcinoma may be classified according to the Armed Forces Institute of Pathology (AFIP) into 2 groups:[3]
- Large cell
- More aggressive form
- Also referred to as comedocarcinoma
- Small cell
- Less aggressive
- Subtypes include cribriform, micropapillary, papillary, and solid in situ.
- Other variants of ductal carcinoma include, non-DCIS entities.
Pathophysiology
- The pathogenesis of ductal carcinoma is characterized by the microinvasion of cancer cells limited to the ducts with no extension beyond the basement membrane.
- The mutation on HER2/neu has been associated with the development of ductal carcinoma.
- On gross pathology, characteristic findings of ductal carcinoma, include:[3]
- White
- Firm stellate lesion
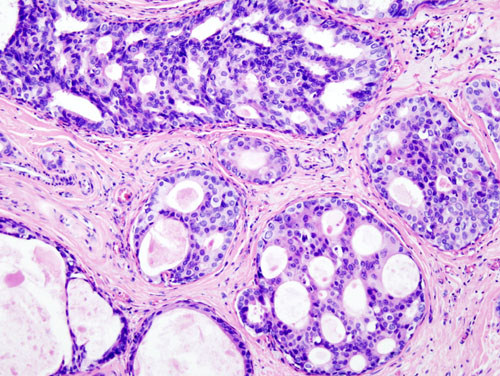
- On microscopic histopathological analysis, characteristic findings of ductal carcinoma, include:
- Equal spacing of cells - "cookie cutter" look.
- Cells line-up along lumen/glandular spaces - form "Roman briges".
- Nuclear enlargement (key feature)
- The image below demonstrates histopathological findings of ductal carcinoma.
-
Ductal carcinoma: cells line-up along lumen (form "Roman briges")
Causes
- The most important cause of ductal carcinoma is mutations in the BRCA1/BRCA2 genes.
Differentiating ductal carcinoma from other Diseases
- Ductal carcinoma must be differentiated from other diseases that cause nipple discharge, breast skin color change, and palpable mass such as:[4]
Epidemiology and Demographics
- The prevalence of ductal carcinoma is approximately 32.5 per 100,000 women worldwide.[3]
Age
- Ductal carcinoma is commonly observed among females between 40 to 80 years old
- Ductal carcinoma is rarely observed among males between 60 and 70 years of age
- Ductal carcinoma is more commonly observed among postmenopausal women[5]
Gender
- Females are significantly more commonly affected with ductal carcinoma than males.
Race
- There is no racial predilection for ductal carcinoma.
Risk Factors
- Common risk factors in the development of ductal carcinoma, include:[4]
- Family history of breast cancer
- Mutations in BRCA1/BRCA2 genes
- Previous exposure to radiation therapy
- Increased breast density
- Hormonal therapy
- Nulliparity
- Genetic syndromes (eg. Li-Fraumeni, Cowden syndrome)
- Obesity
Natural History, Complications and Prognosis
- The majority of patients with ductal carcinoma remain asymptomatic for years.[3]
- Early clinical features include skin color change or nipple discharge.
- If left untreated, the majority of patients with ductal carcinoma may progress to develop lymph node invasion, and metastasis.
- The most common complication of ductal carcinoma is lymphedema.
- Prognosis generally depends on the histological subtype.[4]
Diagnosis
Symptoms
- Ductal carcinoma is usually asymptomatic.
- Symptoms of ductal carcinoma may include the following:[5]
-
- Skin color changes
- Warm and thickened
- Skin of an orange appearance
- Nipple retraction
Physical Examination
- Patients with ductal carcinoma usually are well-appearing.
- Physical examination may show no specific physical findings.
- In some cases, it may be remarkable for:[5]
- Palpable mass
Laboratory Findings
- Laboratory findings consistent with the diagnosis of ductal carcinoma, include:[3]
- Positive/negative estrogen receptor (ER) and progesterone receptor (PR) expression
Imaging Findings
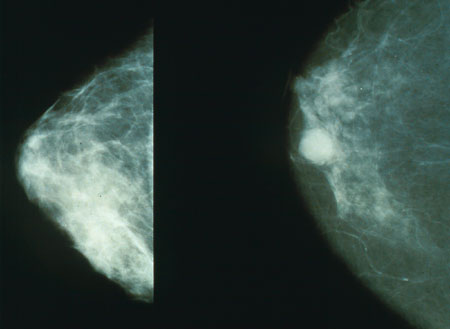
- Mammography is the imaging modality of choice for ductal carcinoma.[4]
- On mammography, findings of ductal carcinoma, include:[4][5]
- Calcifications (most common)
- Simple mass
- Soft-tissue opacity
- Asymmetry without calcification
- The image below demonstrates findings compatible with ductal carcinoma.
-
Normal (left) versus cancerous (right) mammography image.
- On ultrasound, findings of ductal carcinoma, include:[5]
- Microlobulated mild hypoechoic mass
Other Diagnostic Studies
- Ductal carcinoma may also be diagnosed using biopsy.
- Indications for biopsy, include:
- Lesion limited to one quadrant or section of the breast
Treatment
Medical Therapy
- The mainstay of therapies for ductal carcinoma are divided into 2 groups: hormonal therapy and targeted therapy.[3]
Hormonal Therapy
- Selective estrogen receptor modulators, such as:
- Tamoxifen
- Raloxifene
Targeted Therapy
- HER2-directed therapy
- Trastuzumab
- The primary goal of medical therapy is to reduce the risk of ipsilateral or contralateral breast invasion and also decreases the risk of recurrence.[3]
Surgery
- Surgery is the mainstay of therapy for ductal carcinoma.[5]
- Surgical approaches for ductal carcinoma, include: mastectomy or breast-conserving therapy
- Lumpectomy in conjunction with adjuvant chemotherapy or radiation is the most common approach to the treatment of ductal carcinoma (with negative margins)
- Mastectomy is recommended for patients with extensive margins of ductal carcinoma.
Prevention
- Effective measures for the secondary prevention of ductal carcinoma include: screening mammography for women between 50-74 years (or earlier if identified risk factors) and periodical breast self-examination (BSE).[1][5]
- Once diagnosed and successfully treated, patients with ductal carcinoma are followed-up every 3, 6, or 12 months depending on individual assessment.[5]
References
- ↑ 1.0 1.1 US Task Preventive Force. http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening Accessed on April 19, 2016
- ↑ MacCarty WC. The histogenesis of cancer (carcinoma) of the breast and its clinical significance. Surg Gynecol Obstet 1913;17:441–59.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Virnig BA, Tuttle TM, Shamliyan T, Kane RL (2010). "Ductal carcinoma in situ of the breast: a systematic review of incidence, treatment, and outcomes". J. Natl. Cancer Inst. 102 (3): 170–8. doi:10.1093/jnci/djp482. PMID 20071685.
- ↑ 4.0 4.1 4.2 4.3 4.4 Erbas B, Provenzano E, Armes J, Gertig D (2006). "The natural history of ductal carcinoma in situ of the breast: a review". Breast Cancer Res. Treat. 97 (2): 135–44. doi:10.1007/s10549-005-9101-z. PMID 16319971.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 Ductal Carcinoma. Frank Galliard. Radiopedia http://radiopaedia.org/articles/ductal-carcinoma-in-situ Accessed on April 19, 2016