Duchenne muscular dystrophy
For patient information, click here
| Duchenne muscular dystrophy | |
 | |
|---|---|
| ICD-10 | G71.0 |
| ICD-9 | 359.1 |
| OMIM | 310200 |
| DiseasesDB | 3985 |
| MeSH | D020388 |

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Duchenne muscular dystrophy (DMD) (also known as muscular dystrophy - Duchenne type) is an eventually fatal disorder that is characterized by rapidly progressive muscle weakness and atrophy of muscle tissue. DMD is the most common form of muscular dystrophy. There is no available cure at this time.
DMD affects young males due to its X-linked recessive inheritance pattern. Onset of symptoms usually occurs before the sixth year of life and begins with loss of endurance and strength in the legs and pelvis, eventually progressing to include the musculature within the entire body.
Two-thirds of DMD incidences are inherited from the mother, while the remaining one-third are caused by mutations in the genes of the egg or embryo.
DMD is named after the French neurologist Guillaume Benjamin Amand Duchenne (1806-1875), who first described the disease in the 1860s. It is caused by mutations in the gene which encodes dystrophin, an essential cell membrane protein in muscle cells.
Genetics
Duchenne muscular dystrophy is a type of dystrophinopathy which includes a spectrum of muscle disease caused by mutations in the Xp21 gene, which encodes the protein dystrophin. In Duchenne muscular dystrophy, the dystrophin protein is absent. Becker's muscular dystrophy is a milder type of dystrophinopathy where a mutated form of the protein is present. The large size of the gene means it is more prone to mutation, causing DMD to occur spontaneously in many families without a history of the disease.
Duchenne muscular dystrophy is inherited in an X-linked recessive pattern. Male children, who have an XY chromosome pair, receive one of their mother's two X chromosomes and their father's Y chromosome. Women DMD carriers who have an abnormal X chromosome have a one-in-two chance of passing that abnormality on to their male children. Unlike most female children, a male child with an inherited defective Xp21 gene does not have a second X chromosome to provide correct genetic instructions, and the disease manifests.
The sons of carrier females each have a 50% chance of having the disease, and the daughters each have a 50% chance of being carriers. Daughters of men with Duchenne will always be carriers, since they will inherit an affected X chromosome from their father (note that the diagram only shows the results from an unaffected father). Some females will also have very mild degrees of muscular dystrophy, and this is known as being a manifesting carrier. In one-third of the cases, the disease is a result of an unspontaneous or new mutation [2].
Prenatal testing, such as amniocentesis, for pregnancies at risk is possible if the DMD disease-causing mutation has been identified in a family member or if informative linked markers have been identified.
The dystrophin gene contains 24 regions of 109 amino acids that are similar but not exact, making it susceptible to misalignment at the meiotic synapse, which can lead to frameshift mutations and an untranslatable gene. This can happen with a frequency of about 1 in 10,000.
In some female cases, DMD is caused by skewed X inactivation. In these cases, two copies of the X chromosome exist, but for reasons currently unknown, the flawed X chromosome manifests instead of the unflawed copy. In these cases, a mosaic form of DMD is seen, in which some muscle cells are completely normal while others exhibit classic DMD findings. The effects of a mosaic form of DMD on long-term outlook is not known.
Patho-mechanism
Duchenne muscular dystrophy is caused by a mutation of the dystrophin gene whose protein product is responsible for the connection of muscle fibres to the extracellular matrix through a protein complex containing many subunits. The absence of dystrophin permits excess calcium to penetrate the sarcolemma (cell membrane). In a complex cascading process involving several pathways, the excess calcium causes the creation of more reactive oxygen species than the cell's oxide-scavenging enzymes can effectively process. This creates oxidative stress within the cell which damages the sarcolemma and allows more entry points for calcium, and ultimately resulting in the death of the cell. Muscle fibres undergo necrosis and are ultimately replaced with adipose and connective tissue.
Symptoms
The main symptom of Duchenne muscular dystrophy is rapidly progressive muscle weakness associated with muscle wasting with the proximal muscles being first affected, especially the pelvis and calf muscles. Muscle weakness also occurs in the arms, neck, and other areas, but not as severely or as early as in the lower half of the body. Symptoms usually appear before age 6 and may appear as early as infancy. Generalized weakness and muscle wasting first affecting the muscles of the hips, pelvic area, thighs and shoulders. Calves are often enlarged. The other physical symptoms are:
- Awkward gait (patients tend to walk on their forefeet, because of an increased calve tonus)
- Frequent falls
- Difficulty with motor skills (running, hopping, jumping)
- Progressive difficulty walking
- Eventual loss of ability to walk (usually by the age of 12)
- Fatigue
- Higher risk of behaviour and learning difficulties and Autism Spectrum Disorders.
- Skeletal deformities (including scoliosis in some cases)
- Muscle deformities
- Pseudohypertrophy of tongue and calf muscles. The enlarged muscle tissue is eventually replaced by fat and connective tissue, hence the term pseudohypertrophy.
- Muscle contractures of heels and legs, rendering them unusable because the muscle fibers shorten and fibrosis occurs in connective tissue
Signs and tests
Muscle wasting begins in the legs and pelvis, then progresses to the muscles of the shoulders and neck, followed by loss of arm muscles and respiratory muscles. Calf muscle enlargement (pseudohypertrophy) is quite obvious. Cardiomyopathy may occur, but the development of congestive heart failure or arrhythmias (irregular heartbeats) is rare.
- A positive Gower's sign reflects the more severe impairment of the lower extremities muscles. The child helps himself to get up with upper extremities: first by rising to stand on his arms and knees, and then "walking" his hands up his legs to stand upright.
- Affected children usually tire more easily and have less overall strength than their peers.
- Creatine kinase (CPK-MM) levels in the bloodstream are extremely high.
- An electromyography (EMG) shows that weakness is caused by destruction of muscle tissue rather than by damage to nerves.
- Genetic testing can reveal genetic errors in the Xp21 gene.
- A muscle biopsy (immunohistochemistry or immunoblotting) or genetic test (blood test) confirms the absence of dystrophin.
Diagnosis
History and Symptoms
- Symptoms usually become manifest around ages 3-5 with abnormal running, walking and jumping.
- Gowers’ sign is usually evident by age 5.
Heart
- The heart is almost always affected by the disease but overt clinical symptoms are uncommon.
Electrocardiogram
- Typical ECG findings include net RS in V1 with deep, narrow Q’s in the precordial leads.
- This stems from focal transmural becrosis and fibrosis of the posterobasal wall.
AHA Scientific Statement: Management of Cardiac Involvement Associated With Neuromuscular Diseases
Cardiac Evaluation in Duchenne Muscular Dystrophy (DMD) and Becker Muscular Dystrophy (BMD)
| Class I |
| "1. All DMD and BMD patients should have an initial cardiac evaluation with examination, ECG, and imaging performed at diagnosis. (Level of Evidence: B) " |
| "2. Asymptomatic DMD/BMD patients with left ventricular dilation or dysfunction or arrhythmia (eg, supraventricular tachycardia, ventricular ectopy) should be reevaluated at least annually. (Level of Evidence: C) " |
| "3. Symptomatic DMD/BMD patients should be reevaluated more frequently than annually, with testing and frequency determined by the provider and clinical status. (Level of Evidence: C) " |
| "4. Female DMD/BMD carriers should undergo cardiac evaluation by examination, ECG, and noninvasive imaging in the second to third decade of life, with follow-up evaluations every 3 to 5 years thereafter. (Level of Evidence: C) " |
| "5. Echocardiography should be routinely used in the screening and follow-up care of DMD/ BMD patients. (Level of Evidence: B) " |
| Class IIa |
| "1. Every-2-year cardiac evaluation by examina- tion, ECG, and noninvasive imaging is rea- sonable in asymptomatic DMD/BMD patients <10 years of age, increasing to annual evalu- ation at 10 years of age. (Level of Evidence: B) " |
| "2. It is reasonable to consider periodic use of advanced tissue imaging modalities (eg, CMR with contrast) in the care of DMD/BMD patients for assessment of cardiac function, particularly in patients with poor acoustic windows or for assessment of myocardial fibrosis. (Level of Evidence: B) " |
| "3. Ambulatory electrocardiographic monitor- ing for patients with DMD/BMD is reasonable every 1 to 3 years, based on age, EF, and clinical assessment. (Level of Evidence: C) " |
| "4. In the absence of an implantable cardio- verter-de brillator (ICD) or other arrhythmia monitoring, at least annual ambulatory electrocardiographic monitoring is reason- able for patents with DMD/BMD with EF <35% or age ≥17 years. (Level of Evidence: B) " |
Laboratory Findings
CPK test
If a physician suspects DMD after examining the boy they will use a CPK (creatine phosphokinase) test to determine if the muscles are damaged. This test measures the amount of CPK in the blood. In DMD patients CPK leaks out of the muscle cell into the bloodstream, so a high level (nearly 50 to 100 times more) confirms that there is muscle damage. Affected individuals may have a value as high as 15,000 to 35,000iu/l (normal = 60iu/l).
DNA test
The dystrophin gene is composed of 79 exons, and DNA testing and analysis can usually identify the specific type of mutation and the exon or exons that are affected. DNA testing confirms the diagnosis in most cases. [3]
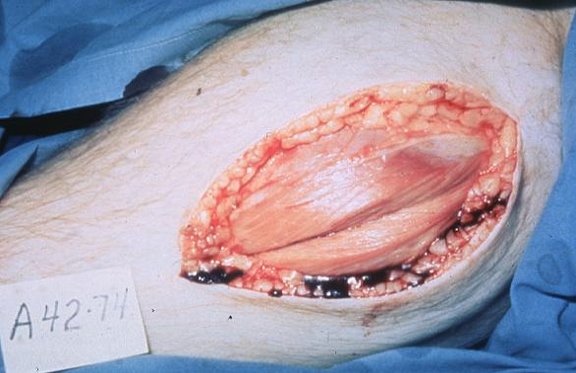
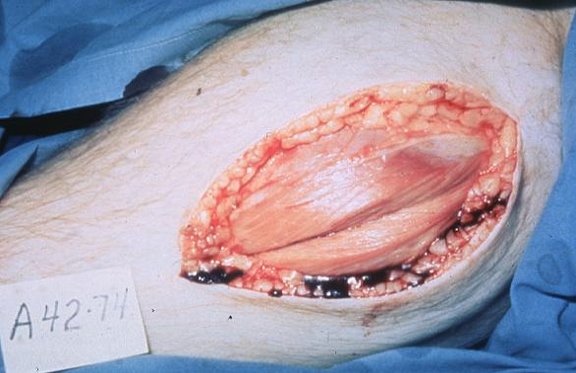
Muscle biopsy
If DNA testing fails to find the mutation, muscle biopsy may be performed. The geneticist may either perform fluorescent labeling or find the amount of dystrophin protein in the blood. In DMD patients there is no fluorescence observed and no protein shown in the column as the patients completely lack dystrophin.
Prenatal tests
If one or both parents are 'carriers' of a particular condition there is a risk that their unborn child will be affected by that condition. 'Prenatal tests' are carried out during pregnancy, to try to find out if the fetus (unborn child) is affected. The tests are only available for some neuromuscular disorders. Different types of prenatal tests can be carried out after about 10 weeks of pregnancy. Chorion villus sampling (CVS) can be done at 10-12 weeks, and amniocentesis at about 14-16 weeks, while placental biopsy and foetal blood sampling can be done at about 18 weeks. Women and/or couples need to consider carefully which test to have and to discuss this with their genetic counselor. Earlier testing would allow early termination which would probably be less traumatic for the couple, but it carries a slightly higher risk of miscarriage than later testing (about 2%, as opposed to 0.5%).
Physical Examination
Appearance of the Patient
Treatment
There is no known cure for Duchenne muscular dystrophy yet although recent stem-cell research is showing some ways to replace damaged muscle tissue. Treatment is aimed at control of symptoms to maximize the quality of life.
- Corticosteroids such as prednisone and deflazacort increase energy and strength and defer severity of some symptoms.
- Mild, non-jarring physical activity such as swimming is encouraged. Inactivity (such as bed rest) can worsen the muscle disease.
- Physical therapy may be helpful to maintain muscle strength and function.
- Orthopedic appliances (such as braces and wheelchairs) may improve mobility and the ability for self-care. Form-fitting removable leg braces that hold the ankle in place during sleep can defer the onset of contractures.
- Appropriate respiratory support as the disease progresses is important
Prognosis
Duchenne muscular dystrophy eventually affects all voluntary muscles and involves the heart and breathing muscles in later stages. Survival is rare beyond the early 30s, [4] although recent advancements in medicine are extending the lives of those afflicted. Death typically occurs from respiratory failure or heart disorders.
Physiotherapy
Physiotherapists are concerned with enabling children to reach their maximum physical potential. Their aim is to:
- minimize the development of contractures and deformity by developing a programme of stretches and exercises where appropriate
- anticipate and minimise other secondary complications of a physical nature
- monitor respiratory function and advise on techniques to assist with breathing exercises and methods of clearing secretions
Mechanical Ventilatory Assistance: Volume Ventilators
Modern "volume ventilators," which deliver a preset volume (amount) of air to the person with each breath, are valuable in the treatment of people with muscular dystrophy related respiratory problems. Ventilator treatment usually begins in childhood when the respiratory muscles begin to fail.
When the vital capacity has dropped below 40 percent of normal, a volume ventilator may be used during sleeping hours, a time when the person is most likely to be underventilating ("hypoventilating"). Hypoventilation during sleep is determined by a thorough history of sleep disorder with an oximetry study and a capillary blood gas (See Pulmonary Function Testing). The ventilator requires a nasal or facemask for connection to the airway. The masks are constructed of comfortable plastic with Velcro straps to hold them in place during sleep.
As the vital capacity declines to less than 30 percent of normal, a volume ventilator may also be needed during the day for more assistance. The person gradually will increase the amount of time using the ventilator during the day as needed. A mouthpiece can be used in the daytime and a nasal or facemask can be used during sleep. The machine can easily fit on a ventilator tray on the bottom of a power wheelchair.
There may be times such as during a respiratory infection when a person needs to rest his/her respiratory muscles during the day even when not yet using full-time ventilation. The versatility of the volume ventilator can meet this need, allowing tired breathing muscles to rest and also allowing aerosol medications to be delivered.
Researching a cure
Promising research is being conducted around the globe to find a cure, or at minimum a therapy that is able to mitigate some of the devastating effects of the disease. Finding a cure is made more complex by the number and variation of genetic mutations in the dystrophin gene that result in DMD.
In the area of stem cell research, a recent paper was published in Nature Cell Biology that describes the identification of pericyte-derived cells from human skeletal muscle. These cells have shown to fulfill important criteria for consideration of therapeutic uses. That is, they are easily accessible in postnatal tissue, they are able to grow to a large enough number in vitro to provide enough cells for systemic treatment of a patient, they have been shown to differentiate into skeletal muscle, and, very importantly, they can reach skeletal muscle through a systemic route. This means that they can be injected arterially and cross through arterial walls into muscle, unlike past hopeful therapeutic cells such as muscle satellite cells which require the impractical task of intramuscular injection. These findings show great potential for stem cell therapy of DMD. In this case a small biopsy of skeletal muscle from the patient would be collected, the pericyte-derived cells would be extracted and grown in culture, and then these cells would be injected into the blood stream where they could navigate into and differentiate into skeletal muscle.
The research group of Kay Davies works on the upregulation of utrophin, a smaller protein, as a substitute for dystrophin.
At the Généthon Institute in Evry near Paris under Olivier Danos and Luis García the U7 gene transfer technique is under development. This new technique is a combination of exon skipping and the transfer of a gene that instructs the muscle cells to continuously produce the antisense oligonucleotides (AONs) themselves so that they do not have to be injected repeatedly. The AONs are potential drugs which are able to modify the genetic information in such a way that the fast progressing Duchenne muscular dystrophy is converted into the much slower developing Becker muscular dystrophy. Early research into the effects of U7 Gene Transfer[5] have been very promising. Treated mice have gone on to show very little muscle weakness even after being stressed. Treated monkeys have retained the active AONs 6 years after injection, and treated dogs have developed 80% of the normal muscle mass within 2 months of treatment. First round tests in humans are due to begin soon, but given the need for multiple rounds of testing before a treatment can be released to the public, it will be at least a few years before this cure is widely available (if indeed these results are possible in humans).
Antisense techniques can also modify splicing of pre-mRNA, similarly converting Duchenne to Becker-like muscular dystrophy in animal models but without the need for insertion of DNA by virus. Because these techniques do not permanently modify the DNA, they are more accurately considered as potential treatments rather than cures. Especially promising for this application are Morpholino antisense oligos [2][3][4]. Morpholinos are commencing Phase 1 clinical trials in the EU (conducted by the MDEX consortium).
More information on the new PTC124 trials, currently nearing the end of Phase II, is available at the MDA.org website. This potential treatment would address from 5 to 15 percent of DMD cases where the dystrophin protein cannot be completed due to an incorrect stop codon in the genetic sequence. The PTC124 treatment skips the improper "stop" instruction, allowing reading through of the remaining sequence and completion of the dystrophin protein assembly process. In recent mouse trials, PTC124 was found to repair damaged muscle tissues. [6] [7]
Recent research shows losartan, a currently available drug used for treating hypertension, to be effective in halting the progress of the disease in mice that were genetically engineered to have Duchenne's. [8] Human trials are in planning.
Parents of children with Duchenne's are noting reductions of symptomatic severity from a regimen of Protandim, a non-prescription nutritional supplement that increases levels of two specific antioxidant enzymes. DMD mouse-model trials of the therapy are in progress, and human trials are planned.[9] [10]
Prevention
Genetic counseling is advised for people with a family history of the disorder. Duchenne muscular dystrophy can be detected with about 95% accuracy by genetic studies performed during pregnancy.
Organizations specific to DMD
In addition to charities devoted to muscular dystrophies in general (such as MDA), these charities are devoted exclusively to DMD:
- Parent Project Muscular Dystrophy: Parent Project Muscular Dystrophy’s mission is to improve the treatment, quality of life and long-term outlook for all individuals affected by Duchenne muscular dystrophy (DMD) through research, advocacy, education and compassion.Parent Project MD's website
- Charley's Fund: an organisation whose mission is to fund research for cure or treatment for Duchenne. Charley's Fund invests money in translational research – research that focuses on moving science from the lab into human clinical trials.
- JettFund (http://www.jettfoundation.org/ , http://www.jettride.org/ ): Currently, 25 teens are biking across America to raise funds for teens with DMD. The recent film Darius Goes West (2007) is a documentary of Darius Weems who suffers from DMD and is taken on a road trip by eleven friends to have MTV "pimp his ride".
- CureDuchenne: is a non-profit organization that aggressively funds leading edge research for treatments and a cure for Duchenne muscular dystrophy. Catchpenny, a band from the mid-west, has written a song for CureDuchenne called "Chance for a Lifetime." Catchpenny performs across the country raising Duchenne awareness. Hear it on CureDuchenne's website
References
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ McClorey G, Moulton H, Iversen P, Fletcher S, Wilton S (2006). "Antisense oligonucleotide-induced exon skipping restores dystrophin expression in vitro in a canine model of DMD". Gene Ther. 13 (19): 1373–1381. PMID 16724091.
- ↑ McClorey G, Fall A, Moulton H, Iversen P, Rasko J, Ryan M, Fletcher S, Wilton S (2006). "Induced dystrophin exon skipping in human muscle explants". Neuromuscul Disord. 16 (9–10): 583–590. PMID 16919955.
- ↑ Fletcher S, Honeyman K, Fall AM, Harding PL, Johnsen RD, Steinhaus JP, Moulton HM, Iversen PL, Wilton SD (2007). "Morpholino Oligomer-Mediated Exon Skipping Averts the Onset of Dystrophic Pathology in the mdx Mouse". Mol Ther. [Epub ahead of print]. PMID 17579573.
Template:Muscular Dystrophy de:Muskeldystrophie it:Distrofia muscolare nl:Ziekte van Duchenne no:Duchenne muskeldystrofi fi:Duchennen lihasdystrofia