Dihydroergotamine (injection)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING
See full prescribing information for complete Boxed Warning.
* Serious and/or life-threatening peripheral ischemia has been associated with the coadministration of DIHYDROERGOTAMINE with potent CYP 3A4 inhibitors including protease inhibitors and macrolide antibiotics. Because CYP 3A4 inhibition elevates the serum levels of DIHYDROERGOTAMINE, the risk for vasospasm leading to cerebral ischemia and/or ischemia of the extremities is increased. Hence, concomitant use of these medications is contraindicated.
|
Overview
Dihydroergotamine (injection) is an anti-migraine that is FDA approved for the treatment of migraine headaches with or without aura and the acute treatment of cluster headache episodes. There is a Black Box Warning for this drug as shown here. Common adverse reactions include vasospasm, paraesthesia, hypertension, dizziness, anxiety, dyspnea, headache, flushing, diarrhea, rash, and pleural and retroperitoneal fibrosis.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP is indicated for the acute treatment of migraine headaches with or without aura and the acute treatment of cluster headache episodes.
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP should be administered in a dose of 1 mL intravenously, intramuscularly or subcutaneously. The dose can be repeated, as needed, at 1 hour intervals to a total dose of 3 mL for intramuscular or subcutaneous delivery or 2 mL for intravenous delivery in a 24 hour period. The total weekly dosage should not exceed 6 mL. D.H.E. 45® (dihydroergotamine mesylate) Injection, USP, should not be used for chronic daily administration.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Dihydroergotamine (injection) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Dihydroergotamine (injection) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Dihydroergotamine (injection) in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Dihydroergotamine (injection) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Dihydroergotamine (injection) in pediatric patients.
Contraindications
- There have been a few reports of serious adverse events associated with the coadministration of dihydroergotamine and potent CYP 3A4 inhibitors, such as protease inhibitors and macrolide antibiotics, resulting in vasospasm that led to cerebral ischemia and/or ischemia of the extremities.
- The use of potent CYP 3A4 inhibitors (ritonavir, nelfinavir, indinavir, erythromycin, clarithromycin, troleandomycin, ketoconazole, itraconazole) with dihydroergotamine is, therefore contraindicated.
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP should not be given to patients with ischemic heart disease (angina pectoris, history of myocardial infarction, or documented silent ischemia) or to patients who have clinical symptoms or findings consistent with coronary artery vasospasm including Prinzmetal’s variant angina.
- Because D.H.E. 45® (dihydroergotamine mesylate) Injection, USP may increase blood pressure, it should not be given to patients with uncontrolled hypertension.
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP, 5-HT1 agonists (e.g., sumatriptan), ergotamine-containing or ergot-type medications or methysergide should not be used within 24 hours of each other.
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP should not be administered to patients with hemiplegic or basilar migraine.
- In addition to those conditions mentioned above, D.H.E. 45® (dihydroergotamine mesylate) Injection, USP is also contraindicated in patients with known peripheral arterial disease, sepsis, following vascular surgery and severely impaired hepatic or renal function.
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP may cause fetal harm when administered to a pregnant woman. Dihydroergotamine possesses oxytocic properties and, therefore, should not be administered during pregnancy. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
- There are no adequate studies of dihydroergotamine in human pregnancy, but developmental toxicity has been demonstrated in experimental animals. In embryo-fetal development studies of dihydroergotamine mesylate nasal spray, intranasal administration to pregnant rats throughout the period of organogenesis resulted in decreased fetal body weights and/or skeletal ossification at doses of 0.16 mg/day (associated with maternal plasma dihydroergotamine exposures [AUC] approximately 0.4-1.2 times the exposures in humans receiving the MRDD of 4 mg) or greater. A no effect level for embryo-fetal toxicity was not established in rats. Delayed skeletal ossification was also noted in rabbit fetuses following intranasal administration of 3.6 mg/day (maternal exposures approximately 7 times human exposures at the MRDD) during organogenesis. A no effect level was seen at 1.2 mg/day (maternal exposures approximately 2.5 times human exposures at the MRDD). When dihydroergotamine mesylate nasal spray was administered intranasally to female rats during pregnancy and lactation, decreased body weights and impaired reproductive function (decreased mating indices) were observed in the offspring at doses of 0.16 mg/day or greater. A no effect level was not established.
- Effects on development occurred at doses below those that produced evidence of significant maternal toxicity in these studies. Dihydroergotamine-induced intrauterine growth retardation has been attributed to reduced uteroplacental blood flow resulting from prolonged vasoconstriction of the uterine vessels and/or increased myometrial tone.
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP is contraindicated in patients who have previously shown hypersensitivity to ergot alkaloids.
- Dihydroergotamine mesylate should not be used by nursing mothers.
- Dihydroergotamine mesylate should not be used with peripheral and central vasoconstrictors because the combination may result in additive or synergistic elevation of blood pressure.
Warnings
|
WARNING
See full prescribing information for complete Boxed Warning.
* Serious and/or life-threatening peripheral ischemia has been associated with the coadministration of DIHYDROERGOTAMINE with potent CYP 3A4 inhibitors including protease inhibitors and macrolide antibiotics. Because CYP 3A4 inhibition elevates the serum levels of DIHYDROERGOTAMINE, the risk for vasospasm leading to cerebral ischemia and/or ischemia of the extremities is increased. Hence, concomitant use of these medications is contraindicated.
|
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP should only be used where a clear diagnosis of migraine headache has been established.
- CYP 3A4 Inhibitors (e.g. Macrolide Antibiotics and Protease Inhibitors)
- There have been rare reports of serious adverse events in connection with the coadministration of dihydroergotamine and potent CYP 3A4 inhibitors, such as protease inhibitors and macrolide antibiotics, resulting in vasospasm that led to cerebral ischemia and/or and ischemia of the extremities.
- The use of potent CYP 3A4 inhibitors with dihydroergotamine should therefore be avoided. Examples of some of the more potent CYP 3A4 inhibitors include: anti-fungals ketoconazole and itraconazole, the protease inhibitors ritonavir, nelfinavir, and indinavir, and macrolide antibiotics erythromycin, clarithromycin, and troleandomycin.
- Other less potent CYP 3A4 inhibitors should be administered with caution. Less potent inhibitors include saquinavir, nefazodone, fluconazole, grapefruit juice, fluoxetine, fluvoxamine, zileuton, and clotrimazole. These lists are not exhaustive, and the prescriber should consider the effects on CYP3A4 of other agents being considered for concomitant use with dihydroergotamine.
Fibrotic Complication
- There have been reports of pleural and retroperitoneal fibrosis in patients following prolonged daily use of injectable dihydroergotamine mesylate. Rarely, prolonged daily use of other ergot alkaloid drugs has been associated with cardiac valvular fibrosis.
- Rare cases have also been reported in association with the use of injectable dihydroergotamine mesylate; however, in those cases, patients also received drugs known to be associated with cardiac valvular fibrosis.
- Administration of D.H.E. 45® (dihydroergotamine mesylate) Injection, USP, should not exceed the dosing guidelines and should not be used for chronic daily administration.
- Risk of Myocardial Ischemia and/or Infarction and Other Adverse Cardiac Events
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP should not be used by patients with documented ischemic or vasospastic coronary artery disease. It is strongly recommended that D.H.E. 45® (dihydroergotamine mesylate) Injection, USP not be given to patients in whom unrecognized coronary artery disease (CAD) is predicted by the presence of risk factors (e.g., hypertension, hypercholesterolemia, smoker, obesity, diabetes, strong family history of CAD females who are surgically or physiologically postmenopausal, or males who are over 40 years of age) unless a cardiovascular evaluation provides satisfactory clinical evidence that the patient is reasonably free of coronary artery and ischemic myocardial disease or other significant underlying cardiovascular disease.
- The sensitivity of cardiac diagnostic procedures to detect cardiovascular disease or predisposition to coronary artery vasospasm is modest, at best. If, during the cardiovascular evaluation, the patient’s medical history or electrocardiographic investigations reveal findings indicative of or consistent with coronary artery vasospasm or myocardial ischemia, D.H.E. 45® (dihydroergotamine mesylate) Injection, USP should not be administered.
- For patients with risk factors predictive of CAD who are determined to have a satisfactory cardiovascular evaluation, it is strongly recommended that administration of the first dose of D.H.E. 45® (dihydroergotamine mesylate) Injection, USP take place in the setting of a physician’s office or similar medically staffed and equipped facility unless the patient has previously received dihydroergotamine mesylate.
- Because cardiac ischemia can occur in the absence of clinical symptoms, consideration should be given to obtaining on the first occasion of use an electrocardiogram (ECG) during the interval immediately following D.H.E. 45® (dihydroergotamine mesylate) Injection, USP, in those patients with risk factors.
- It is recommended that patients who are intermittent long-term users of D.H.E. 45® (dihydroergotamine mesylate) Injection, USP and who have or acquire risk factors predictive of CAD, as described above, undergo periodic interval cardiovascular evaluation as they continue to use D.H.E. 45® (dihydroergotamine mesylate) Injection, USP.
- The systematic approach described above is currently recommended as a method to identify patients in whom D.H.E. 45® (dihydroergotamine mesylate) Injection, USP may be used to treat migraine headaches with an acceptable margin of cardiovascular safety.
Cardiac Events and Fatalities
- The potential for adverse cardiac events exists. Serious adverse cardiac events, including acute myocardial infarction, life-threatening disturbances of cardiac rhythm, and death have been reported to have occurred following the administration of dihydroergotamine mesylate injection.
- Considering the extent of use of dihydroergotamine mesylate in patients with migraine, the incidence of these events is extremely low.
- Drug-Associated Cerebrovascular Events and Fatalities
- Cerebral hemorrhage, subarachnoid hemorrhage, stroke, and other cerebrovascular events have been reported in patients treated with D.H.E. 45® (dihydroergotamine mesylate) Injection, USP; and some have resulted in fatalities. In a number of cases, it appears possible that the cerebrovascular events were primary, the D.H.E. 45® (dihydroergotamine mesylate) Injection, USP having been administered in the incorrect belief that the symptoms experienced were a consequence of migraine, when they were not.
- It should be noted that patients with migraine may be at increased risk of certain cerebrovascular events (e.g., stroke, hemorrhage, transient ischemic attack).
Other Vasospasm Related Events
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP, like other ergot alkaloids, may cause vasospastic reactions other than coronary artery vasospasm. Myocardial, peripheral vascular, and colonic ischemia have been reported with D.H.E. 45® (dihydroergotamine mesylate) Injection, USP.
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP associated vasospastic phenomena may also cause muscle pains, numbness, coldness, pallor, and cyanosis of the digits. In patients with compromised circulation, persistent vasospasm may result in gangrene or death. D.H.E. 45® (dihydroergotamine mesylate) Injection, USP should be discontinued immediately if signs or symptoms of vasoconstriction develop.
Increase In Blood Pressure
- Significant elevation in blood pressure has been reported on rare occasions in patients with and without a history of hypertension treated with dihydroergotamine mesylate injection. D.H.E. 45® (dihydroergotamine mesylate) Injection, USP is contraindicated in patients with uncontrolled hypertension.
- An 18% increase in mean pulmonary artery pressure was seen following dosing with another 5-HT1 agonist in a study evaluating subjects undergoing cardiac catheterization.
Adverse Reactions
Clinical Trials Experience
- Serious cardiac events, including some that have been fatal, have occurred following use of D.H.E. 45® (dihydroergotamine mesylate) Injection, USP, but are extremely rare.
- Events reported have included coronary artery vasospasm, transient myocardial ischemia, myocardial infarction, ventricular tachycardia, and ventricular fibrillation.
- Fibrotic complications have been reported in association with long term use of injectable dihydroergotamine mesylate.
Postmarketing Experience
- The following events derived from postmarketing experience have been occasionally reported in patients receiving D.H.E. 45® (dihydroergotamine mesylate) Injection, USP: vasospasm, paraesthesia, hypertension, dizziness, anxiety, dyspnea, headache, flushing, diarrhea, rash, increased sweating, and pleural and retroperitoneal fibrosis after long-term use of dihydroergotamine.
- Extremely rare cases of myocardial infarction and stroke have been reported. A causal relationship has not been established.
Drug Interactions
There is limited information regarding Dihydroergotamine (injection) Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
- Pregnancy Category
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Dihydroergotamine (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Dihydroergotamine (injection) during labor and delivery.
Nursing Mothers
- Ergot drugs are known to inhibit prolactin. It is likely that D.H.E. 45® (dihydroergotamine mesylate) Injection, USP is excreted in human milk, but there are no data on the concentration of dihydroergotamine in human milk.
- It is known that ergotamine is excreted in breast milk and may cause vomiting, diarrhea, weak pulse, and unstable blood pressure in nursing infants. Because of the potential for these serious adverse events in nursing infants exposed to D.H.E. 45® (dihydroergotamine mesylate) Injection, USP, nursing should not be undertaken with the use of D.H.E. 45® (dihydroergotamine mesylate) Injection, USP.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
There is no FDA guidance on the use of Dihydroergotamine (injection) with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Dihydroergotamine (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Dihydroergotamine (injection) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Dihydroergotamine (injection) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Dihydroergotamine (injection) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Dihydroergotamine (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Dihydroergotamine (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
There is limited information regarding Monitoring of Dihydroergotamine (injection) in the drug label.
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Dihydroergotamine (injection) in the drug label.
Overdosage
- To date, there have been no reports of acute overdosage with this drug. Due to the risk of vascular spasm, exceeding the recommended dosages of D.H.E. 45® (dihydroergotamine mesylate) Injection, USP is to be avoided. Excessive doses of dihydroergotamine may result in peripheral signs and symptoms of ergotism.
- Treatment includes discontinuance of the drug, local application of warmth to the affected area, the administration of vasodilators, and nursing care to prevent tissue damage.
- In general, the symptoms of an acute D.H.E. 45® (dihydroergotamine mesylate) Injection, USP overdose are similar to those of an ergotamine overdose, although there is less pronounced nausea and vomiting with D.H.E. 45® (dihydroergotamine mesylate) Injection, USP. The symptoms of an ergotamine overdose include the following: numbness, tingling, pain, and cyanosis of the extremities associated with diminished or absent peripheral pulses; respiratory depression; an increase and/or decrease in blood pressure, usually in that order; confusion, delirium, convulsions, and coma; and/or some degree of nausea, vomiting, and abdominal pain.
- In laboratory animals, significant lethality occurs when dihydroergotamine is given at I.V. doses of 44 mg/kg in mice, 130 mg/kg in rats, and 37 mg/kg in rabbits.
- Up-to-date information about the treatment of overdosage can often be obtained from a certified Regional Poison Control Center. Telephone numbers of certified Poison Control Centers are listed in the Physician’s Desk Reference® (PDR).*
Pharmacology
Mechanism of Action
- Dihydroergotamine binds with high affinity to 5-HT1Dα and 5-HT1Dβ receptors. It also binds with high affinity to serotonin 5-HT1A, 5-HT2A, and 5-HT2C receptors, noradrenaline α2A, α2B and α, receptors, and dopamine D2L and D3 receptors.
- The therapeutic activity of dihydroergotamine in migraine is generally attributed to the agonist effect at 5-HT1D receptors. Two current theories have been proposed to explain the efficacy of 5-HT1D receptor agonists in migraine. One theory suggests that activation of 5-HT1D receptors located on intracranial blood vessels, including those on arterio-venous anastomoses, leads to vasoconstriction, which correlates with the relief of migraine headache. The alternative hypothesis suggests that activation of 5-HT1D receptors on sensory nerve endings of the trigeminal system results in the inhibition of pro-inflammatory neuropeptide release.
- In addition, dihydroergotamine possesses oxytocic properties.
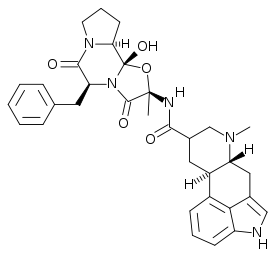
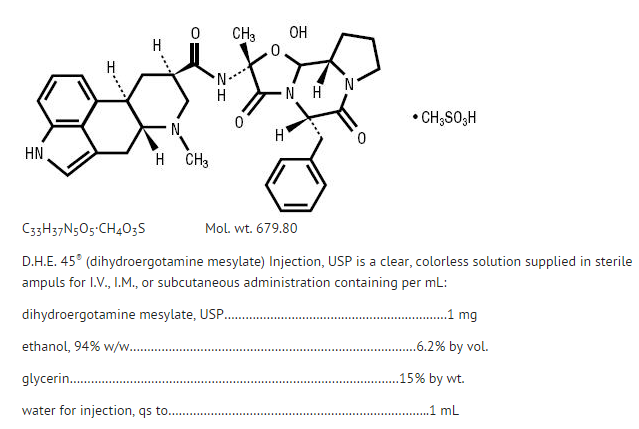
Structure
- D.H.E. 45® is ergotamine hydrogenated in the 9, 10 position as the mesylate salt. D.H.E. 45® is known chemically as ergotaman-3´,6´,18-trione,9,10-dihydro-12´-hydroxy-2´-methyl-5´-(phenylmethyl)-,(5´α)-, monomethanesulfonate. Its molecular weight is 679.80 and its empirical formula is C33H37N5O5·CH4O3S.
The chemical structure is
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Dihydroergotamine (injection) in the drug label.
Pharmacokinetics
Absorption
- Absolute bioavailability for the subcutaneous and intramuscular route have not been determined, however, no difference was observed in dihydroergotamine bioavailability from intramuscular and subcutaneous doses. Dihydroergotamine mesylate is poorly bioavailable following oral administration.
Distribution
- Dihydroergotamine mesylate is 93% plasma protein bound. The apparent steady-state volume of distribution is approximately 800 liters.
Metabolism
- Four dihydroergotamine mesylate metabolites have been identified in human plasma following oral administration. The major metabolite, 8´-β-hydroxydihydroergotamine, exhibits affinity equivalent to its parent for adrenergic and 5-HT receptors and demonstrates equivalent potency in several venoconstrictor activity models, in vivo and in vitro. The other metabolites, i.e., dihydrolysergic acid, dihydrolysergic amide, and a metabolite formed by oxidative opening of the proline ring are of minor importance. Following nasal administration, total metabolites represent only 20%-30% of plasma AUC.
- Quantitative pharmacokinetic characterization of the four metabolites has not been performed
Excretion
- The major excretory route of dihydroergotamine is via the bile in the feces. The total body clearance is 1.5 L/min which reflects mainly hepatic clearance. Only 6%-7% of unchanged dihydroergotamine is excreted in the urine after intramuscular injection. The renal clearance (0.1 L/min) is unaffected by the route of dihydroergotamine administration. The decline of plasma dihydroergotamine after intramuscular or intravenous administration is multi-exponential with a terminal half-life of about 9 hours.
Subpopulations
- No studies have been conducted on the effect of renal or hepatic impairment, gender, race, or ethnicity on dihydroergotamine pharmacokinetics. D.H.E. 45® (dihydroergotamine mesylate) Injection, USP is contraindicated in patients with severely impaired hepatic or renal function.
Interactions
- Pharmacokinetic interactions have been reported in patients treated orally with other ergot alkaloids (e.g., increased levels of ergotamine) and macrolide antibiotics, principally troleandomycin, presumably due to inhibition of cytochrome P450 3A metabolism of the alkaloids by troleandomycin. Dihydroergotamine has also been shown to be an inhibitor of cytochrome P450 3A catalyzed reactions and rare reports of ergotism have been obtained from patients treated with dihydroergotamine and macrolide antibiotics (e.g., troleandomycin, clarithromycin, erythromycin), and in patients treated with dihydroergotamine and protease inhibitors (e.g. ritonavir), presumably due to inhibition of cytochrome P450 3A metabolism of ergotamine.
- No pharmacokinetic interactions involving other cytochrome P450 isoenzymes are known.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Dihydroergotamine (injection) in the drug label.
Clinical Studies
There is limited information regarding Clinical Studies of Dihydroergotamine (injection) in the drug label.
How Supplied
- D.H.E. 45® (dihydroergotamine mesylate) Injection, USP
- Available as a clear, colorless, sterile solution in single 1 mL sterile ampuls containing 1 mg of dihydroergotamine mesylate per mL, in packages of 10 (NDC 0078-0041-01).
Storage
- Store below 25°C (77°F), in light-resistant containers.
- Do not refrigerate or freeze.
- To assure constant potency, protect the ampuls from light and heat. Administer only if clear and colorless.
Images
Drug Images
{{#ask: Page Name::Dihydroergotamine (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
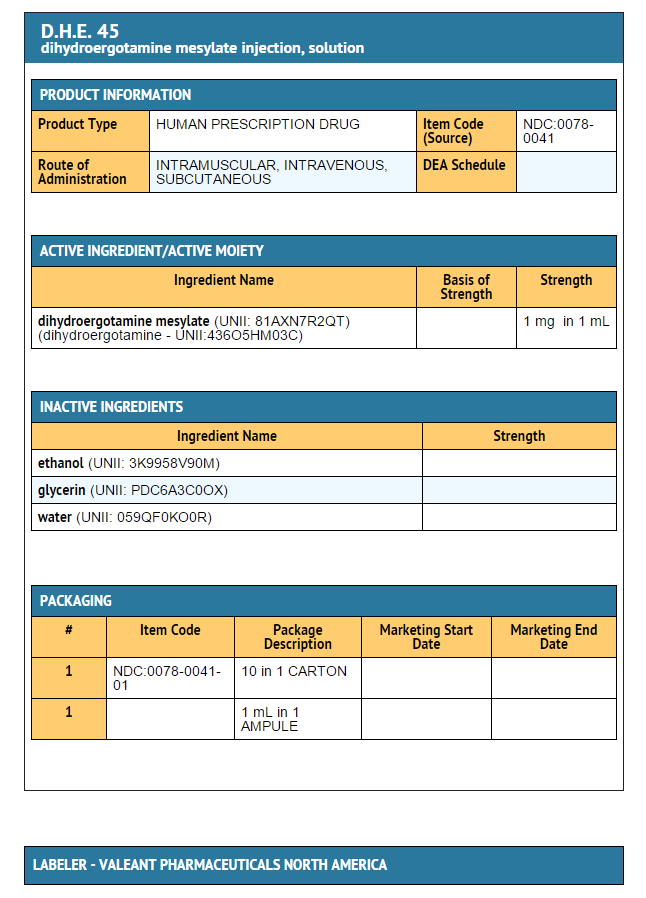
{{#ask: Label Page::Dihydroergotamine (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Dihydroergotamine (injection) in the drug label.
Precautions with Alcohol
- Alcohol-Dihydroergotamine (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- D.H.E. 45 ®[1]
Look-Alike Drug Names
There is limited information regarding Dihydroergotamine (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Dihydroergotamine (injection) |Label Name=DailyMed - D.H.E. 45- dihydroergotamine mesylate injection, solution .png
}}