Diaphragmatic hernia
|
Diaphragmatic hernia Main page |
|
Diagnosis |
|---|
|
Treatment |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Template:DiseaseDisorder infobox
Overview
Diaphragmatic hernia is a congenital anomaly that occurs due to failure of the diaphragm to close leading to herniation of the abdominal content into the thoracic cavity leading to pulmonary hypoplasia. It most commonly presents in the neonates as respiratory distress. It is classified according to the site of herniation into anterior, posterolateral, and hiatal diaphragmatic hernia. It can cause complications in both the GIT and the cardiopulmonary circulation. It can be diagnosed antenatally in the week 24 and after birth, it is apparent on chest x-ray. The mainstay of treatment is surgical correction which must be done when the infant is completely stabilized.
Historical Perspective
- In 1679, the first case of congenital diaphragmatic hernia was reported by Riverius.
- In 1888, the first procedure to repair congenital diaphragmatic hernia in an adult was done and in 1889, the first procedure on an infant was done.
- In 1905, the first successful operation was done but the success rate remained below 60% until 1925.
- In 1940, A set of diagnostic criteria for diaphragmatic hernia were suggested.
- In 1950, the transthoracic approach was suggested instead of the transabdominal approach.
Classification
Congenital diaphragmatic hernia can be classified into three types according to the site of herniation.[1][2]
Posterolateral (Bochdalek) diaphragmatic hernia
- It is the most common subtype.
- Most commonly occurs on the left side and rarely occurs bilaterally.
Anterior (Morgagni) diaphragmatic hernia
- In anterior diaphragmatic hernia, the intestine bulges into the thorax through the anterior midline.
- Most of the cases of anterior diaphragmatic hernia occur on the right side.
Hiatal hernia
- The intestine finds its way to the thorax through the esophageal hiatus.
- More common in the adults than in the neonates.
Pathophysiology
- The herniated viscera decrease the area needed by the lung to develop appropriately.[3]
- According to the degree of herniation, the degree of pulmonary hypoplasia is determined.
- The herniated viscera impairs the development of the bronchial tree.
- As a consequence, the alveoli development is also slowed.[4]
- The development of the pulmonary artery tree is halted too resulting in excessive masculinization of the arteries.
- The increased pulmonary pressure leads to increased pressure on the right ventricle leading to the development of a right to left shunt.
- The development of the pulmonary artery tree is halted too resulting in excessive masculinization of the arteries.
- As most of the cases of diaphragmatic hernia are unilateral, the pulmonary hypoplasia is also usually unilateral, but it can be bilateral if the mediastinum is pushed by a massive unilateral hernia.
- The abnormal alveolar development can lead to hypoxemia leading to pulmonary vasoconstriction which aggravates the condition.
Risk factors
Risk factors of diaphragmatic hernia include:[5]
- Male gender
- Premature birth
- Macrosomia
- Low birth weight
Differentiating Diaphragmatic hernia from other Diseases
Epidemiology
Incidence
- The incidence of congenital diaphragmatic hernia ranges from 50-150 per 100.000 live births.[6]
Prevalence
- The prevalence of congenital diaphragmatic hernia ranges from 10 to 40 per live births.[7]
Sex
- Congenital diaphragmatic hernia has no sex predilection.[7]
Age
- 90% of the congenital diaphragmatic hernias present in the neonatal period.
Screening
According to USPSTF, there is no screening recommended for diaphragmatic hernia.
Natural history, complications and prognosis
Natural history
- 90% of the cases of congenital diaphragmatic hernia presents in the neonatal period.
- If left untreated, congenital diaphragmatic hernia can be fatal due to pulmonary hypoplasia and severe pulmonary hypertension.
Complications
GI complications[8]
- Abnormal developmental rotation of the midgut
- Midgut volvulus
- Gastric volvulus
Cardiopulmonary complications[8]
- Pulmonary hypoplasia
- Pulmonary artery hypertension
- In severe cases, ventricular hypoplasia
Prognosis
- The prognosis is mainly dependent on the size of the defect and the degree of the herniation.[9]
- The presence or absence of liver herniation on fetal MRI is the most reliable prediction of the postnatal survival.
- The estimation of fetal lung volume and lung area to head circumference is a useful indicator of the prognosis of the disease in the absence of liver herniation.
- The mortality ranges from 25-60% of the cases.
History and Symptoms
CDH most often presents in the neonatal period as:[10]
- Cyanosis
- Rapid breathing (tachypnea)
- Shortness of breath (dyspnea)
- Increased work of breathing (labored breathing)[11]
- Lethargy
- Intolerance to feeding due to inadequate oxygenation.
- Adrenal insufficiency: it is a common association with congenital diaphragmatic hernia.
{{#ev:youtube|jPpGHVkB54A}}
Physical Examination
General appearance
- A neonate with CDH usually appears cyanotic and in acute distress.[12]
Vital signs
- Heart rate: tachycardia
- Respiratory rate: tachypnea
- Blood pressure: The infant may have hypotension due to compression of the ventricles
Lungs
- The chest may have a barrel shape.
- Absent breath sounds at the side of the hernia[13]
- Peristaltic sounds in the chest
Heart
- The heart sounds may be displaced to the other side of the chest.
- The heart sounds may reveal the murmurs of associated cardiac anomalies.
Abdomen
- The abdomen is scaphoid due to herniation of the abdominal content into the thoracic cavity.
Laboratory Findings
Antenatal tests
- Amniocentesis: karyotype should be obtained to rule out associated chromosomal abnormalities.
- Maternal alpha-fetoprotein is decreased in CDH[14]
Postnatal tests
- Arterial blood gas: ABG may show hypoxemia, metabolic acidosis, and hypercapnia.
- The infant should be investigated for the presence of associated chromosomal abnormalities.[15]
Radiological tests
Antenatal ultrasound
- CDH can be diagnosed in the 24th week.[16]
- In addition to the hernia, ultrasound can show polyhydramnios and absence of the gastric air bubble
- Left sided CDH is far more common than right sided CDH, while bilateral CDH is rare.
- The presence of liver herniation is associated with worse prognosis and survival.
- The estimation of lung area to head circumference ratio can give an idea about the prognosis (especially if there is no liver herniation). The lower the ratio, the worse the prognosis.

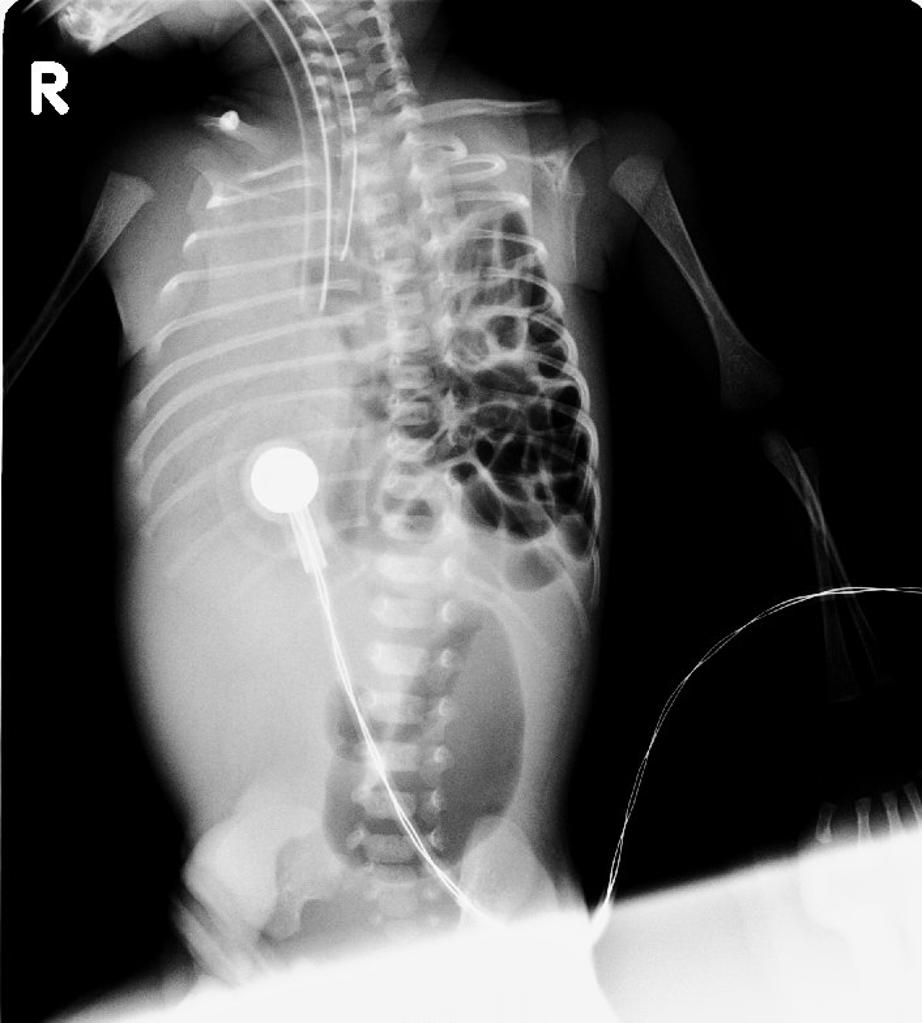
Chest x-ray
- Bowel loops in the thoracic cavity (can be further demonstrated through placement of a feeding tube)
- Shifting of the mediastinum to the contralateral side
Echocardiography
- Echocardiography must be done to exclude associated cardiac anomalies and to exclude the presence of an associated ventricular strain from the pressure.
Medical treatment
Antenatal glucocorticoids
Antenatal glucocorticoids improve the survival by increasing the secretion of surfactant and thus stimulating lung maturation and preventing severe pulmonary hypoplasia.[1]
Preoperative stabilization
- Preoperative stabilization of the patient is important as performing the operation in an unstable infant is associated with higher morbidity and mortality rates.
- Preoperative stabilization measures include:[17]
- Mechanical ventilation: The aim is to ensure proper oxygenation without causing any barotrauma to the lung. Peak inspiratory pressure should be always less than 30 cm H2O
- Nasogastric tube insertion: The aim is to decompress the bowel and to give more space for the lung
- Blood pressure support: using vasopressors or isotonic fluid: The aim is to keep the mean blood pressure above 50 mmHg.[17]
- High-frequency oscillatory ventilation: It is useful in improving the oxygenation without increasing the pressure in the airways or the alveoli.
- Extracorporeal membrane oxygenation: It is used as the last resort in patients resistant to all the conventional methods of ventilation.
- Inhaled nitric oxide: The hypoxemia resulting from lung compression can cause hypoxemia that may result in pulmonary vasoconstriction and hypertension.
Surgical treatment
- The procedure must not be done unless the infant is stable.[18]
- Most of the operations are done through a subcostal incision.
- The repair can be done in one of two ways depending on its size:[9]
- Primary closure: it involves repairing the defect using non-absorbable sutures. It is used if the defect is relatively small.
- Patch closure: using a prosthetic or fascial patch to close the defect. It is useful especially with large defects but increases the risk of infection.
- Endoscopic procedures through the thorax or the abdomen have been reported to have lower mortality rates but have higher recurrence rates.[12]
- If CDH repair is associated with an abdominal wall defect, silo closure may be tried temporarily until the CDH is stabilized.[19]
Refrences
- ↑ 1.0 1.1 Badillo A, Gingalewski C (2014). "Congenital diaphragmatic hernia: treatment and outcomes". Semin. Perinatol. 38 (2): 92–6. doi:10.1053/j.semperi.2013.11.005. PMID 24580764.
- ↑ Schumacher L, Gilbert S (2009). "Congenital diaphragmatic hernia in the adult". Thorac Surg Clin. 19 (4): 469–72. doi:10.1016/j.thorsurg.2009.08.004. PMID 20112629.
- ↑ Langham MR, Kays DW, Ledbetter DJ, Frentzen B, Sanford LL, Richards DS (1996). "Congenital diaphragmatic hernia. Epidemiology and outcome". Clin Perinatol. 23 (4): 671–88. PMID 8982563.
- ↑ Keijzer R, Puri P (2010). "Congenital diaphragmatic hernia". Semin. Pediatr. Surg. 19 (3): 180–5. doi:10.1053/j.sempedsurg.2010.03.001. PMID 20610190.
- ↑ Cullen ML, Klein MD, Philippart AI (1985). "Congenital diaphragmatic hernia". Surg. Clin. North Am. 65 (5): 1115–38. PMID 3904042.
- ↑ Fisher JC, Haley MJ, Ruiz-Elizalde A, Stolar CJ, Arkovitz MS (2009). "Multivariate model for predicting recurrence in congenital diaphragmatic hernia". J. Pediatr. Surg. 44 (6): 1173–9, discussion 1179–80. doi:10.1016/j.jpedsurg.2009.02.043. PMC 3072822. PMID 19524735.
- ↑ 7.0 7.1 McGivern MR, Best KE, Rankin J, Wellesley D, Greenlees R, Addor MC, Arriola L, de Walle H, Barisic I, Beres J, Bianchi F, Calzolari E, Doray B, Draper ES, Garne E, Gatt M, Haeusler M, Khoshnood B, Klungsoyr K, Latos-Bielenska A, O'Mahony M, Braz P, McDonnell B, Mullaney C, Nelen V, Queisser-Luft A, Randrianaivo H, Rissmann A, Rounding C, Sipek A, Thompson R, Tucker D, Wertelecki W, Martos C (2015). "Epidemiology of congenital diaphragmatic hernia in Europe: a register-based study". Arch. Dis. Child. Fetal Neonatal Ed. 100 (2): F137–44. doi:10.1136/archdischild-2014-306174. PMID 25411443.
- ↑ 8.0 8.1 Tovar JA (2012). "Congenital diaphragmatic hernia". Orphanet J Rare Dis. 7: 1. doi:10.1186/1750-1172-7-1. PMC 3261088. PMID 22214468.
- ↑ 9.0 9.1 Chandrasekharan PK, Rawat M, Madappa R, Rothstein DH, Lakshminrusimha S (2017). "Congenital Diaphragmatic hernia - a review". Matern Health Neonatol Perinatol. 3: 6. doi:10.1186/s40748-017-0045-1. PMC 5356475. PMID 28331629.
- ↑ Kotecha S, Barbato A, Bush A, Claus F, Davenport M, Delacourt C, Deprest J, Eber E, Frenckner B, Greenough A, Nicholson AG, Antón-Pacheco JL, Midulla F (2012). "Congenital diaphragmatic hernia". Eur. Respir. J. 39 (4): 820–9. doi:10.1183/09031936.00066511. PMID 22034651.
- ↑ Peetsold MG, Kneepkens CM, Heij HA, IJsselstijn H, Tibboel D, Gemke RJ (2010). "Congenital diaphragmatic hernia: long-term risk of gastroesophageal reflux disease". J. Pediatr. Gastroenterol. Nutr. 51 (4): 448–53. doi:10.1097/MPG.0b013e3181d1b149. PMID 20512059.
- ↑ 12.0 12.1 Haroon J, Chamberlain RS (2013). "An evidence-based review of the current treatment of congenital diaphragmatic hernia". Clin Pediatr (Phila). 52 (2): 115–24. doi:10.1177/0009922812472249. PMID 23378478.
- ↑ Lund DP, Mitchell J, Kharasch V, Quigley S, Kuehn M, Wilson JM (1994). "Congenital diaphragmatic hernia: the hidden morbidity". J. Pediatr. Surg. 29 (2): 258–62, discussion 262–4. PMID 8176602.
- ↑ McHoney M (2015). "Congenital diaphragmatic hernia, management in the newborn". Pediatr. Surg. Int. 31 (11): 1005–13. doi:10.1007/s00383-015-3794-9. PMID 26403792.
- ↑ Lally KP, Paranka MS, Roden J, Georgeson KE, Wilson JM, Lillehei CW, Breaux CW, Poon M, Clark RH, Atkinson JB (1992). "Congenital diaphragmatic hernia. Stabilization and repair on ECMO". Ann. Surg. 216 (5): 569–73. PMC 1242675. PMID 1444648.
- ↑ Waag KL, Loff S, Zahn K, Ali M, Hien S, Kratz M, Neff W, Schaffelder R, Schaible T (2008). "Congenital diaphragmatic hernia: a modern day approach". Semin. Pediatr. Surg. 17 (4): 244–54. doi:10.1053/j.sempedsurg.2008.07.009. PMID 19019293.
- ↑ 17.0 17.1 Kesieme EB, Kesieme CN (2011). "Congenital diaphragmatic hernia: review of current concept in surgical management". ISRN Surg. 2011: 974041. doi:10.5402/2011/974041. PMC 3251163. PMID 22229104.
- ↑ Clark RH, Hardin WD, Hirschl RB, Jaksic T, Lally KP, Langham MR, Wilson JM (1998). "Current surgical management of congenital diaphragmatic hernia: a report from the Congenital Diaphragmatic Hernia Study Group". J. Pediatr. Surg. 33 (7): 1004–9. PMID 9694085.
- ↑ Shue EH, Miniati D, Lee H (2012). "Advances in prenatal diagnosis and treatment of congenital diaphragmatic hernia". Clin Perinatol. 39 (2): 289–300. doi:10.1016/j.clp.2012.04.005. PMID 22682380.