Dengue fever physical examination: Difference between revisions
(→Skin) |
|||
| Line 13: | Line 13: | ||
==Skin== | ==Skin== | ||
[[Petechiae]] may be present | [[Petechiae]] may be present. | ||
<gallery> | |||
Image:Denguerash.jpg|The above picture is a [[rash]] typically associated with Dengue fever. | |||
</gallery> | |||
==Mental Status== | ==Mental Status== | ||
Revision as of 19:19, 14 June 2014
|
Dengue Fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Dengue fever physical examination On the Web |
|
American Roentgen Ray Society Images of Dengue fever physical examination |
|
Risk calculators and risk factors for Dengue fever physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The physical examination in Dengue fever should be directed to ward identifying signs that the patient has severe disease warranting admission or in-hospital observation.
Vital Signs
Tachycardia, postural hypotension, and hypotension could indicate dehydration. Patients who are triaged to home management should urinate at least every 6 hours.
The tourniquet test
Skin
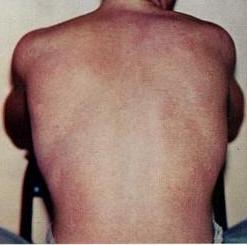
Petechiae may be present.
-
The above picture is a rash typically associated with Dengue fever.
Mental Status
Lethargy and restlessness are warning signs that the patient should be monitored.
HEENT
Mucosal bleeding is a warning signs that the patient should be monitored.
Abdomen
- Abdominal pain or tenderness are warning signs that the patient should be monitored.
- Liver enlargment >2 cm is a warning signs that the patient should be monitored.
- Ascites is a warning signs that the patient should be monitored.
Extremities
- Pedal edema or evidence of fluid accumulation
• assessment of haemodynamic status (Textbox D);
• checking for quiet tachypnoea/acidotic breathing/pleural effusion;
Appearance of the Patient
The diagnosis of dengue is usually made clinically. The classic picture is high fever with no localising source of infection, a petechial rash with thrombocytopenia and relative leukopenia.
There exists a WHO definition of dengue haemorrhagic fever that has been in use since 1975; all four criteria must be fulfilled:
- Fever
- Haemorrhagic tendency (positive tourniquet test, spontaneous bruising, bleeding from mucosa, gingiva, injection sites, etc.; vomiting blood, or bloody diarrhea)
- Thrombocytopaenia (<100,000 platelets per mm³ or estimated as less than 3 platelets per high power field)
- Evidence of plasma leakage (hematocrit more than 20% higher than expected, or drop in haematocrit of 20% or more from baseline following IV fluid, pleural effusion, ascites, hypoproteinaemia)
Dengue shock syndrome is defined as dengue haemorrhagic fever plus:
- Weak rapid pulse,
- Narrow pulse pressure (less than 20 mm Hg)
or,
- Hypotension for age;
- Cold, clammy skin and restlessness.