Dacryocystitis
|
WikiDoc Resources for Dacryocystitis |
|
Articles |
|---|
|
Most recent articles on Dacryocystitis Most cited articles on Dacryocystitis |
|
Media |
|
Powerpoint slides on Dacryocystitis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Dacryocystitis at Clinical Trials.gov Trial results on Dacryocystitis Clinical Trials on Dacryocystitis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Dacryocystitis NICE Guidance on Dacryocystitis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Dacryocystitis Discussion groups on Dacryocystitis Patient Handouts on Dacryocystitis Directions to Hospitals Treating Dacryocystitis Risk calculators and risk factors for Dacryocystitis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Dacryocystitis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Fatimo Biobaku M.B.B.S [2]
Overview
Anatomy of the Lacrimal System[1][2]
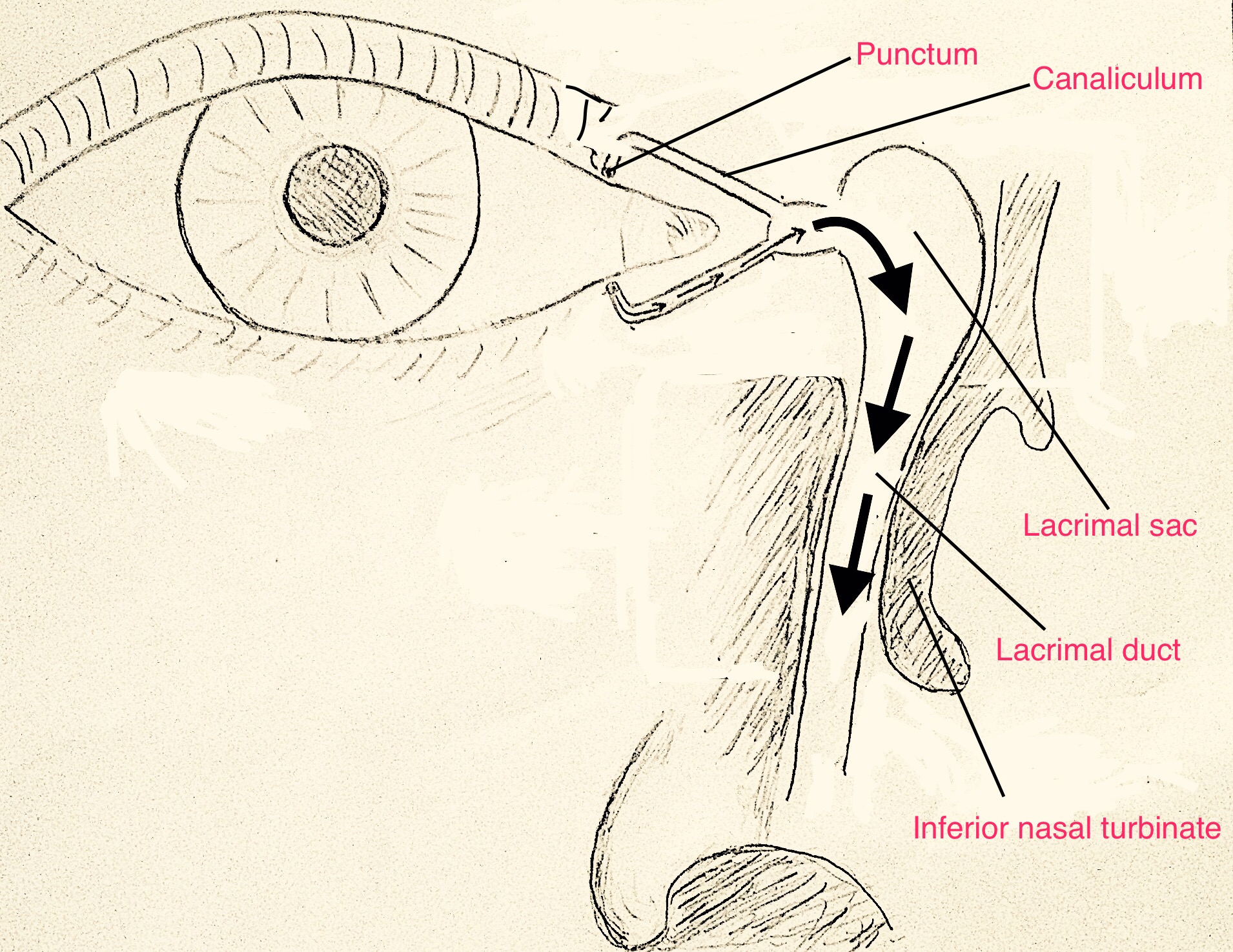
The lacrimal gland produces tears, and it secretes an approximate volume of 10mL in 24hrs. Tears flow across the eye, draining into the puncta, canaliculi, lacrimal sac, and lacrimal duct into the nasal cavity. The valves within the drainage system are unidirectional, allowing one-way flow of tears only.
Classification
Dacryocystitis may be classified as:[2]
- Acute- This is an acute inflammation of the lacrimal sac with tenderness and erythema of the overlying tissues.[3]
- Subacute
- Chronic- This may be the end stage of acute/subacute dacryocystitis, and dacryocystorhinostomy is commonly the definitive management when chronic or recurrent dacryocystitis occurs.[1]
Pathophysiology[4][5]
Dacryocystitis is an inflammation and infection of the lacrimal sac. Dacryocystitis usually occurs following partial/complete obstruction within the nasolacrimal duct or in the lacrimal sac, and it is the most common infection of the lacrimal apparatus. Nasolacrimal duct obstruction can occur in any age group, and it can be congenital or acquired. The lacrimal excretory system drain tears from the eyes into the nasal cavity, and its mucus membrane-lined tract is contiguous with the conjunctival and nasal mucosal surfaces which are normally colonized with bacteria. Following the obstruction of the nasolacrimal duct, stasis occurs with the accumulation of tears, desquamated cells, and mucoid secretions, creating an enabling environment for superimposed bacterial infection.
Nasolacrimal duct obstruction
- Congenital obstruction- This occurs in 3–6% of term infants. The nasal end of the duct is commonly affected, and it can be blocked by epithelial debris or an imperforate mucosal membrane resulting from incomplete canalization of the embryonic duct.
- Acquired obstruction- This can be primary or secondary.
- Primary acquired nasolacrimal duct obstruction- seen in idiopathic inflammatory stenosis.
- Secondary acquired nasolacrimal duct obstruction- occurs as a result of trauma, infection, inflammation, neoplasm, or mechanical obstruction.
Causes
Bacterial Causes[6]
The most common aerobic organisms
- Staphylococcus spp like S. epidermidis, S. aureus.
- Streptococcus spp
- Pseudomonas spp
- Pneumococcal species
The most common anaerobic organisms:
- Peptostreptococcus spp
- Propionibacterium spp
- Prevotella spp
- Fusobacterium species
The most common gram-negative bacteria
Fungal causes[6]
- Actinomyces spp
- Aspergillus spp
- Candida species
Differential Diagnosis
Epidemiology and Demographics
Risk Factors
Natural History, Complications, and Prognosis
Diagnosis
Treatment
Clincial Features
- pain, swelling, redness over the lacrimal sac at medial canthus.
- tearing, crusting, fever
- digital pressure over the lacrimal sac may extrude pus through the punctum
- In chronic cases, tearing may be the only symptom
Diagnosis
Patient #1: CT images demonstrate dacryocystitis and preseptal cellulitis
Treatment
- warm compresses, nasal decongestants, systemic and topic antibiotics
- if chronic, obtain cultures by aspiration
- Once infection resolves consider Dacryocystorhinostomy(DCR)
References
- ↑ 1.0 1.1 1.2 Durand, Marlene (2015). "Chapter 118:Periocular infections". Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases Updated Edition, Eighth Edition. Elsevier. pp. 1432–1438. ISBN 978-1-4557-4801-3.
- ↑ 2.0 2.1 Jeffrey, Hurwitz (2014). "Chapter12.15:The Lacrimal Drainage System". Ophthalmology, Fourth Edition. Elsevier. pp. 1346–1351. ISBN 978-1-4557-5001-6.
- ↑ 3.0 3.1 Eshraghi B, Abdi P, Akbari M, Fard MA (2014). "Microbiologic spectrum of acute and chronic dacryocystitis". Int J Ophthalmol. 7 (5): 864–7. doi:10.3980/j.issn.2222-3959.2014.05.23. PMC 4206896. PMID 25349808.
- ↑ Bharathi MJ, Ramakrishnan R, Maneksha V, Shivakumar C, Nithya V, Mittal S (2008). "Comparative bacteriology of acute and chronic dacryocystitis". Eye (Lond). 22 (7): 953–60. doi:10.1038/sj.eye.6702918. PMID 17603466.
- ↑ Wadgaonkar S.P., Patil P.A., Nikumbh D.B., Rathod S.S. and Sawat C.M. (2016). "Epidemiology of chronic dacryocystitis with special reference to socioeconomic status: A rural hospital study" (PDF). Indian Journal of Clinical and Experimental Ophthalmology. 2 (1): 52–56.
- ↑ 6.0 6.1 Asheim J, Spickler E (2005). "CT demonstration of dacryolithiasis complicated by dacryocystitis". AJNR Am J Neuroradiol. 26 (10): 2640–1. PMID 16286415.
External Links
de:Dakryozystitis id:Dakriosistitis Template:WikiDoc Sources Template:WH


