Cystic fibrosis transmembrane conductance regulator
| Cystic fibrosis transmembrane conductance regulator (ATP-binding cassette sub-family C, member 7) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 PDB rendering based on 1xmi. | |||||||||||||
| |||||||||||||
| Identifiers | |||||||||||||
| Symbols | CFTR ; ABC35; ABCC7; CF; CFTR/MRP; MRP7; TNR-CFTR; dJ760C5.1 | ||||||||||||
| External IDs | Template:OMIM5 Template:MGI HomoloGene: 55465 | ||||||||||||
| |||||||||||||
| Orthologs | |||||||||||||
| Template:GNF Ortholog box | |||||||||||||
| Species | Human | Mouse | |||||||||||
| Entrez | n/a | n/a | |||||||||||
| Ensembl | n/a | n/a | |||||||||||
| UniProt | n/a | n/a | |||||||||||
| RefSeq (mRNA) | n/a | n/a | |||||||||||
| RefSeq (protein) | n/a | n/a | |||||||||||
| Location (UCSC) | n/a | n/a | |||||||||||
| PubMed search | n/a | n/a | |||||||||||
Cystic fibrosis transmembrane conductance regulator (CFTR) is an ABC transporter-class protein and ion channel that transports chloride ions across epithelial cell membranes. Mutations of the CFTR gene affect functioning of the chloride ion channels in these cell membranes, leading to cystic fibrosis and congenital absence of the vas deferens.
Structure
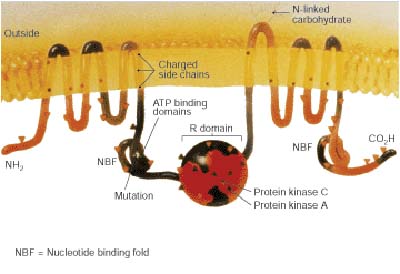
The gene that encodes for CFTR is found on the human chromosome 7, on the long arm at position q31.2. It contains about 170,000 base pairs. The encoded CFTR is a glycoprotein with 1480 amino acids. It contains two transmembrane regions , each with six spans of alpha helices, that are connected to their cytoplasmatic nucleotide binding folds (NBF). These two nucleotide binding folds are linked to a single R-domain that is a unique feature of this type of ABC protein. ATP is bound to the two NBFs. The carboxyl terminal of the protein is anchored to the cytoskeleton by a PDZ domain interaction.[1]
Function
The CFTR is found in the epithelial cells of many organs including the lung, liver, pancreas, digestive tract, reproductive tract, and skin. Normally, the protein moves chloride ions (with a negative charge) out of an epithelial cell to the covering mucus. This results in an electrical gradient being formed and in the movement of (positively charged) sodium ions in the opposite direction via the ENaC. Due to this movement, the water potential of the mucus is reduced, resulting in the movement of water here by osmosis and a more fluid mucus.
In sweat glands, CFTR defects result in reduced transport of sodium chloride in the reabsorptive duct and saltier sweat. This was the basis of a clinically important sweat test for cystic fibrosis before genetic screening was available ( see The Relevance of Sweat Testing for the Diagnosis of Cystic Fibrosis in the Genomic Era).
Mutations
Well over one thousand mutations have been described that can affect the CFTR gene. Such mutations can cause two genetic disorders, congenital bilateral absence of vas deferens and the more widely known disorder cystic fibrosis. Both disorders arise from the blockage of the movement of ions and, therefore, water into and out of cells. In congenital bilateral absence of vas deferens, the protein may be still functional but not at normal efficiency, this leads to the production of thick mucus, which blocks the developing vas deferens. In people with mutations giving rise to cystic fibrosis, the blockage in ion transport occurs in epithelial cells that line the passageways of the lungs, pancreas, and other organs. This leads to chronic dysfunction, disability, and a reduced life expectancy.
The most common mutation, ΔF508 results from a deletion (Δ) of three nucleotides which results in a loss of the amino acid phenylalanine (F) at the 508th (508) position on the protein. As a result the protein does not fold normally and is more quickly degraded.
The vast majority of mutations are quite rare. The distribution and frequency of mutations varies among different populations which has implications for genetic screening and counseling.
Mutations consist of replacements, duplications, deletions or shortenings in the CFTR gene. This may result in proteins that may not function, work less effectively, are more quickly degraded, or are present in inadequate numbers..[2]
It has been hypothesized that mutations in the CFTR gene may confer a selective advantage to heterozygous individuals. Cells expressing a mutant form of the CFTR protein are resistant to invasion by the Salmonella typhii bacterium, the agent of typhoid fever, and mice carrying a single copy of mutant CFTR are resistant to diarrhea caused by cholera toxin.
List of common mutations
The most common mutations in a Caucasian population are: [3]
- ΔF508
- G542X
- G551D
- N1303K
- W1282X
References
- ↑ Short DB, Trotter KW, Reczek D, Kreda SM, Bretscher A, Boucher RC, Stutts MJ, Milgram SL. An apical PDZ protein anchors the cystic fibrosis transmembrane conductance regulator to the cytoskeleton. J Biol Chem. 1998 Jul 31;273(31):19797-801. PMID 9677412
- ↑ Rowe SM, Miller S, Sorscher EJ. Cystic fibrosis. N Engl J Med. 2005 May 12;352(19):1992-2001. PMID 15888700
- ↑ Prevalence of ΔF508, G551D, G542X, R553X mutations among cystic fibrosis patients in the North of Brazil. Brazilian Journal of Medical and Biological Research 2005; 38:11-15. PMID 15665983
Further reading
- Tsui LC (1993). "Mutations and sequence variations detected in the cystic fibrosis transmembrane conductance regulator (CFTR) gene: a report from the Cystic Fibrosis Genetic Analysis Consortium". Hum. Mutat. 1 (3): 197–203. doi:10.1002/humu.1380010304. PMID 1284534.
- McIntosh I, Cutting GR (1992). "Cystic fibrosis transmembrane conductance regulator and the etiology and pathogenesis of cystic fibrosis". FASEB J. 6 (10): 2775–82. PMID 1378801.
- Drumm ML, Collins FS (1993). "Molecular biology of cystic fibrosis". Mol. Genet. Med. 3: 33–68. PMID 7693108.
- Kerem B, Kerem E (1996). "The molecular basis for disease variability in cystic fibrosis". Eur. J. Hum. Genet. 4 (2): 65–73. PMID 8744024.
- Devidas S, Guggino WB (1998). "CFTR: domains, structure, and function". J. Bioenerg. Biomembr. 29 (5): 443–51. PMID 9511929.
- Nagel G (2000). "Differential function of the two nucleotide binding domains on cystic fibrosis transmembrane conductance regulator". Biochim. Biophys. Acta. 1461 (2): 263–74. PMID 10581360.
- Boyle MP (2003). "Unique presentations and chronic complications in adult cystic fibrosis: do they teach us anything about CFTR?". Respir. Res. 1 (3): 133–5. PMID 11667976.
- Greger R, Schreiber R, Mall M; et al. (2002). "Cystic fibrosis and CFTR". Pflugers Arch. 443 Suppl 1: S3–7. doi:10.1007/s004240100635. PMID 11845294.
- Bradbury NA (2002). "cAMP signaling cascades and CFTR: is there more to learn?". Pflugers Arch. 443 Suppl 1: S85–91. doi:10.1007/s004240100651. PMID 11845310.
- Dahan D, Evagelidis A, Hanrahan JW; et al. (2002). "Regulation of the CFTR channel by phosphorylation". Pflugers Arch. 443 Suppl 1: S92–6. doi:10.1007/s004240100652. PMID 11845311.
- Cohn JA, Noone PG, Jowell PS (2002). "Idiopathic pancreatitis related to CFTR: complex inheritance and identification of a modifier gene". J. Investig. Med. 50 (5): 247S–255S. PMID 12227654.
- Kulczycki LL, Kostuch M, Bellanti JA (2003). "A clinical perspective of cystic fibrosis and new genetic findings: relationship of CFTR mutations to genotype-phenotype manifestations". Am. J. Med. Genet. A. 116 (3): 262–7. doi:10.1002/ajmg.a.10886. PMID 12503104.
- Schwartz M (2003). "[Cystic fibrosis transmembrane conductance regulator (CFTR) gene: mutations and clinical phenotypes]". Ugeskr. Laeg. 165 (9): 912–6. PMID 12661515.
- Wong LJ, Alper OM, Wang BT; et al. (2004). "Two novel null mutations in a Taiwanese cystic fibrosis patient and a survey of East Asian CFTR mutations". Am. J. Med. Genet. A. 120 (2): 296–8. doi:10.1002/ajmg.a.20039. PMID 12833420.
- Cuppens H, Cassiman JJ (2005). "CFTR mutations and polymorphisms in male infertility". Int. J. Androl. 27 (5): 251–6. doi:10.1111/j.1365-2605.2004.00485.x. PMID 15379964.
- Cohn JA, Mitchell RM, Jowell PS (2005). "The impact of cystic fibrosis and PSTI/SPINK1 gene mutations on susceptibility to chronic pancreatitis". Clin. Lab. Med. 25 (1): 79–100. doi:10.1016/j.cll.2004.12.007. PMID 15749233.
- Southern KW, Peckham D (2005). "Establishing a diagnosis of cystic fibrosis". Chronic respiratory disease. 1 (4): 205–10. PMID 16281647.
- Kandula L, Whitcomb DC, Lowe ME (2006). "Genetic issues in pediatric pancreatitis". Current gastroenterology reports. 8 (3): 248–53. PMID 16764792.
- Marcet B, Boeynaems JM (2007). "Relationships between cystic fibrosis transmembrane conductance regulator, extracellular nucleotides and cystic fibrosis". Pharmacol. Ther. 112 (3): 719–32. doi:10.1016/j.pharmthera.2006.05.010. PMID 16828872.
- Wilschanski M, Durie PR (2007). "Patterns of GI disease in adulthood associated with mutations in the CFTR gene". Gut. 56 (8): 1153–63. doi:10.1136/gut.2004.062786. PMID 17446304.
External links
- The Cystic Fibrosis Transmembrane Conductance Regulator Protein
- The Human Gene Mutation Database - CFTR Records
- Cystic Fibrosis Mutation Database
- Oak Ridge National Laboratory CFTR Information
- CFTR at OMIM (National Center for Biotechnology Information)
de:Cystic Fibrosis Transmembrane Conductance Regulator sk:Cystic fibrosis transmembrane conductance regulator