Cushing's syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 15: | Line 15: | ||
{{SI}} | {{SI}} | ||
'''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
{{CMG}} | {{CMG}} | ||
Revision as of 18:08, 9 July 2009
| Cushing's syndrome | |
 | |
|---|---|
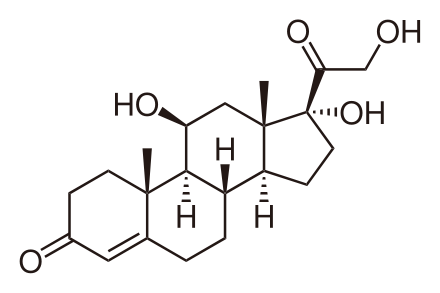
| Cortisol | |
| ICD-10 | E24 |
| ICD-9 | 255.0 |
| DiseasesDB | 3242 |
| MedlinePlus | 000410 |
| eMedicine | med/485 |
| MeSH | D003480 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Cushing's Syndrome (also called hypercortisolism or hyperadrenocorticism) is an endocrine disorder caused by high levels of cortisol in the blood from a variety of causes, including primary pituitary adenoma (known as Cushing's disease), primary adrenal hyperplasia or neoplasia, ectopic ACTH production (e.g., from a small cell lung cancer), and iatrogenic (steroid use). Normally, cortisol is released from the adrenal gland in response to ACTH being released from the pituitary gland. Both Cushing's syndrome and Cushing's disease are characterized by elevated levels of cortisol in the blood, but the cause of elevated cortisol differs between the two. Cushing's disease specifically refers to a tumour in the pituitary gland that stimulates excessive release of cortisol from the adrenal gland by releasing large amounts of ACTH. In Cushing's disease, ACTH levels do not respond to negative feedback from the high levels of cortisol.
Cushing's disease was described by American physician, surgeon and endocrinologist Harvey Cushing (1869-1939) and reported by him in 1932.[1]
Cushing's syndrome--which is also a relatively common condition in domestic dogs and horses--is characterised by abnormal fat deposition.
Signs and symptoms
Symptoms include rapid weight gain, particularly of the trunk and face with sparing of the limbs (central obesity), a round face often referred to as a "moon face", excess sweating, telangiectasia (dilation of capillaries), thinning of the skin (which causes easy bruising) and other mucous membranes, purple or red striae (the weight gain in Cushing's stretches the skin, which is thin and weakened, causing it to hemorrhage) on the trunk, buttocks, arms, legs or breasts, proximal muscle weakness (hips, shoulders), and hirsutism (facial male-pattern hair growth). A common sign is the growth of fat pads along the collar bone and on the back of the neck (known as a lipodystrophy). The excess cortisol may also affect other endocrine systems and cause, for example, insomnia, reduced libido, impotence, amenorrhoea and infertility. Patients frequently suffer various psychological disturbances, ranging from euphoria to psychosis. Depression and anxiety are also common.[2]
Other signs include persistent hypertension (due to cortisol's enhancement of epinephrine's vasoconstrictive effect) and insulin resistance (especially common in ectopic ACTH production), leading to hyperglycemia (high blood sugars) which can lead to diabetes mellitus. Untreated Cushing's syndrome can lead to heart disease and increased mortality. Cushing's syndrome due to excess ACTH may also result in hyperpigmentation. This is due to Melanocyte-Stimulating Hormone production as a byproduct of ACTH synthesis from Proopiomelanocortin (POMC). Cortisol can also exhibit mineralcorticoid activity in high concentrations, worsening the hypertension and leading to hypokalemia (common in ectopic ACTH secretion). Furthermore, gastrointestinal disturbances, opportunistic infections and impaired wound healing (cortisol is a stress hormone, so it depresses the immune and inflammatory responses). Osteoporosis is also problem in Cushing's Syndrome, as mentioned before, cortisol evokes a stress-like response. The body's maintenance of bone (and other tissues) is therefore no longer one of its main priorities, so to speak.
Moon face is a medical sign where the face swells up into a rounded shape. It is often associated with Cushing's syndrome, which has led to it being known as Cushingoid facies ("Cushings-like face"), or steroid treatment, which has led to the name steroid facies.
Exogenous Versus Endogenous
There are two types of Cushing’s syndrome: exogenous and endogenous. In endogenous disease, excess cortisol production within the body is the cause, whilst in exogenous disease the causal factor is typically steroid medication (i.e. it originates outside the body) mimicing cortisol's activity. The signs and symptoms are therefore virtually identical, aside from those induced by ACTH in pituitary-dependent disease and ectopic ACTH-producing tumours (such as hyperpigmentation). The exogenous route is by far the most commonly taken in Cushing’s syndrome (a fact that all too many seem to forget). Examples of such exogenous steroid medications are those used to treat inflammatory disorders such as asthma and rheumatoid arthritis, or to suppress the immune system after an organ transplant. This type of Cushing’s is temporary and goes away after the patient has finished taking the cortisol-like medications. Endogenous Cushing’s syndrome is unusual, it usually comes on slowly and can be difficult to diagnose.
Diagnosis
When Cushing's is suspected, either a dexamethasone suppression test (administration of dexamethasone and frequent determination of cortisol and ACTH level), or a 24-hour urinary measurement for cortisol offer equal detection rates.[3] Dexamethasone is a glucocorticoid and simulates the effects of cortisol, including negative feedback on the pituitary gland. When dexamethasone is administered and a blood sample is tested, high cortisol would be indicative of Cushing's syndrome because there is an ectopic source of cortisol or ACTH (eg: adrenal adenoma) that is not inhibited by the dexamethasone. A novel approach, recently cleared by the US FDA, is sampling cortisol in saliva over 24 hours, which may be equally sensitive, as late night levels of salivary cortisol are high in Cushingoid patients. Other pituitary hormone levels may need to be ascertained. Performing a physical examination to determine any visual field defect may be necessary if a pituitary lesion is suspected, which may compress the optic chiasm causing typical bitemporal hemianopia.
When any of these tests are positive, CT scanning of the adrenal gland and MRI of the pituitary gland are performed to detect the presence of any adrenal or pituitary adenomas or incidentalomas (the incidental discovery of harmless lesions). Scintigraphy of the adrenal gland with iodocholesterol scan is occasionally necessary. Very rarely, determining the cortisol levels in various veins in the body by venous catheterisation, working towards the pituitary (petrosal sinus sampling) is necessary.
Pathophysiology
Both the hypothalamus and the pituitary gland are in the brain. The hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to release corticotropin (ACTH). ACTH travels via the blood to the adrenal gland, where it stimulates the release of cortisol. Cortisol is secreted by the cortex of the adrenal gland from a region called the zona fasciculata in response to ACTH. Elevated levels of cortisol exert negative feedback on the pituitary, which decreases the amount of ACTH released from the pituitary gland. Strictly, Cushing's syndrome refers to excess cortisol of any etiology. One of the causes of Cushing's syndrome is a cortisol secreting adenoma in the cortex of the adrenal gland. The adenoma causes cortisol levels in the blood to be very high, and negative feedback on the pituitary from the high cortisol levels causes ACTH levels to be very low. Cushing's disease refers only to hypercortisolism secondary to excess production of ACTH from a corticotrophic pituitary adenoma. This causes the blood ACTH levels to be elevated along with cortisol from the adrenal gland. The ACTH levels remain high because a tumor causes the pituitary to be unresponsive to negative feedback from high cortisol levels.
Treatment
The main point to remember is that the vast majority of cases of Cushing's syndrome are caused by steroid medications (such causes are described as iatrogenic) so healthcare workers must always remember to check patients' medications first, as stopping or reducing the dose will usually resolve the problem.
If an adrenal adenoma is identified it may be removed by surgery. An ACTH-secreting corticotrophic pituitary adenoma should be removed after diagnosis. Regardless of the adenoma's location, most patients will require steroid replacement postoperatively at least in the interim as long-term suppression of pituitary ACTH and normal adrenal tissue does not recover immediately. Clearly, if both adrenals are removed, replacement with hydrocortisone or prednisolone is imperative.
In those patients not suitable for or unwilling to undergo surgery, several drugs have been found to inhibit cortisol synthesis (e.g. ketoconazole, metyrapone) but they are of limited efficacy.
Removal of the adrenals in the absence of a known tumor is occasionally performed to eliminate the production of excess cortisol. In some occasions, this removes negative feedback from a previously occult pituitary adenoma, which starts growing rapidly and produces extreme levels of ACTH, leading to hyperpigmentation. This clinical situation is known as Nelson's syndrome.[4]
Epidemiology
Iatrogenic Cushing's (caused by treatment with corticosteroids) is the most common form of Cushing's syndrome. The incidence of pituitary tumors may be relatively high, as much as one in five people, [5] but only a minute fraction are active and produce excessive hormones.
See also
References
- ↑ Cushing HW. The basophil adenomas of the pituitary body and their clinical manifestations (pituitary basophilism). Bull Johns Hopkins Hosp 1932;50:137-195.
- ↑ Yudofsky, Stuart C. (2007). The American Psychiatric Publishing Textbook of Neuropsychiatry and Behavioral Neurosciences (5th ed.). American Psychiatric Pub, Inc. ISBN 1585622397. Unknown parameter
|coauthors=ignored (help) - ↑ Raff H, Findling JW. A physiologic approach to diagnosis of the Cushing's syndrome. Ann Intern Med 2003;138:980-91. PMID 12809455
- ↑ Nelson DH, Meakin JW, Thorn GW. ACTH-producing tumors following adrenalectomy for Cushing's syndrome. Ann Intern Med 1960;52:560–569. PMID 14426442
- ↑ Ezzat S, Asa SL, Couldwell WT; et al. (2004). "The prevalence of pituitary adenomas: a systematic review". Cancer. 101 (3): 613–9. doi:10.1002/cncr.20412. PMID 15274075.
External links
- Cushing's Syndrome
- Cushing's information at Oregon Health Sciences University
- Cushing's Fact Sheets from The Hormone Foundation
- Cushing's Help and Support
- Cushing's syndrome
- Cushing Syndrome information at Merck.com
- Endocrine and Metabolic Diseases Information Service
da:Cushings syndrom de:Cushing-Syndrom eo:Cushing-sindromo id:Sindrom Cushing it:Sindrome di Cushing he:תסמונת קושינג ms:Sindrom Cushing nl:Syndroom van Cushing no:Cushings sykdom sv:Cushings syndrom