Creutzfeldt-Jakob disease epidemiology and demographics
|
Creutzfeldt-Jakob disease Microchapters |
|
Differentiating Creutzfeldt-Jakob disease from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Creutzfeldt-Jakob disease epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Creutzfeldt-Jakob disease epidemiology and demographics |
|
FDA on Creutzfeldt-Jakob disease epidemiology and demographics |
|
CDC on Creutzfeldt-Jakob disease epidemiology and demographics |
|
Creutzfeldt-Jakob disease epidemiology and demographics in the news |
|
Blogs on Creutzfeldt-Jakob disease epidemiology and demographics |
|
Risk calculators and risk factors for Creutzfeldt-Jakob disease epidemiology and demographics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Creutzfeldt Jakob disease is a very rare disorder with an incidence of 1 case per 1 million per year.
Epidemiology and Demographics
Classic CJD has been recognized since the early 1920s. The most common form of classic CJD is believed to occur sporadically, caused by the spontaneous transformation of normal prion proteins into abnormal prions.
- This sporadic disease occurs worldwide, including the United States, at a rate of approximately one case per 1 million population per year, although rates of up to two cases per million are not unusual.
- The risk of CJD increases with age, and in persons aged over 50 years of age, the annual rate is approximately 3.4 cases per million.
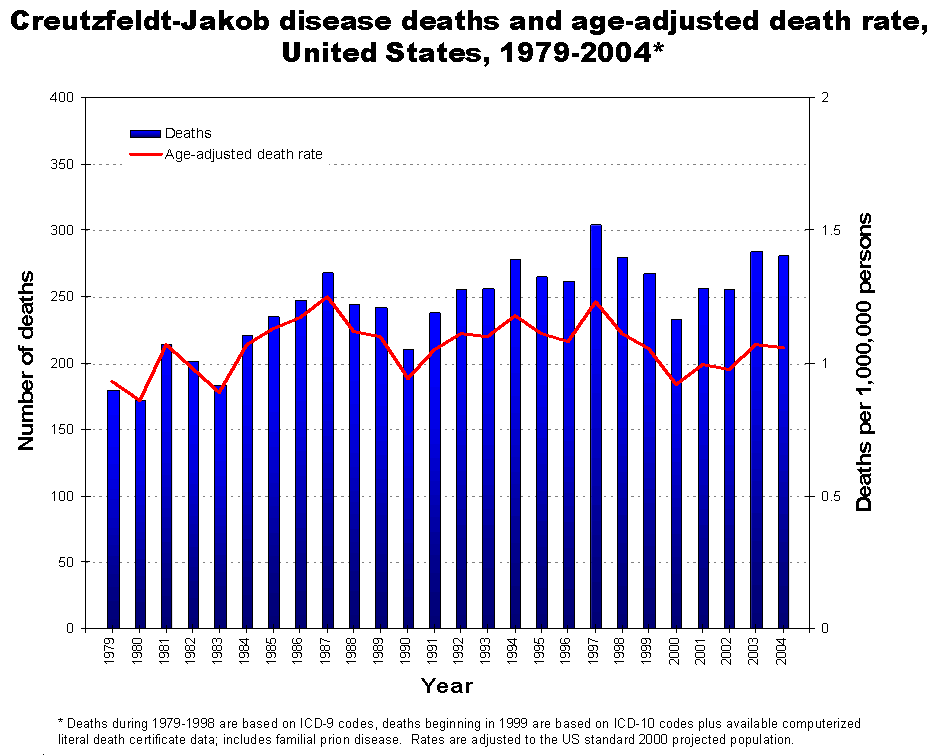
- In recent years, the United States has reported fewer than 300 cases of CJD a year.
Whereas the majority of cases of CJD (about 85%) occur as sporadic disease, a smaller proportion of patients (5-15%) develop CJD because of inherited mutations of the prion protein gene. These inherited forms include Gerstmann-Straussler-Scheinker syndrome and fatal familial insomnia.
Incidence and Prevalence
Although CJD is the most common human prion disease, it is still rare and only occurs in about one out of every one million people. It usually affects people aged 45–75, most commonly appearing in people between the ages of 60–65. The exception to this is the more recently-recognised 'variant' CJD (vCJD), which occurs in younger people. CDC monitors the occurrence of CJD in the United States through periodic reviews of national mortality data. According to the CDC:
- CJD occurs worldwide at a rate of about 1 case per million population per year.
- On the basis of mortality surveillance from 1979 to 1994, the annual incidence of CJD remained stable at approximately 1 case per million persons in the United States.
- In the United States, CJD deaths among persons younger than 30 years of age are extremely rare (fewer than 5 deaths per billion per year).
- In more than 85% of cases, the duration of CJD is less than 1 year (median: 4 months) after onset of symptoms.[1][2]
New Concerns on Incidence and Prevalence
In The Lancet (June 2006), a University College London team suggested that it may take more than 50 years for vCJD to develop, from their studies of kuru, a similar disease in Papua New Guinea. The reasoning behind the claim is that kuru was transmitted through cannibalism in Papua New Guinea when relatives would eat their dead relative's bodies as a sign of mourning. In the 1950s, the practice was banned, thereby preventing any further possible transmission. In the late 20th century, however, kuru reached epidemic proportions in certain Papua New Guinean communities, therefore suggesting that vCJD may also have a similar incubation period of 30 to 50 years. A critique to this theory is that while mortuary cannibalism was banned in Papua New Guinea in the 1950s, that does not necessarily mean that the practice ended. Fifteen years later Jared Diamond was informed by Papuans that the practice continued.[3]
These researchers noticed a genetic variation in some kuru patients that has been known to promote long incubation periods. They have also proposed that individuals who contracted CJD in the early 1990s represent a distinct genetic subpopulation, with unusually short incubation periods for BSE. This means that there may be many more vCJD patients who have longer incubation periods, which may surface many years later.
Age
- The risk of CJD increases with age.
- The disease is found most frequently in patients 55 to 65 years of age, but cases can occur in persons older than 90 years and younger than 55 years of age.
References
- ↑ "Homepage". Retrieved 2007-12-02. Text " CDC Classic CJD " ignored (help)
- ↑ "Variant CJD, Fact Sheet". Retrieved 2007-12-02. Text " CDC vCJD" ignored (help)
- ↑ "Diamond, J.M. (2000)"Archaeology: Talk of cannibalism" Nature 407, 25-26".