Coronary artery thrombus: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
{{SK}} Coronary thrombosis; coronary thrombus | {{SK}} Coronary thrombosis; coronary thrombus | ||
Revision as of 18:57, 15 November 2013
Synonyms and keywords: Coronary thrombosis; coronary thrombus
Overview
The Thrombus of coronary arteries occurs when the lumen, of the artery starts becoming smaller and creates a narrowed segment in which the blood flow clots slowly in the artery. This phenomenum in coronary artery decreases the perfusion and may cause necrosis which may lead to a heart attack if not treated.[1]
Definition
The coronary artery thrombus may be defined as an occlusion or blockage of blood flow within a vessel due to a clot.[1]
Pathophysiology
The pathogenic process of arterial thrombosis involves the formation of platelet-rich “white clots” after the rupture of atherosclerotic plaques and exposure of procoagulant material such as lipid-rich macrophages (foam cells), collagen, tissue factor, and/or endothelial breach, in a high shear environment. The exposed material come from within the plaque and also from the activation and aggregation of platelets. Platelet accumulation and fibrin deposition cause an occlusive platelet-rich intravascular thrombus. The growing thrombus increases the degree of narrowing, which may result in extremely high shear rates within the stenotic region. This phenomenum is responsible for a turbulent flow which is developed downstream of the stenosis depending on stenosis geometry and location in the vasculature.[2][3]
Clinical Significance
- The location of the thrombosis is clinically relevant once the infarction may be subclinical or not.[4]
- Coronary thrombosis may be a complication related to drug-eluting stents.[4]
TIMI Thrombus Grade
A patient is considered to have angiographically evident thrombus (AET) if TIMI thrombus grades 2 to 5 are present.[5]
TIMI Thrombus Grade 0
- None (no cineangiographic characteristics of thrombus present).
TIMI Thrombus Grade 1
- Possible thrombus present.
- Angiography demonstrates characteristics such as reduced contrast density, haziness, irregular lesion contour or a smooth convex "meniscus" at the site of total occlusion suggestive but not diagnostic of thrombus.
TIMI Thrombus Grade 2
- Thrombus present (small size).
- Definite thrombus with greatest dimensions less than or equal to ½ vessel diameter.
TIMI Thrombus Grade 3
- Thrombus present (moderate size).
- Definite thrombus but with greatest linear dimension greater than ½ but less than 2 vessel diameters.
TIMI Thrombus Grade 4
- Thrombus present (large size).
- As in Grade 3 but with the largest dimension greater than or equal to 2 vessel diameters.
TIMI Thrombus Grade 5
- Recent total occlusion, can involve some collateralization but usually does not involve extensive collateralization.
- The clot has not propagated backward to the most distal branch and there is often a beak-like appearance of the occlusion.
TIMI Thrombus Grade 6
- Chronic total occlusion, usually involving extensive collateralization.
- Tends to have distinct, blunt cut-off/edge and will generally clot up to the nearest proximal side branch.
Treatment
The treatment is based mainly on percutaneous coronary intervention which is commonly known as coronary angioplasty, is an invasive cardiologic therapeutic procedure to treat the stenotic (narrowed) coronary arteries of the heart. These stenotic segments are due to the build up of cholesterol-laden plaques that form due to atherosclerosis in coronary heart disease. PCI is usually performed by an interventional cardiologist. Percutaneous coronary intervention can be performed to reduce or eliminate the symptoms of coronary artery disease, including angina (chest pain), dyspnea (shortness of breath) on exertion, and congestive heart failure. PCI is also used to abort an acute myocardial infarction, and in some specific cases it may reduce mortality.
The pharmacological treatment may be done by intracoronary pharmacoterapy or through non invasive therapy that requires the use of thrombolytic drugs which can be prescribed also in association with percutaneous coronary intervention.
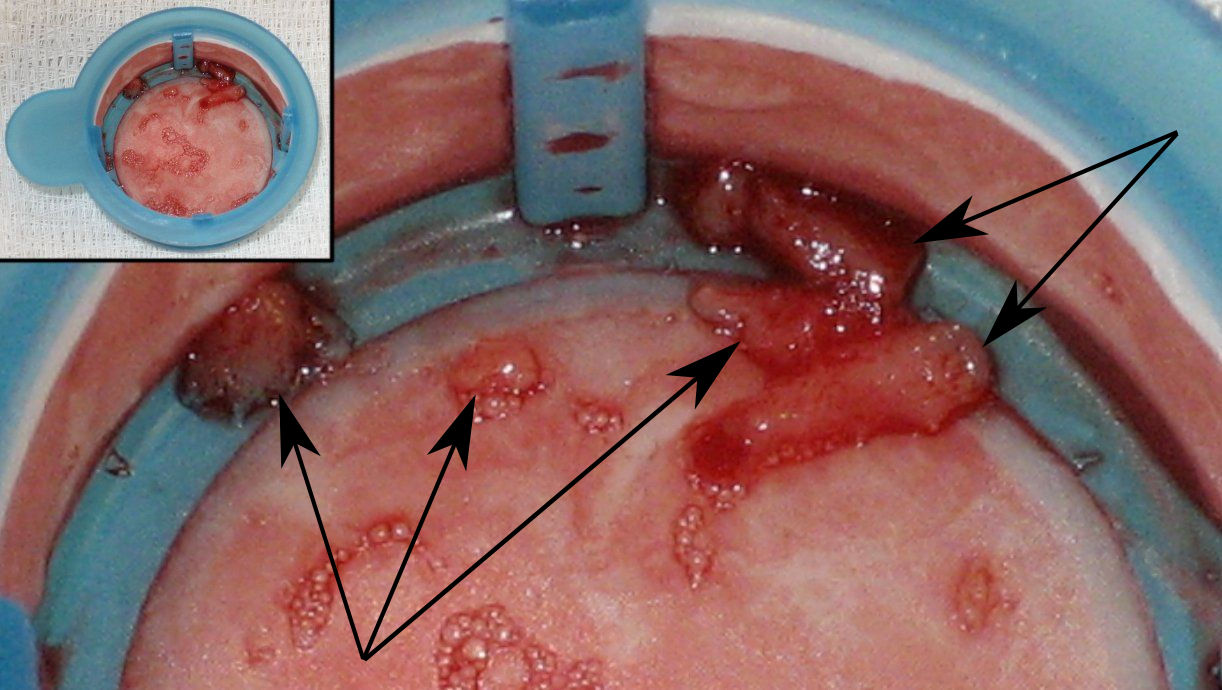
Examples
References
- ↑ 1.0 1.1 "http://www.cts.usc.edu/zglossary-thrombosis.html". Retrieved 14 November 2013. External link in
|title=(help) - ↑ Bark, DL.; Ku, DN. (2010). "Wall shear over high degree stenoses pertinent to atherothrombosis". J Biomech. 43 (15): 2970–7. doi:10.1016/j.jbiomech.2010.07.011. PMID 20728892. Unknown parameter
|month=ignored (help) - ↑ Wolberg, AS.; Aleman, MM.; Leiderman, K.; Machlus, KR. (2012). "Procoagulant activity in hemostasis and thrombosis: Virchow's triad revisited". Anesth Analg. 114 (2): 275–85. doi:10.1213/ANE.0b013e31823a088c. PMID 22104070. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 Lüscher, TF.; Steffel, J.; Eberli, FR.; Joner, M.; Nakazawa, G.; Tanner, FC.; Virmani, R. (2007). "Drug-eluting stent and coronary thrombosis: biological mechanisms and clinical implications". Circulation. 115 (8): 1051–8. doi:10.1161/CIRCULATIONAHA.106.675934. PMID 17325255. Unknown parameter
|month=ignored (help) - ↑ Gibson, CM.; de Lemos, JA.; Murphy, SA.; Marble, SJ.; McCabe, CH.; Cannon, CP.; Antman, EM.; Braunwald, E. (2001). "Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction: a TIMI 14 substudy". Circulation. 103 (21): 2550–4. PMID 11382722. Unknown parameter
|month=ignored (help)