Coronary artery dual ostia
|
Coronary Angiography | |
|
General Principles | |
|---|---|
|
Anatomy & Projection Angles | |
|
Normal Anatomy | |
|
Anatomic Variants | |
|
Projection Angles | |
|
Epicardial Flow & Myocardial Perfusion | |
|
Epicardial Flow | |
|
Myocardial Perfusion | |
|
Lesion Complexity | |
|
ACC/AHA Lesion-Specific Classification of the Primary Target Stenosis | |
|
Lesion Morphology | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2]
Synonyms and keywords: Separate ostia
Overview
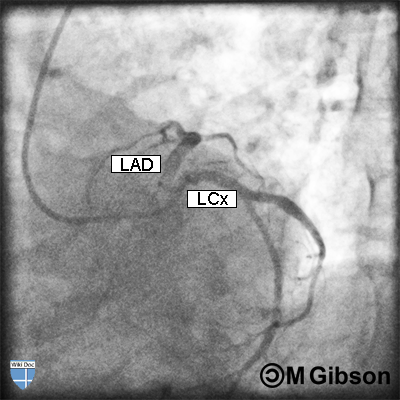
In cases of dual ostia, the left anterior descending artery (LAD) and left circumflex artery (LCx) arise from separate but adjacent ostia in the left sinus of Valsalva. This anomaly is considered as one of the most common benign anatomic variants of the coronary system.
Dual Ostia
The length of the left main coronary artery may vary from 1 mm to 10 mm. Occasionally, the left anterior descending artery (LAD) and left circumflex artery (LCx) may have separate openings in the left sinus of Valsalva. The anomaly generally does not cause hemodynamic alterations and the vessels are otherwise normal regarding to the territory they supply.
Epidemiology and Demographics
Dual ostia is reported to account for about 0.4% of the cases in a review and is considered as the most common benign coronary anomalies. This anomaly is found with increased incidence in the left-dominant coronary system as well as in aortic valve diseases.[1]
Angiographic Considerations
Angiographically, it may be difficult to determine whether the left main coronary artery is short or absent and a LAO caudal projection is usually obtained to provide optimal view to make the distinction. In cases of dual ostia, LAD generally has a more anterior and superior trajectory and selective engagement with the Judkins left (JL) catheter may be achieved by counterclockwise manipulations. The opposite maneuver can be used for selective cannulation of the LCx.
Additional Images
 |
 |
LAD = Left anterior descending artery; LCx = Left circumflex artery