Coronary artery bifurcation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 47: | Line 47: | ||
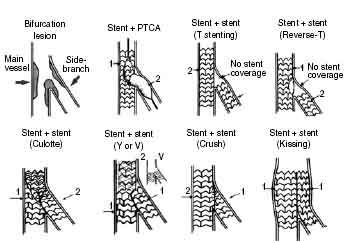
==Overview of Treatment Choices== | ==Overview of Treatment Choices== | ||
===PTCA=== | ===PTCA=== | ||
*Double guidewire followed by sequential PTCA | *Double guidewire followed by sequential PTCA | ||
*Kissing balloon dilation (i.e.: simultaneous balloon inflations) | *Kissing balloon dilation (i.e.: simultaneous balloon inflations) | ||
===Debulking=== | ===Debulking=== | ||
*Directional coronary atherectomy (DCA) | *Directional coronary atherectomy (DCA) | ||
*Rotational atherectomy (RA) | *Rotational atherectomy (RA) | ||
===Stenting=== | ===Stenting=== | ||
====Single Stent Technique==== | |||
The single stent technique (also known as “provisional stenting”) is most commonly adopted. It involves stenting the main branch and then rescuing the side branch with either balloon [[angioplasty]] or stenting if necessary. | |||
====T-stent Technique==== | |||
This involves stenting the side branch first to cover the ostium and then stenting the main branch. This approach can be difficult if the angle of the side branch is not 90 degrees and thus not allowing perfect alignment of the two stents. In this situation, there will either be side branch stent strut protruding into the main vessel or incomplete coverage of the side branch ostium. | |||
The modified T-stent approach (also known as “blocking balloon technique”) positions the side branch stent followed by a balloon placed in the main branch at the bifurcation. The main branch balloon is inflated first at low pressure to provide support against which the side branch stent can be aligned more accurately to cover the ostium without protruding. The side branch stent is then deployed followed by main branch stent deployment. | |||
In the TAP (T and small protrusion) technique, the main branch is stented first, and then the side branch is reaccessed and redilated. The side branch stent is then placed with a small amount of strut protruding into the main branch. A main branch blocking balloon is then inflated simultaneously with the side branch stent. | |||
====Culotte/Trousers Technique==== | |||
If necessary, both the main branch and side branch are first wired with pre-dilation to allow for better access. The parent vessel is then stented before accessing the side branch through the main branch stent struts and a second stent is deployed in the side branch. This second stent extends back into the main branch stent. The main branch is then reaccessed through the side branch stent strut and both stents are kissing ballooned to complete the procedure, which allows flaring of the small protrusion. | |||
====Kissing Stent Technique==== | |||
This involves simultaneous stent deployment in parent and side branch vessels in parallel. This technique is useful in lesions that are difficult to cross, as wires do not need to be removed and lesions are not re-crossed. However, overdilation of the bifurcation carina may occur. | |||
====V-stenting and Y stenting==== | |||
These are used when the stenosis is limited to the ostium of the side branch and the main vessel distal to the side branch. In V-stenting, stents are deployed simultaneously without either stent extending proximally enough to cover the other. Y stenting is when an additional stent is placed proximally in the main branch. | |||
====Crush Technique==== | |||
=====Standard Crush Stenting===== | |||
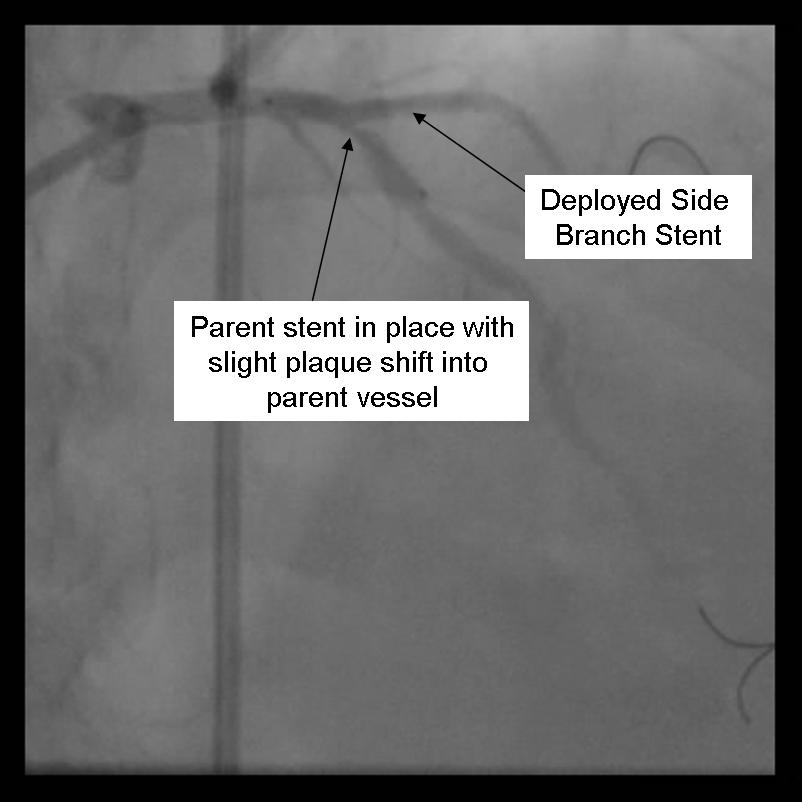
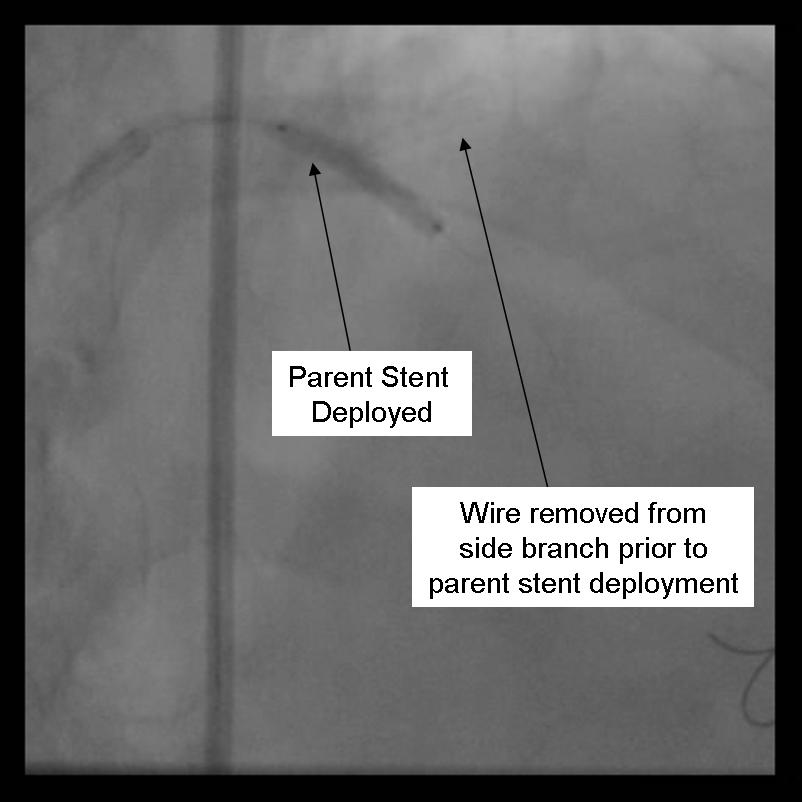
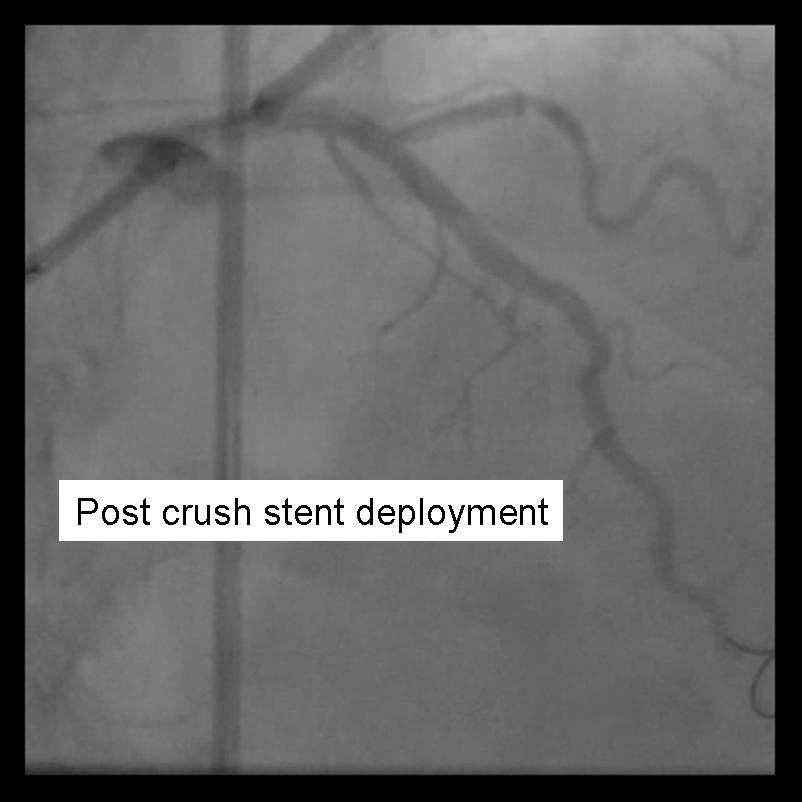
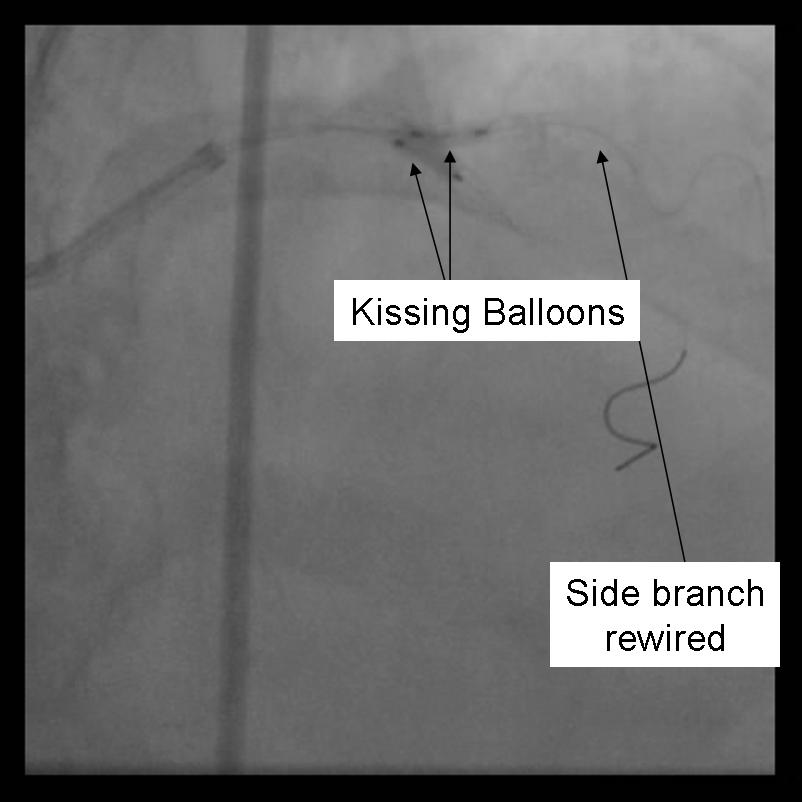
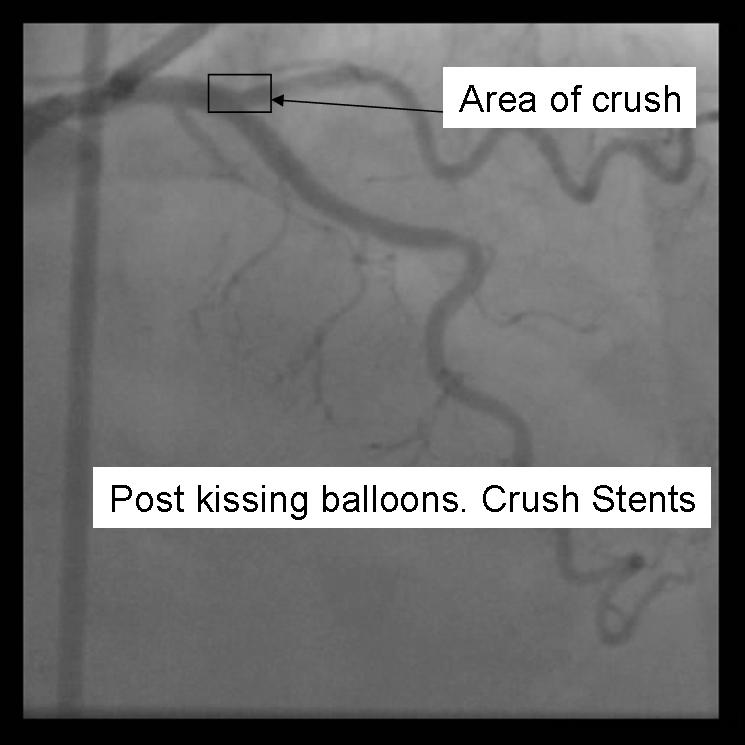
Two stents are deployed with the side branch stent prior to main branch stent. The standard crush technique involves positioning both stents simultaneously. Next, the side branch stent is deployed and both the stent-delivery system and side branch guidewire are withdrawn. The main branch stent is then deployed – crushing the portion of the side branch stent in the parent vessel into the vessel wall. In such a case, the main branch proximal to the bifurcation lesion is scaffolded with a triple layer of stent. The side branch may then be re-wired and kissing balloon inflations employed in both vessels. This technique ensures stent coverage in the origin of the side branch and protects functional side branches during main branch stenting, however re-wiring and re-inflating balloons makes the procedure more technically challenging and time-consuming. | |||
=====Inverse Crush Stenting===== | |||
The inverse crush approach is similar to the standard crush approach, however, there are a few differences. The side branch stent is positioned more proximally than the parent vessel stent, the parent vessel stent is deployed first, and then it is crushed by the side branch stent when it is deployed. The main branch is then re-wired and kissing balloon inflations are employed. Hoye and colleagues found that the crush technique was effective with low rates of target lesions [[revascularization]] and major adverse cardiac events (MACE) except in left main disease. They also noted that final kissing balloon inflation significantly decreased side branch [[restenosis]] rates. Furthermore, a study using registry data in Canada found that patients treated with the crush technique had decreased rates of MACE and [[angina]] compared to those patients with just main branch treatment. | |||
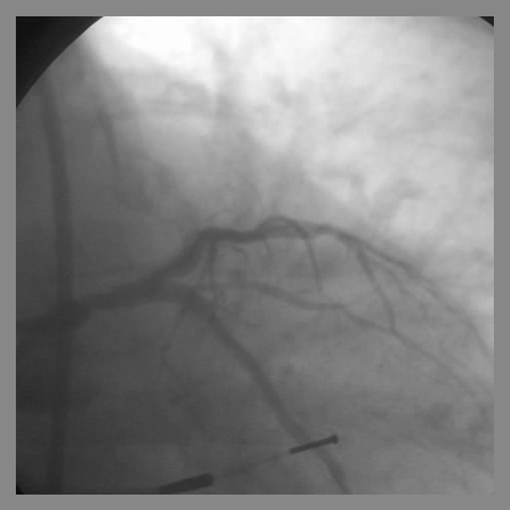
[[Image:Image1.jpg | Bifurcation Stenting Techniques]] | [[Image:Image1.jpg | Bifurcation Stenting Techniques]] | ||
Revision as of 16:13, 28 July 2010
| Cardiology Network |
 Discuss Coronary artery bifurcation further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Template:WikiDoc Cardiology News Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editors-In-Chief: Lisa Battaglia, M.D.; Xin Yang, M.D.; Michael C. Nguyen, M.B.B.S.
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Bifurcation lesions in coronary artery disease (CAD) are common, encompassing 15-18% of lesions treated with percutaneous coronary intervention (PCI). The optimal treatment for these lesions is subject to intense debate and current practice includes a variety of approaches.
The goal of PCI in the bifurcation lesion is to:
- Maximize flow in both the parent vessel while maintaining flow in the side branch
- Prevent side branch occlusion or compromise
- Maximize long-term patency of both parent vessel and side branch
Classification of Bifurcation Lesions
Bifurcation lesions are classified according to the angulation of the bifurcation and plaque burden. This will determine the ease of access to the side branch, plaque shift, and hence the preferred treatment strategy.
Several classifications have been proposed over the years to help better define the anatomy in bifurcation lesions. The original schemes published by Samborn, Safian, Lefevre and Duke are similar in their approach of using numbers or letters to represent various lesion types. However the absence of intuitive correlations between the various lesion type and associated classifications makes it difficult to remember and apply these classifications in routine clinical practices.
Medina et al. subsequently published their classification which assigns a suffix of 1 (diseased) or 0 (not diseased) to the proximal main branch, side branch and distal main branch, respectively. This classification allows for easy remembrance and it has since become the most commonly used scheme for defining anatomy of bifurcation lesions.
Technical Considerations
The operator needs to consider the following when formulating a strategy:
- How important is the side branch?
- Is there a significant lesion at the origin of the side branch?
- Will the angle of the side branch make directing a wire into it difficult and thereby complicate a side branch "rescue" procedure?
- Is there a significant plaque volume at the bifurcation?
- Is a two stent strategy neccessary?
Risks of Side Branch Involvement in Main Vessel Interventions
Early studies demonstrated that the occlusion of a side branch (with or without baseline disease in the side branch) during coronary angioplasty led to a higher rate of peri-procedural myocardial infarction (MI).
In the stent era, the use of angioplasty in a compromised side branch can lead to stent deformation in the main branch. Studies have also demonstrated that patients undergoing PCI of a main vessel were at an increased risk for a MI within 30 days of their procedure if the stent compromised a side branch.
Goals of Treatment
Three major goals of treating bifurcation lesions include:
- Maximize flow in the parent vessel, while also maintaining flow in the sidebranch
- Prevent side branch occlusion or compromise
- Maximize long-term patency of both the parent vessel and side branch
Overview of Treatment Choices
PTCA
- Double guidewire followed by sequential PTCA
- Kissing balloon dilation (i.e.: simultaneous balloon inflations)
Debulking
- Directional coronary atherectomy (DCA)
- Rotational atherectomy (RA)
Stenting
Single Stent Technique
The single stent technique (also known as “provisional stenting”) is most commonly adopted. It involves stenting the main branch and then rescuing the side branch with either balloon angioplasty or stenting if necessary.
T-stent Technique
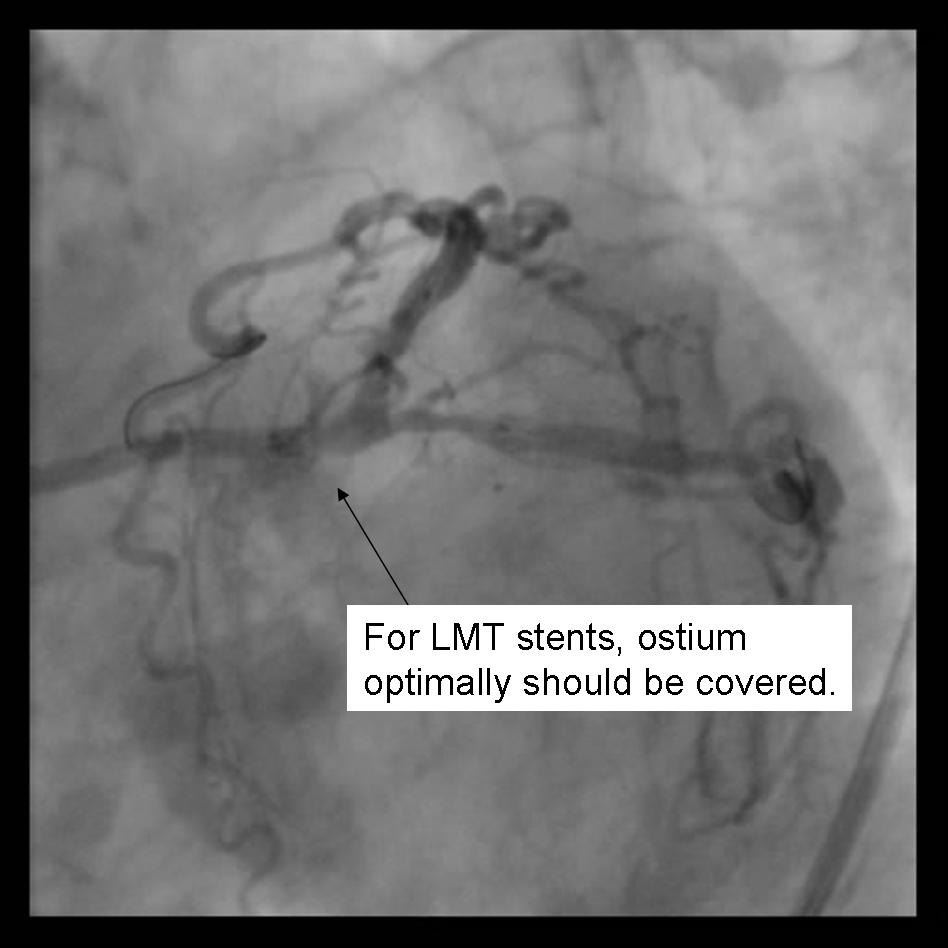
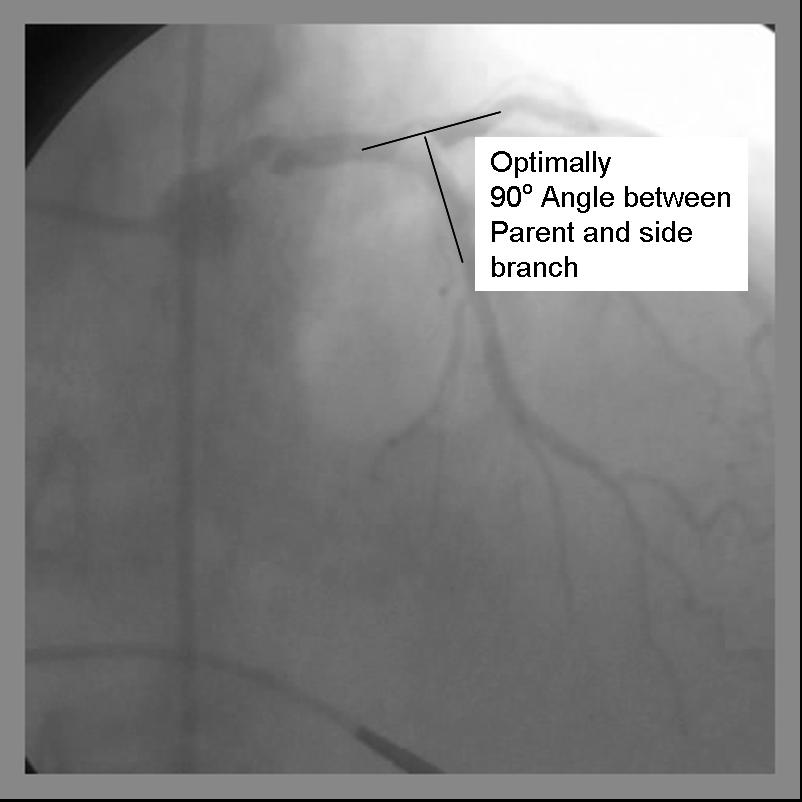
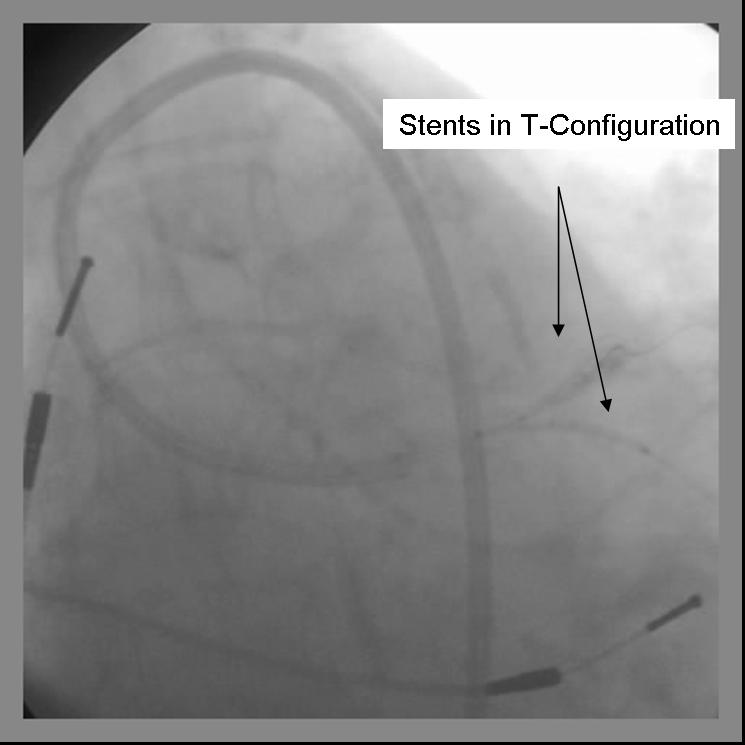
This involves stenting the side branch first to cover the ostium and then stenting the main branch. This approach can be difficult if the angle of the side branch is not 90 degrees and thus not allowing perfect alignment of the two stents. In this situation, there will either be side branch stent strut protruding into the main vessel or incomplete coverage of the side branch ostium.
The modified T-stent approach (also known as “blocking balloon technique”) positions the side branch stent followed by a balloon placed in the main branch at the bifurcation. The main branch balloon is inflated first at low pressure to provide support against which the side branch stent can be aligned more accurately to cover the ostium without protruding. The side branch stent is then deployed followed by main branch stent deployment.
In the TAP (T and small protrusion) technique, the main branch is stented first, and then the side branch is reaccessed and redilated. The side branch stent is then placed with a small amount of strut protruding into the main branch. A main branch blocking balloon is then inflated simultaneously with the side branch stent.
Culotte/Trousers Technique
If necessary, both the main branch and side branch are first wired with pre-dilation to allow for better access. The parent vessel is then stented before accessing the side branch through the main branch stent struts and a second stent is deployed in the side branch. This second stent extends back into the main branch stent. The main branch is then reaccessed through the side branch stent strut and both stents are kissing ballooned to complete the procedure, which allows flaring of the small protrusion.
Kissing Stent Technique
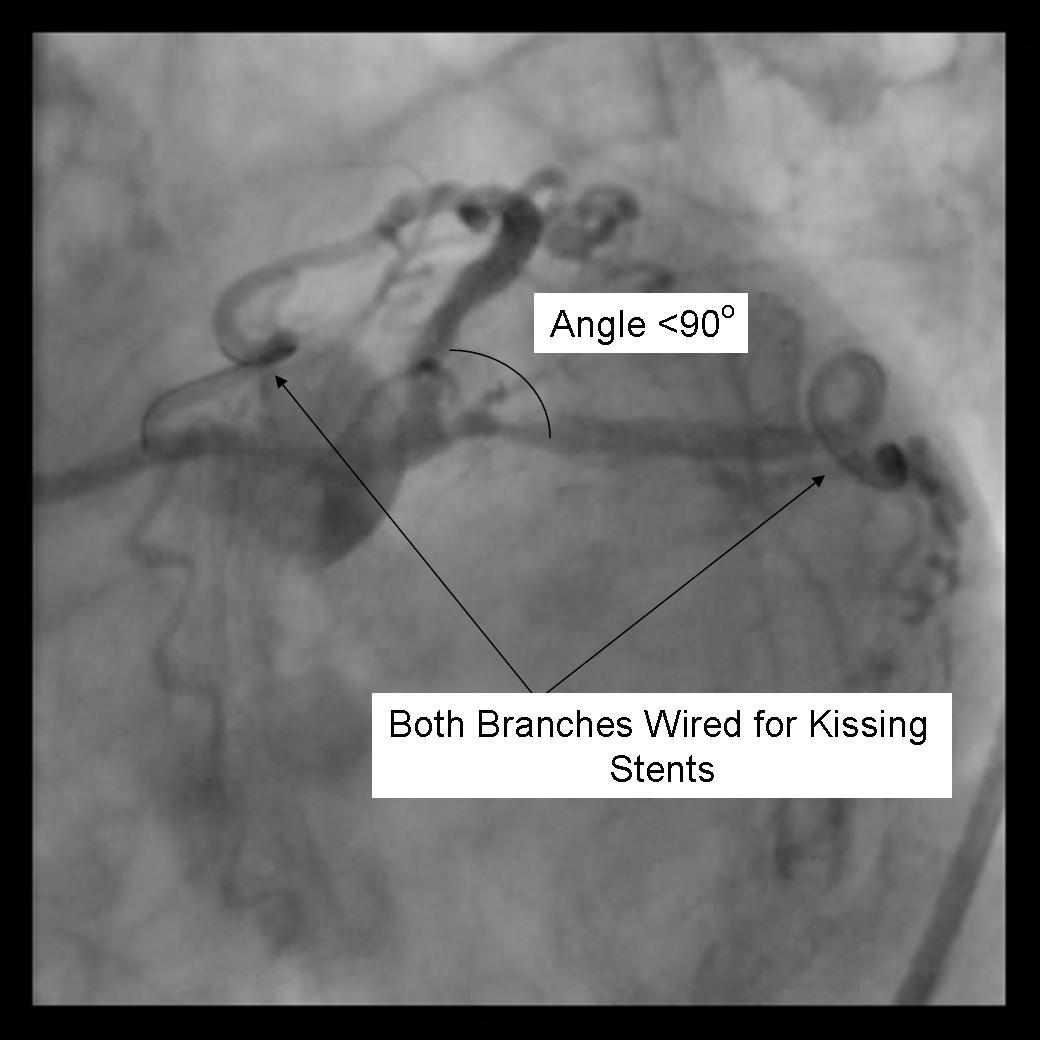
This involves simultaneous stent deployment in parent and side branch vessels in parallel. This technique is useful in lesions that are difficult to cross, as wires do not need to be removed and lesions are not re-crossed. However, overdilation of the bifurcation carina may occur.
V-stenting and Y stenting
These are used when the stenosis is limited to the ostium of the side branch and the main vessel distal to the side branch. In V-stenting, stents are deployed simultaneously without either stent extending proximally enough to cover the other. Y stenting is when an additional stent is placed proximally in the main branch.
Crush Technique
Standard Crush Stenting
Two stents are deployed with the side branch stent prior to main branch stent. The standard crush technique involves positioning both stents simultaneously. Next, the side branch stent is deployed and both the stent-delivery system and side branch guidewire are withdrawn. The main branch stent is then deployed – crushing the portion of the side branch stent in the parent vessel into the vessel wall. In such a case, the main branch proximal to the bifurcation lesion is scaffolded with a triple layer of stent. The side branch may then be re-wired and kissing balloon inflations employed in both vessels. This technique ensures stent coverage in the origin of the side branch and protects functional side branches during main branch stenting, however re-wiring and re-inflating balloons makes the procedure more technically challenging and time-consuming.
Inverse Crush Stenting
The inverse crush approach is similar to the standard crush approach, however, there are a few differences. The side branch stent is positioned more proximally than the parent vessel stent, the parent vessel stent is deployed first, and then it is crushed by the side branch stent when it is deployed. The main branch is then re-wired and kissing balloon inflations are employed. Hoye and colleagues found that the crush technique was effective with low rates of target lesions revascularization and major adverse cardiac events (MACE) except in left main disease. They also noted that final kissing balloon inflation significantly decreased side branch restenosis rates. Furthermore, a study using registry data in Canada found that patients treated with the crush technique had decreased rates of MACE and angina compared to those patients with just main branch treatment.
Advantages and Disadvantages of Each Choice
Stent Parent and PTCA of Side Branch
Recent studies (Nordic Bifurcation study) have shown that a strategy of provisional stenting in the parent artery with rescue balloon inflation of the side branch reduces procedure time, fluoroscopy time and contrast use and procedure related biomarker release compared with a two stent strategy.
DCA
Older studies suggested less revascularization and restenosis rates & higher success rates with DCA compared to PTCA, but DCA is associated with more ischemic complications.
T Stenting
The stent in the side branch may not adequately cover the side branch ostium or alternatively it may protrude into parent vessel with T stenting, especially if the lesion is angulated.
Kissing Stents
In difficult-to-cross lesions, kissing stents may be preferred. The wires need not be removed and the side branch and parent lesions need not be recrossed. A disadvantage is the potential for overdilation of bifurcation carina.
Stent Crush
Crush stenting techniques ensure stent coverage in the origin of the side branch but studies suggest possible increase stent thrombosis as well as high target lesion restenosis and major adverse cardiac events in the setting of left main stenting and among patients with multivessel disease.
Selecting a Strategy
- Decision whether to stent compromised side branch based on size of vessel, amount of jeopardized myocardium, & probability of repeat revascularization
- Side branch protection with a guidewire should be considered for any vessel >2.0 mm; in addition, if >50% stenosis of side branch is present, risk of side branch occlusion is >25% after dilation of parent vessel, & difficulty wiring vessel will be high
- If side branch is <1.5 mm or small amount of viable myocardium is supplied, side branch protection not usually necessary
- Kissing balloon inflations prevent plaque from prolapsing from one vessel to the other
- RA & PTCA may be performed for late ostial side branch stenosis, but there is increased risk of burr entrapment if stent struts have not been dilated w/ previous PTCA
- Sequential balloon inflation as opposed to kissing balloon dilation may lead to shifting plaque & side branch occlusion, but the same balloon may be used to dilate both vessels; parent vessel may remain underexpanded if balloon is sized according to caliber of vessel distal to bifurcation
- T stenting & crush stenting: well suited for branches that originate at 90-degree angles from parent vessel, because coverage of branch ostium is improved in these cases
- T stenting & Y stenting: technically demanding; stent & retrieve technique may be preferred, depending on operator experience
- Isolated side branch ostial stenosis does not require protection of parent vessel
Anticipated Outcomes and Complications
- Successful dilation of the parent vessel can be achieved in >85% of bifurcation lesions, but the success rates in side branch are lower.
- Incomplete dilation and occlusion of side branch can occur.
- Retrograde propagation of a dissection from the side branch into the parent vessel can occur.
- Freshly occluded side branches can be opened successfully in >75% of cases if there is no preexisting disease, but they can be opened in <50% of cases if there is preexisting disease (>50% stenosis).
- Almost 40% of side branches will occlude after debulking w/ DCA in parent vessel, but these usually can be rescued with PTCA.
- Side branch occlusion occurs more common after roational atherectomy if the preexisting side branch ostial stenosis was >50%.
- If the side branch wire is left in place when deploying the stent in the main parent vessel, then there is a risk of jailing the wire. If main parent branch stent extends a signicant length proximal from the side branch (therefore jailing a longer length of wire) then consideration should be given to removing the wire prior to stenting.
Assessing the Outcomes of Bifurcation PCI
- Angiography can confirm prolapse of plaque into side branch after dilation of parent vessel & failure of dilating just the parent
- Hemodynamic decompensation, arrhythmia, ST elevation, or chest pain may signify side branch occlusion
- Side branch occlusion may be silent, especially in presence of collaterals
When to Change Strategies
- Consider terminating procedure if small side branch cannot be crossed and the patient is hemodynamically stable
- Inadequate dilation or inability to cross with the guidewire or balloon may necessitate equipment change.
Technical Considerations
- Before beginning the procedure, larger guiding catheters (i.e.: at least 7 French) should be inserted as they are required for complex bifurcation stenting in order to accommodate the additional equipment however 6F guiding catheters can be used for kissing balloon inflations.
- If balloon-on-wire devices used (Ace balloon), guidewire position may be lost if upsizing or exchange becomes necessary
- Consideration should also be given to using a hydrophylic wire for easier wire removal if the wire becomes jailed.
Detailed Discussion of Specific Techniques
The Crush Technique
Benefits
Ensures complete coverage of the side branch ostium Immediate patency of parent and side branch Excellent immediate angiographic results Restenosis is usually very focal [1]
Detriments
- 3 Layers of stent in the main artery
- Without final kissing balloon inflation high Restenosis rate
- May be difficult to re-cross side branch
- Minimal 7F guide system required
Technical Considerations
- Requires minimum of a 7F Guiding system
- Final Kissing balloon inflation required due to high Restenosis rate
Technique
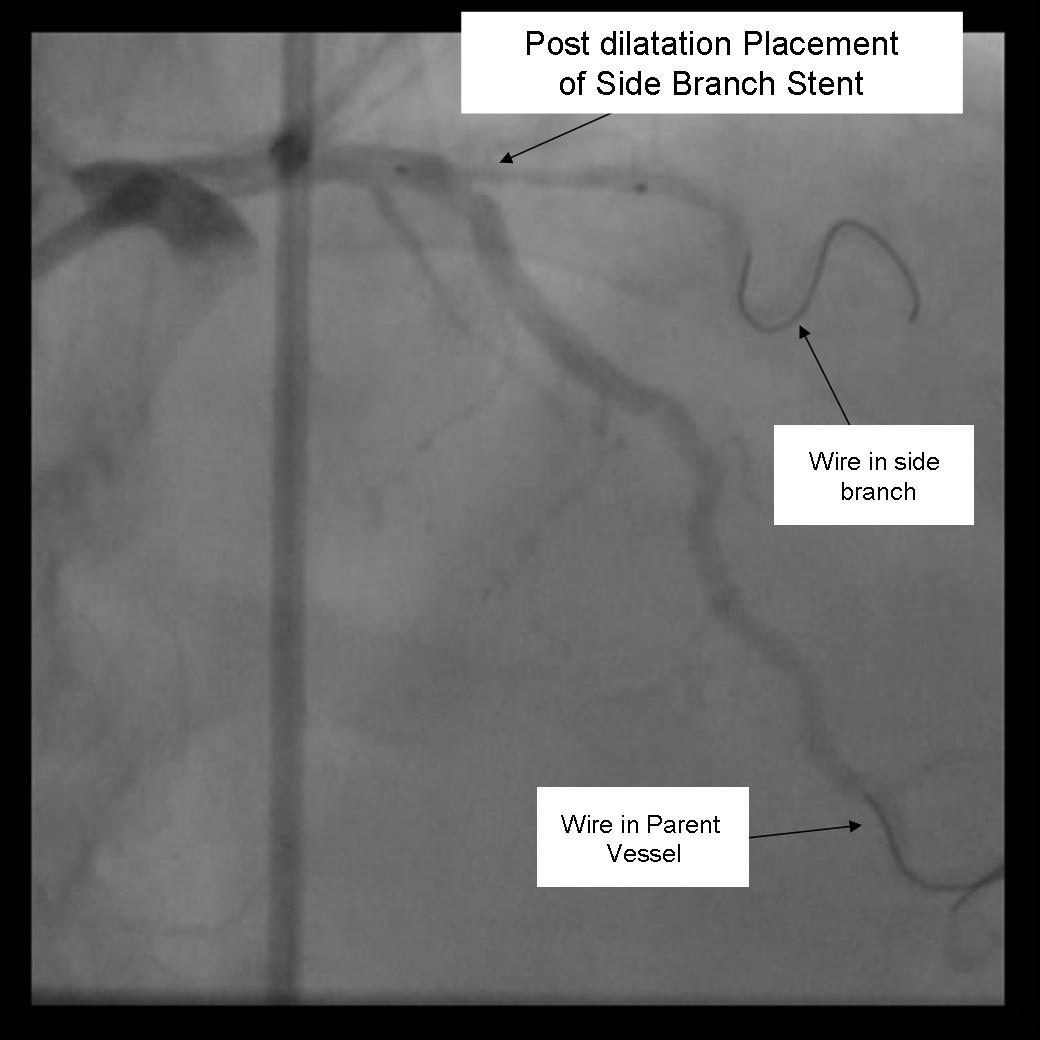
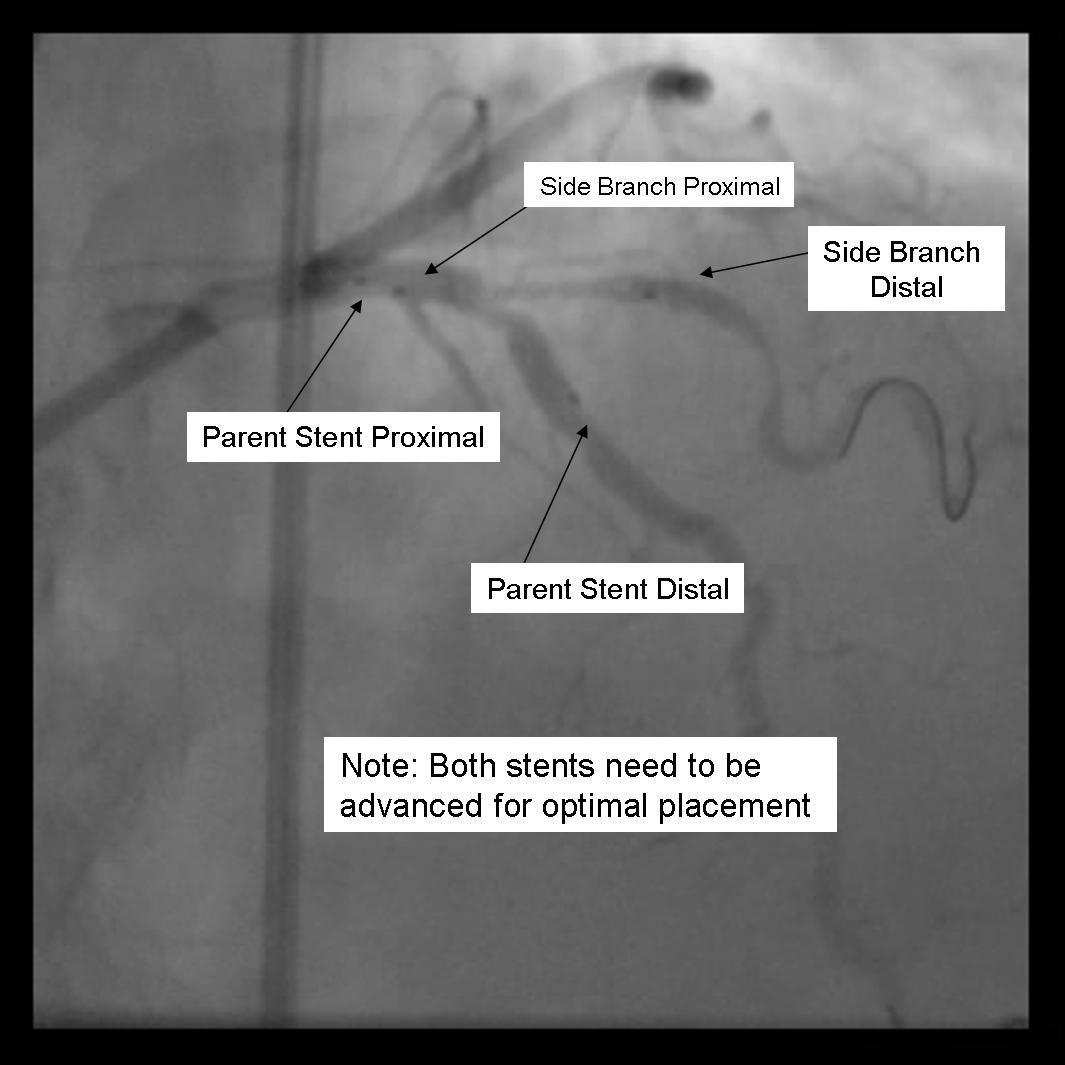
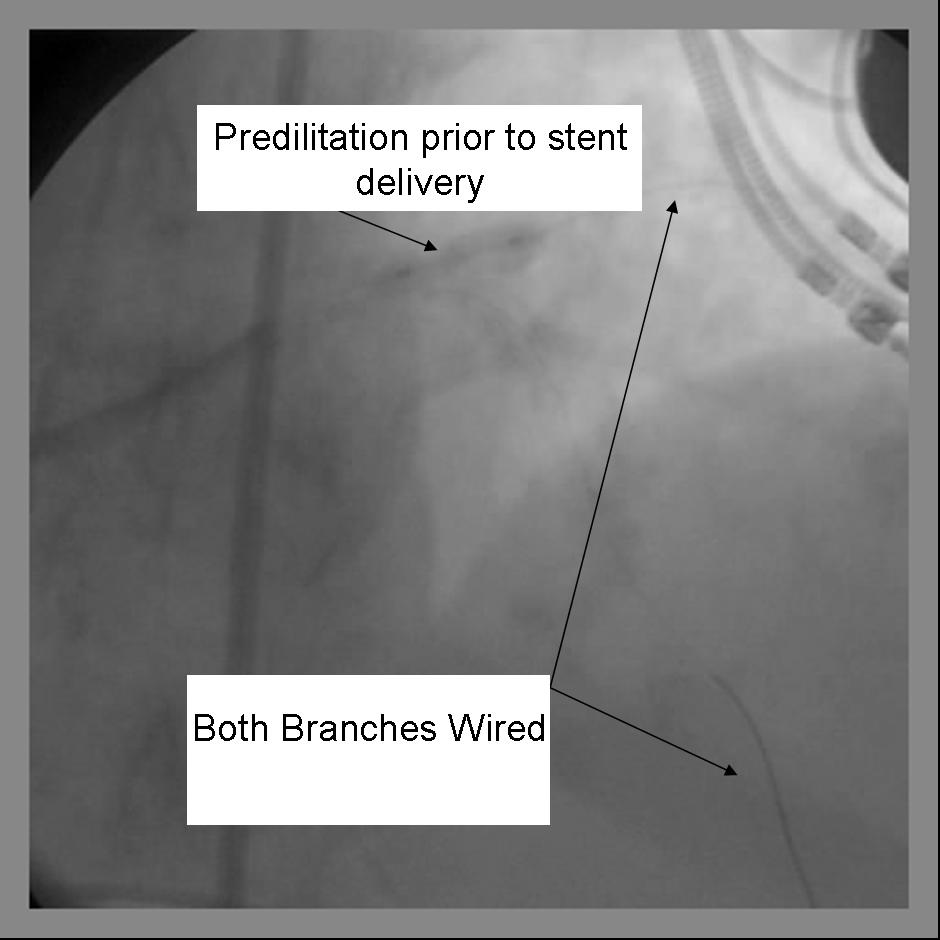
- Using a minimum 7F guide system, both the parent and side branch are wired. Predilation is recommended to ensure optimal balloon expansion and ease stent delivery. It is important to identify which wire is placed in which branch. We recommend either using 2 separate colored guide wires, keeping a marker on 1 wire, or covering a wire with a sterile towel while not in use.
- Any disease distal to the side branch should optimally be repaired before the final crush step.
- The 1st stent is advanced into the side branch. This may require further predilitation. Generally, the stent is advanced beyond the delivery point.
 |
<googlevideo>-6644364110521967374&hl=en</googlevideo> |
- The 2nd stent is advanced into the parent vessel. This is also placed beyond the intended deployment site.
- The side branch stent is pulled back into the parent vessel about 5 mm. This ensures adequate coverage of the ostium.
- The parent stent is pulled back crossing the side branch and the proximal end is placed proximal to the proximal end of the side branch stent.
 |
<googlevideo>-2384934812388551194&hl=en</googlevideo> |
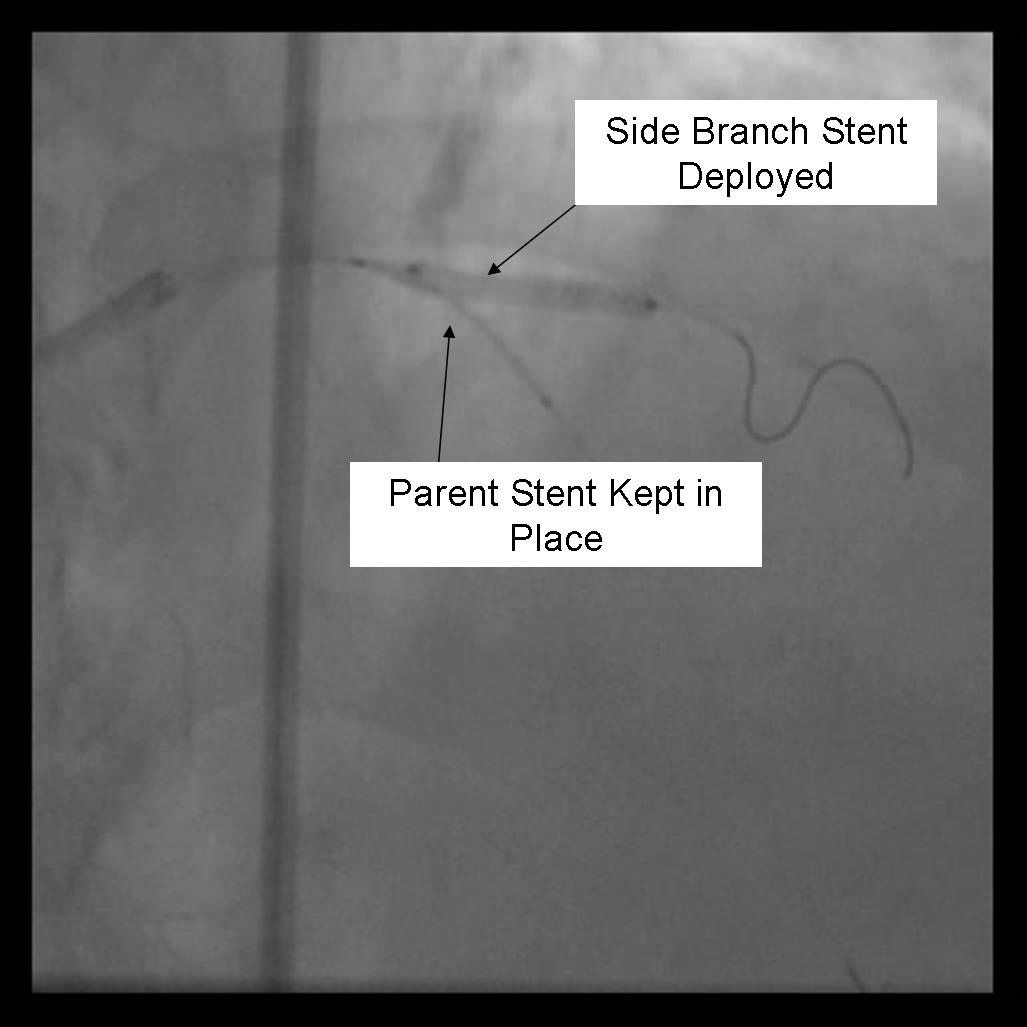
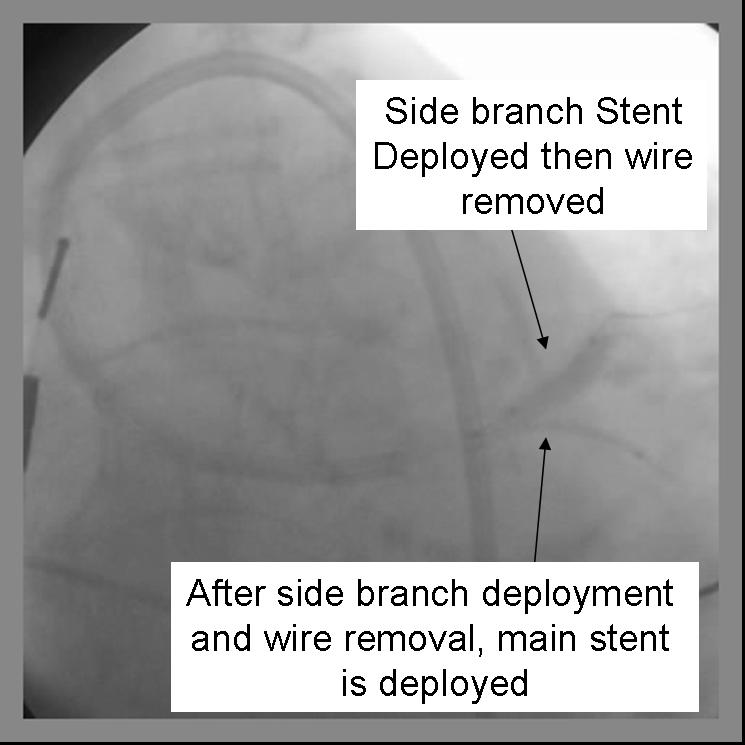
- The side branch stent is deployed.
 |
<googlevideo>-2225481000332319520&hl=en</googlevideo> |
- Angiography should now be performed to ensure adequate side branch coverage and stent deployment. Distal edge dissections or disease should be addressed before parent stent deployment. Once complete, the side branch wire is removed.
 |
<googlevideo>6608019255966212549&hl=en</googlevideo> |
- The parent stent is deployed.
 |
<googlevideo>5013022603317484197&hl=en</googlevideo> |
 |
<googlevideo>2049938197341162787&hl=en</googlevideo> |
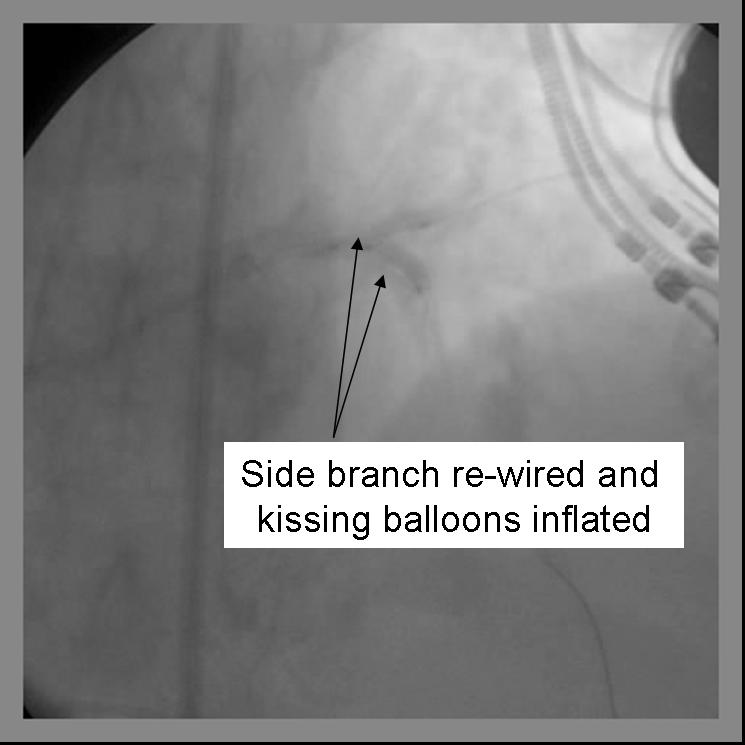
- The side-branch is rewired. It is sometimes necessary to change wires to either a hydrophilic wire eg. Whisper, or Pilot 50 or 150, or ASAHI Fielder, one of increasing stiffness e.g. ASAHI Miracle Bros 3, or both e.g. Shinobi or Confienza.
- Kissing balloons are inflated at the bifurcation. It is sometimes necessary to dilate the side branch with a small balloon (1.5 mm middle marker balloon) to facilitate a larger balloon for the kissing technique.
 |
<googlevideo>-3998349476747507559&hl=en</googlevideo> |
- Repeat angiography is performed. Wires are removed and final angiography completed.
 |
<googlevideo>9148159160696936306&hl=en</googlevideo> |
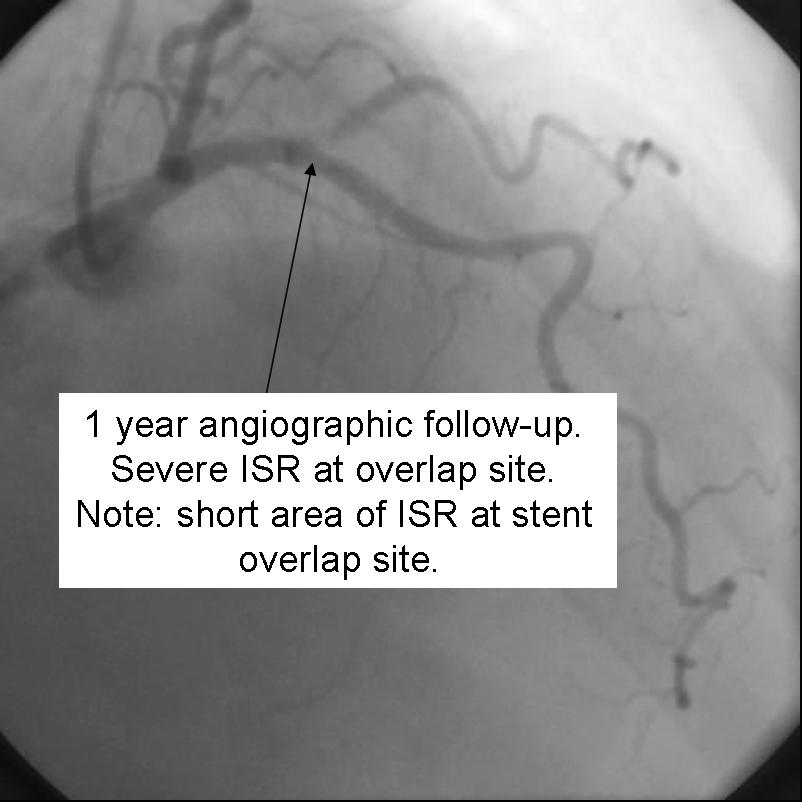
Despite excellent initial angiographic results, side branch restenosis is still a significant problem with Crush stenting(Up to 25% without kissing ballon inflation). However,most of the restenosis is silent. The above example used Cypher drug eluting stents in the Side branch and Parent vessels. The patient returned with positive stress testing 13 months later. Repeat angiography demonstrated a short segment of significant in-stent restenosis.
 |
<googlevideo>-676433419690470542&hl=en</googlevideo> |
The Kissing Stents Technique
Benefits
- Ensures complete coverage of the side branch ostium
- Immediate patency of parent and side branch
- Access to both branches maintained through procedure
- No need for final kissing balloon
Detriments
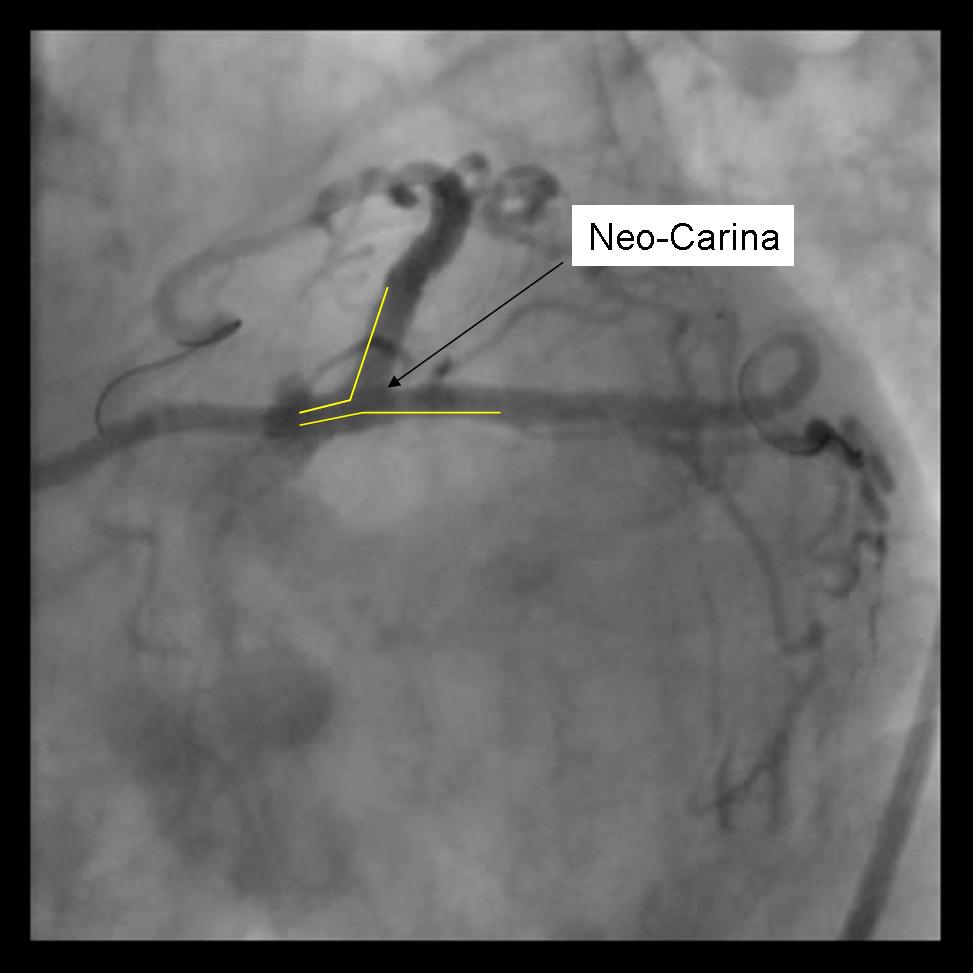
- Unendothelialized layer of stents forming neo-carina may predispose to stent thrombosis.
- 8F Guide system required
- May be difficult to re-access side branch or parent vessel
Technical Considerations
- Requires minimum of a 8F Guiding system
- Optimal angle of bifurcation less than 90 degrees.
Technique
- Using a minimum 8F guide system, both the parent and side branch are wired. Predilation is recommended to ensure optimal balloon expansion and ease stent delivery. It is important to identify which wire is placed in which branch. Either using 2 separate colored guide wires, keeping a marker on 1 wire, or covering a wire with a sterile towel while not in use are recommended.
 |
<googlevideo>1873623062002840911&hl=en</googlevideo> |
- Any disease distal to the side branch or parent vessel should optimally be repaired before the kissing stents are deployed.
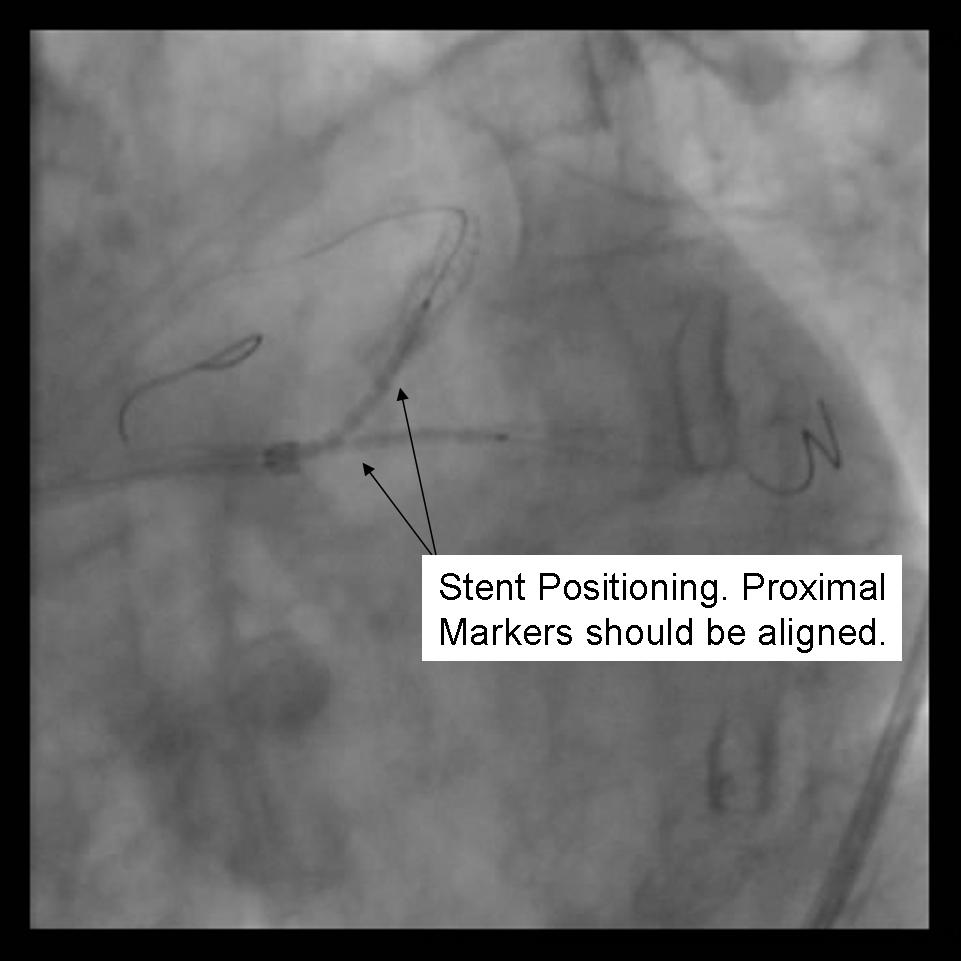
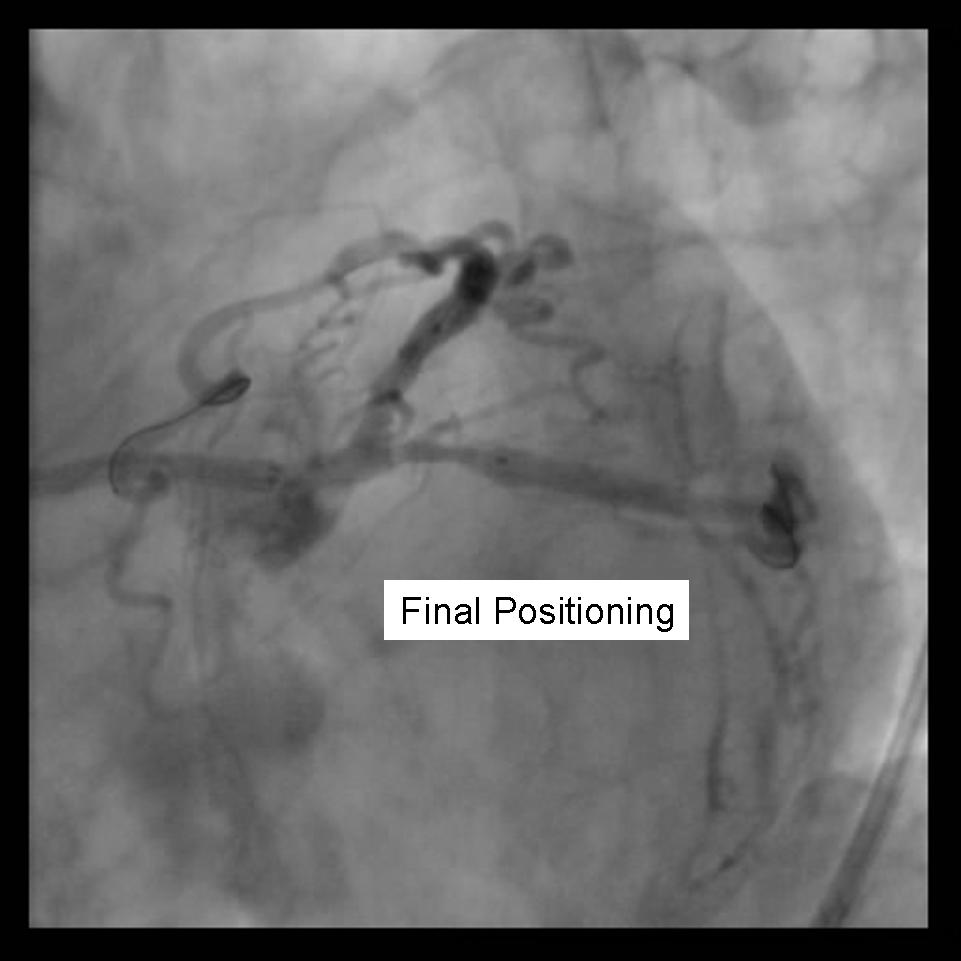
- Both stents are advanced into the side branch and parent vessel. This may require further predilitation. Generally, the stents are advanced beyond the delivery point. Operator preference differs with respect to amount of overlap. Some operators form a long segment of overlap (>5mm), while others try to minimize overlap. It is absolutely essential that both vessels are covered during the balloon inflation. Optimal placement is ensured by advancing both stents distal to the intended deployment site then pulling them back into position. The proximal marker segements should be aligned, with positional confirmation in at least 2 separate views.
 |
<googlevideo>-2198706559365896519&hl=en</googlevideo> |
 |
<googlevideo>6739334144213459915&hl=en</googlevideo> |
- Using 2 Insufflators, both stents are inflated to low pressure. Then alternating with side branch and parent branch inflated to optimal deployment size. There is some risk of
over sizing the main branch with the overlapping stent segments. In the case where proximal disease may interfere with the 2 overlapping stents, a proximal stent may be deployed prior to inflating the 2 distal stents. (Pants-and-trousers technique)
 |
<googlevideo>6739334144213459915&hl=en</googlevideo> |
- Angiography should now be performed to ensure adequate side branch coverage and stent deployment. Distal edge dissections or disease should be addressed before wire removal \
from the vessels.
 |
<googlevideo>-1540905286545689451&hl=en</googlevideo> |
Variations of this method may be used to stent trifurcation disease. While an 8F catheter can be used depending on the stent system, optimally a 9 F system should be used in this situation.
The T-Stent Technique
Benefits
- May be used for provisional stenting of side branch if angiographic result is poor.
- Can Use 6F guide system
- Restenosis is usually very focal
Detriments
- Very difficult, if not impossible to completely cover side branch ostium
- Requires final kissing balloon inflation
- Modified T-stent technique requires 7F guide system
Technical Considerations
- May use a 6F Guiding system
- Final Kissing balloon inflation required due to high Restenosis rate
- Ideal angle of bifurcation is at or near 90 degrees.
 |
<googlevideo>7259214304163348609&hl=en</googlevideo> |
Technique (Modified T-Stenting)
- A 6F guide system may be used with standard T stenting in which the side branch stent is deployed, followed by delivery and deployment of the parent stent. The modified technique, which is preferred by this operator, requires a minimum of 7F guide system.
- Both the parent and side branch are wired. Predilation is recommended to ensure optimal balloon expansion and ease stent delivery. It is important to identify which wire is placed in which branch. We recommend either using 2 separate colored guide wires, keeping a marker on 1 wire, or covering a wire with a sterile towel while not in use.
 |
<googlevideo>-8290939644314628088&hl=en</googlevideo> |
- Any disease in the distal side branch or parent vessel should optimally be repaired before the bifurcation stents are deployed.
- The 1st stent is advanced into the side branch. This may require further predilatation. Generally, the stent is advanced beyond the delivery point.
- The 2nd stent is advanced into the parent vessel and placed across the side branch.
 |
<googlevideo>-8176401098564532983&hl=en</googlevideo> |
- The side branch stent is deployed. (Another option is to place a balloon in the parent branch and inflating to low atm while pulling the side branch back. This may help ensure adequate coverage of the ostium.
- Side branch wire is removed once adequate angiographic result confirmed.
- The parent stent is deployed across the side branch.
 |
<googlevideo>4485530437540579771&hl=en</googlevideo> |
- Angiography should now be performed to ensure adequate side branch coverage and stent deployment. The parent stent is deployed.
- The side-branch is rewired. It is sometimes necessary to change wires to either a hydrophilic wire e.g. Whisper, or Pilot 50 or 150, or Fielder, one of increasing stiffness e.g. ASAHI Miracle Bros 3, or both e.g. Shinobi or Confienza.
- Kissing balloons are inflated at the bifurcation. It is sometimes necessary to dilate the sidebranch with a small balloon (1.5 mm middle marker balloon) to facilitate a larger balloon for the kiss.
 |
<googlevideo>4382003640399583914&hl=en</googlevideo> |
- Repeat angiography is performed. Wires are removed and final angiography completed.
 |
<googlevideo>-2232340403491043434&hl=en</googlevideo> |
- Provisional T-Stenting involves the stenting the parent vessel and only the side branch if there is less than adequate side branch angiographic result. In this situation, the side branch may need to be serially dilated with up to a 2.5 mm balloon to ensure stent delivery. Final kissing balloons should be repeated.
- Sometimes the side branch stent impinges on the parent lumen making delivery of the parent stent impossible. If this happens, dilation of the parent lumen with a balloon allows for stent delivery. This may create a partial or small area of crushed stents at the bifurcation and should be followed with kissing balloons.
References
- ↑ Nordic bifurcation study PMID 17060387