Contrast induced nephropathy primary prevention: Difference between revisions
Rim Halaby (talk | contribs) |
|||
| (33 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Many strategies have aimed at preventing CIN. Non-therapeutic measures include '''smaller doses of contrast''' and use of '''low-osmolar or iso-osmolar agents'''. | |||
==Prevention== | ==Prevention== | ||
===Non-Pharmacologic Approaches=== | ===Non-Pharmacologic Approaches=== | ||
====Dose of contrast media==== | ====Dose of contrast media==== | ||
The 2012 [[clinical practice guideline]]s by [http://kdigo.org/ KDIGO] recommended using the smallest possible dose in every procedure requiring IV contrast especially in patients at high risk for developing CIN.<ref name="pmid25018920">{{cite journal|author=Kidney Disease Improving Global Outcomes Work Group| title=2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury| journal=Kidey Int Supp |year= 2012 | volume= 2 | pages= 69-88 | doi=10.1038/kisup.2011.34 | pmc= |url=http://www.nature.com/kisup/journal/v2/n1/full/kisup201134a.html }} </ref> Nyman et al suggested an alternative approach, using the ratio of dose of iodine (in grams) to estimated glomerular filtration rate (eGFR). The team found the ratio to be predictive of the risk of CIN. A ratio '''I<sub>(g)</sub>/eGFR < 1''' was shown to be relatively safe even in patients with many possible risk factors. The estimated risk decreased eightfold when the ratio dropped below 1.<ref name="pmid18568558">{{cite journal| author=Nyman U, Björk J, Aspelin P, Marenzi G| title=Contrast medium dose-to-GFR ratio: a measure of systemic exposure to predict contrast-induced nephropathy after percutaneous coronary intervention. | journal=Acta Radiol | year= 2008 | volume= 49 | issue= 6 | pages= 658-67 | pmid=18568558 | doi=10.1080/02841850802050762 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18568558 }} </ref> | |||
====Route of Administration==== | ====Route of Administration==== | ||
| Line 17: | Line 16: | ||
====Osmolarity of Contrast Agent==== | ====Osmolarity of Contrast Agent==== | ||
The | The [[clinical practice guideline]]s from 2012 by [http://kdigo.org/ KDIGO] advocate the use of either iso-osmolar or low-osmolar iodinated contrast media, rather than high-osmolar media particularly in patients at increased risk of CIN.<ref name="pmid25018920">{{cite journal|author=Kidney Disease Improving Global Outcomes Work Group| title=2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury| journal=Kidey Int Supp |year= 2012 | volume= 2 | pages= 69-88 | doi=10.1038/kisup.2011.34 | pmc= |url=http://www.nature.com/kisup/journal/v2/n1/full/kisup201134a.html }} </ref> | ||
More recently: | |||
* A more recent [[randomized controlled trial]] found no difference in frequency of nephropathy between iso and low osmolar contrast agents.<ref name="pmid26830055">{{cite journal| author=Eng J, Wilson RF, Subramaniam RM, Zhang A, Suarez-Cuervo C, Turban S et al.| title=Comparative Effect of Contrast Media Type on the Incidence of Contrast-Induced Nephropathy: A Systematic Review and Meta-analysis. | journal=Ann Intern Med | year= 2016 | volume= 164 | issue= 6 | pages= 417-24 | pmid=26830055 | doi=10.7326/M15-1402 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26830055 }} </ref> | |||
{| | {| | ||
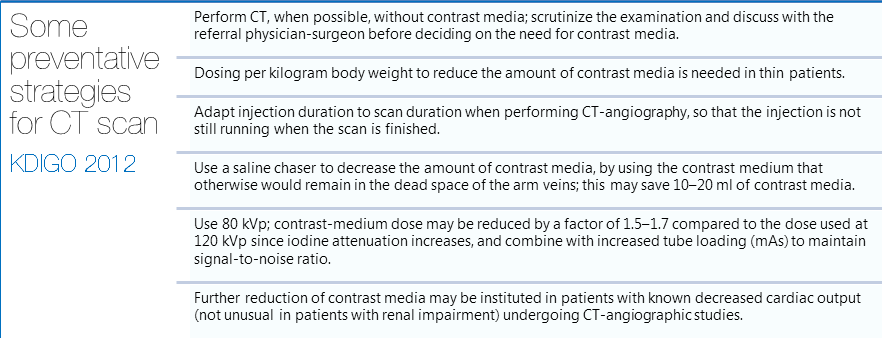
| [[File: | | [[File:Preventative_strategies_CT_KDIGO2012.png|thumb|608px|center|Preventative Strategies in CT scan - Click to Enlarge]] | ||
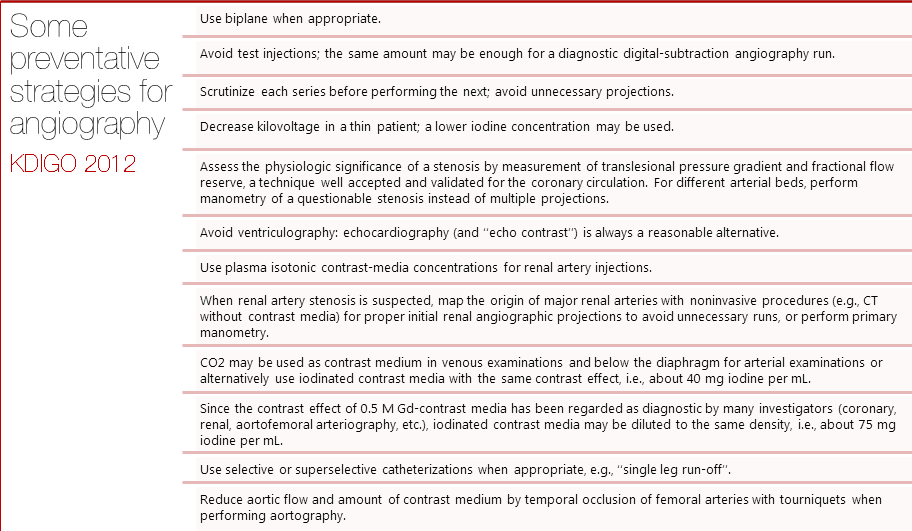
| [[File: | | [[File:Preventative_strategies_angiography_KDIGO2012.png|thumb|400px|center|Preventative Strategies in Angiography - Click to Enlarge]] | ||
|} | |} | ||
| Line 29: | Line 31: | ||
===Pharmacologic Approaches=== | ===Pharmacologic Approaches=== | ||
==== | ====Volume Expansion==== | ||
The mechanisms by which volume expansion decrease the risk of CIN may include dilution of the contrast media, increase in renal prostaglandins, counteraction of altered renal hemodynamics, and inhibition of the renin-angiotensin system. | |||
[[Clinical practice guideline]]s from 2012 by [http://kdigo.org/ KDIGO] recommend '''fluid administration should be initiated 1-2 h intravenously before and maintained for 3–6 hours after contrast exposure'''.<ref name="pmid25018920">{{cite journal|author=Kidney Disease Improving Global Outcomes Work Group| title=2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury| journal=Kidey Int Supp |year= 2012 | volume= 2 | pages= 69-88 | doi=10.1038/kisup.2011.34 | pmc= |url=http://www.nature.com/kisup/journal/v2/n1/full/kisup201134a.html }} </ref> | |||
More recently: | |||
* [[Sodium bicarbonate]] was found beneficial by a [[meta-analysis]] of patients with pre-existing renal insufficiency.<ref name="pmid25783425">{{cite journal| author=Zhang B, Liang L, Chen W, Liang C, Zhang S| title=The efficacy of sodium bicarbonate in preventing contrast-induced nephropathy in patients with pre-existing renal insufficiency: a meta-analysis. | journal=BMJ Open | year= 2015 | volume= 5 | issue= 3 | pages= e006989 | pmid=25783425 | doi=10.1136/bmjopen-2014-006989 | pmc=PMC4368906 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25783425 }} </ref> The 2012 KDIGO guidelines did not recommend against the use of bicarbonate stating possible benefit but inconsistent data. | |||
* Among patients undergoing cardiac catheterization, dosing the amount of fluid based on the left ventricular end-diastolic pressure is beneficial.<ref name="pmid24856027">{{cite journal| author=Brar SS, Aharonian V, Mansukhani P, Moore N, Shen AY, Jorgensen M et al.| title=Haemodynamic-guided fluid administration for the prevention of contrast-induced acute kidney injury: the POSEIDON randomised controlled trial. | journal=Lancet | year= 2014 | volume= 383 | issue= 9931 | pages= 1814-23 | pmid=24856027 | doi=10.1016/S0140-6736(14)60689-9 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24856027 }} </ref> | |||
====N-acetylcysteine==== | |||
N-acetylcyteine (NAC) is a mycolytic agent and an antioxidant used in the treatment of acetaminophen overdose. | |||
[[Clinical practice guideline]]s by KDIGO from 2012 recommend '''NAC along with isotonic crystalloids'''.<ref name="pmid25018920">{{cite journal|author=Kidney Disease Improving Global Outcomes Work Group| title=2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury| journal=Kidey Int Supp |year= 2012 | volume= 2 | pages= 69-88 | doi=10.1038/kisup.2011.34 | pmc= |url=http://www.nature.com/kisup/journal/v2/n1/full/kisup201134a.html }} </ref> | |||
More recently: | |||
* A [[meta-analysis]] suggests "High-dose [[statin]]s plus hydration with or without [[N-acetylcysteine|NAC]] might be the preferred treatment strategy to prevent contrast-induced". <ref name="pmid27707552">{{cite journal| author=Su X, Xie X, Liu L, Lv J, Song F, Perkovic V et al.| title=Comparative Effectiveness of 12 Treatment Strategies for Preventing Contrast-Induced Acute Kidney Injury: A Systematic Review and Bayesian Network Meta-analysis. | journal=Am J Kidney Dis | year= 2016 | volume= | issue= | pages= | pmid=27707552 | doi=10.1053/j.ajkd.2016.07.033 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27707552 }} </ref> Consistent with the meta-analysis<ref name="pmid27707552"/> | |||
* More[[randomized controlled trial]]s found similar outcomes between normal saline (NS) alone, NS with N-acetylcysteine, NS with sodium bicarbonate.<ref name="pmid29130810">{{cite journal| author=Weisbord SD, Gallagher M, Jneid H, Garcia S, Cass A, Thwin SS et al.| title=Outcomes after Angiography with Sodium Bicarbonate and Acetylcysteine. | journal=N Engl J Med | year= 2018 | volume= 378 | issue= 7 | pages= 603-614 | pmid=29130810 | doi=10.1056/NEJMoa1710933 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29130810 }} </ref><ref name="pmid27411777">{{cite journal| author=Turedi S, Erdem E, Karaca Y, Tatli O, Sahin A, Turkmen S et al.| title=The High Risk of Contrast-induced Nephropathy in Patients with Suspected Pulmonary Embolism Despite Three Different Prophylaxis: A Randomized Controlled Trial. | journal=Acad Emerg Med | year= 2016 | volume= 23 | issue= 10 | pages= 1136-1145 | pmid=27411777 | doi=10.1111/acem.13051 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27411777 }} </ref> | |||
Two commonly used regimens are N-acetylcysteine (NAC) 600 mg orally twice daily, one day before the procedure and on the day of the procedure,<ref name="pmid12578487">{{cite journal |author=Kay J, Chow W, Chan T, Lo S, Kwok O, Yip A, Fan K, Lee C, Lam W|title=Acetylcysteine for prevention of acute deterioration of renal function following elective coronary angiography and intervention: a randomized controlled trial |journal=JAMA |volume=289 |issue=5 |pages=553-8 |year=2003 |pmid=12578487}}</ref> or a higher dose of 1200 mg orally twice daily administered in the similarly.<ref name="pmid16807414">{{cite journal |author=Marenzi G, Assanelli E, Marana I, Lauri G, Campodonico J, Grazi M, De Metrio M, Galli S, Fabbiocchi F, Montorsi P, Veglia F, Bartorelli A |title=N-acetylcysteine and contrast-induced nephropathy in primary angioplasty |journal=N Engl J Med |volume=354|issue=26 |pages=2773-82 |year=2006 |pmid=16807414}}</ref>. | |||
===Prophylactic | ====Prophylactic Hemodialysis==== | ||
Considering studies have shown association with estimated GFR and risk of CIN, and given the fact that contrast media can be effectively removed with as little as one session of hemodialysis, many studies have aimed at evaluating the benefit of pre-emptive hemodialysis in patients with underlying renal disease. Studies until recently have had very variable results with some showing lower risk of CIN,<ref name="pmid17825709">{{cite journal| author=Lee PT, Chou KJ, Liu CP, Mar GY, Chen CL, Hsu CY et al.| title=Renal protection for coronary angiography in advanced renal failure patients by prophylactic hemodialysis. A randomized controlled trial. | journal=J Am Coll Cardiol | year= 2007 | volume= 50 | issue= 11 | pages= 1015-20 | pmid=17825709 | doi=10.1016/j.jacc.2007.05.033 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17825709 }} [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18311873 Review in: ACP J Club. 2008 Mar-Apr;148(2):43] </ref><ref name="pmid14523141">{{cite journal| author=Marenzi G, Marana I, Lauri G, Assanelli E, Grazi M, Campodonico J et al.| title=The prevention of radiocontrast-agent-induced nephropathy by hemofiltration. | journal=N Engl J Med | year= 2003 | volume= 349 | issue= 14 | pages= 1333-40 | pmid=14523141 | doi=10.1056/NEJMoa023204 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14523141 }} </ref> some showing no added benefit over saline infusion or NAC,<ref name="pmid16636489">{{cite journal| author=Kawashima S, Takano H, Iino Y, Takayama M, Takano T| title=Prophylactic hemodialysis does not prevent contrast-induced nephropathy after cardiac catheterization in patients with chronic renal insufficiency. | journal=Circ J | year= 2006 | volume= 70 | issue= 5 | pages= 553-8 | pmid=16636489 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16636489 }} </ref><ref name="pmid17180572">{{cite journal| author=Reinecke H, Fobker M, Wellmann J, Becke B, Fleiter J, Heitmeyer C et al.| title=A randomized controlled trial comparing hydration therapy to additional hemodialysis or N-acetylcysteine for the prevention of contrast medium-induced nephropathy: the Dialysis-versus-Diuresis (DVD) Trial. | journal=Clin Res Cardiol | year= 2007 | volume= 96 | issue= 3 | pages= 130-9 | pmid=17180572 | doi=10.1007/s00392-007-0473-4 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17180572 }} </ref> and some even showing a worse outcome following hemodialysis.<ref name="pmid11747848">{{cite journal| author=Vogt B, Ferrari P, Schönholzer C, Marti HP, Mohaupt M, Wiederkehr M et al.| title=Prophylactic hemodialysis after radiocontrast media in patients with renal insufficiency is potentially harmful. | journal=Am J Med | year= 2001 | volume= 111 | issue= 9 | pages= 692-8 | pmid=11747848 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11747848 }} </ref> Given the very conflicting evidence, the eleveated costs, and the difficult logistics, no recommendations can be made about the use of prophylactic hemodialysis for CIN prevention. '''The 2012 KDIGO guidelines recommend against the use of prophylactic hemodialysis stating that use can only be advocated if future studies convincingly show added benefit'''.<ref name="doi10.1038/kisup.2011.34">{{cite journal|author=Kidney Disease Improving Global Outcomes Work Group| title=2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury| journal=Kidey Int Supp |year= 2012 | volume= 2 | pages= 69-88 | doi=10.1038/kisup.2011.34 | pmc=|url=http://www.nature.com/kisup/journal/v2/n1/full/kisup201134a.html }} </ref> | |||
=== | ====Theophylline==== | ||
Interest in theophylline for CIN prophylaxis stems from the association of adenosine with the pathophysiology of CIN in certain studies.<ref name="pmid8731082">{{cite journal| author=Arakawa K, Suzuki H, Naitoh M, Matsumoto A, Hayashi K, Matsuda H et al.| title=Role of adenosine in the renal responses to contrast medium. | journal=Kidney Int | year= 1996|volume= 49 | issue= 5 | pages= 1199-206 | pmid=8731082 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8731082 }} </ref> Theophylline is a methylxanthine previously used for the treatment of asthma that also acts as an adenosine antagonist. Data about the use of theophylline is conflicting and several meta-analysis have shown little to not benefit from the use of theophylline prophylaxis.<ref name="pmid15911721">{{cite journal| author=Bagshaw SM, Ghali WA| title=Theophylline for prevention of contrast-induced nephropathy: a systematic review and meta-analysis. | journal=Arch Intern Med | year= 2005 | volume= 165 | issue= 10 | pages= 1087-93 | pmid=15911721 | doi=10.1001/archinte.165.10.1087 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15911721 }} </ref><ref name="pmid18283206">{{cite journal| author=Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC| title=Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. | journal=Ann Intern Med | year= 2008 | volume= 148 | issue= 4 | pages= 284-94 | pmid=18283206 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18283206 }} </ref> However, more recent studies have shown some significant decrease in the risk of CIN when theophylline was compared to other prophylactic measures notably N-acetylcysteine and bicarbonate.<ref name="pmid16714461">{{cite journal| author=Huber W, Eckel F, Hennig M, Rosenbrock H, Wacker A, Saur D et al.| title=Prophylaxis of contrast material-induced nephropathy in patients in intensive care: acetylcysteine, theophylline, or both? A randomized study. | journal=Radiology | year= 2006 | volume= 239 | issue= 3 | pages= 793-804 | pmid=16714461 | doi=10.1148/radiol.2393041456 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16714461 }} </ref><ref name="pmid19500141">{{cite journal| author=Baskurt M, Okcun B, Abaci O, Dogan GM, Kilickesmez K, Ozkan AA et al.| title=N-acetylcysteine versus N-acetylcysteine + theophylline for the prevention of contrast nephropathy. | journal=Eur J Clin Invest | year= 2009 | volume= 39 | issue= 9 | pages= 793-9 | pmid=19500141 | doi=10.1111/j.1365-2362.2009.02173.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19500141 }} </ref> Still, the use of theophylline is not advocated given the limited data and the skewed risk to benefit ratio. Theophylline has many side effects including cardiac and CNS toxicity, and a very narrow therapeutic index entailing cautious use. '''The 2012 KDIGO guidelines recommend against the use of theophylline for CIN prophylaxis.''' | |||
====Statins==== | |||
[[Clinical practice guideline]]s by KDIGO from 2012 did not recommend statins.<ref name="pmid25018920">{{cite journal|author=Kidney Disease Improving Global Outcomes Work Group| title=2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury| journal=Kidey Int Supp |year= 2012 | volume= 2 | pages= 69-88 | doi=10.1038/kisup.2011.34 | pmc=|url=http://www.nature.com/kisup/journal/v2/n1/full/kisup201134a.html }} </ref> | |||
More recently: | |||
* A [[meta-analysis]] suggests "High-dose [[statin]]s plus hydration with or without [[N-acetylcysteine|NAC]] might be the preferred treatment strategy to prevent contrast-induced". <ref name="pmid27707552">{{cite journal| author=Su X, Xie X, Liu L, Lv J, Song F, Perkovic V et al.| title=Comparative Effectiveness of 12 Treatment Strategies for Preventing Contrast-Induced Acute Kidney Injury: A Systematic Review and Bayesian Network Meta-analysis. | journal=Am J Kidney Dis | year= 2016 | volume= | issue= | pages= | pmid=27707552 | doi=10.1053/j.ajkd.2016.07.033 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27707552 }} </ref> Consistent with the meta-analysis<ref name="pmid27707552"/> | |||
====Fenoldopam==== | |||
Fenoldopam is a selective dopamine A1 receptor agonist used as an anti-hypertensive with the added effect of increased renal medullary blood flow. Although small retrospective reviews showed benefit from using fenoldopam with isotonic saline, two randomized control trials showed no added benefit from using fenoldopam with saline compared to saline alone.<ref name="pmid12410497">{{cite journal| author=Allaqaband S, Tumuluri R, Malik AM, Gupta A, Volkert P, Shalev Y et al.| title=Prospective randomized study of N-acetylcysteine, fenoldopam, and saline for prevention of radiocontrast-induced nephropathy. | journal=Catheter Cardiovasc Interv | year= 2002 | volume= 57 | issue= 3 | pages= 279-83 | pmid=12410497 | doi=10.1002/ccd.10323 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12410497 }} </ref><ref name="pmid14600187">{{cite journal| author=Stone GW, McCullough PA, Tumlin JA, Lepor NE, Madyoon H, Murray P et al.| title=Fenoldopam mesylate for the prevention of contrast-induced nephropathy: a randomized controlled trial. | journal=JAMA | year= 2003 | volume= 290 | issue= 17 | pages= 2284-91 | pmid=14600187 | doi=10.1001/jama.290.17.2284 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14600187 }} </ref> '''The 2012 KDIGO AKI guidelines recommend against using fenoldopam as a CIN prophylactic agent.'''<ref name="doi10.1038/kisup.2011.34">{{cite journal|author=Kidney Disease Improving Global Outcomes Work Group| title=2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury| journal=Kidey Int Supp |year= 2012 | volume= 2 | pages= 69-88 | doi=10.1038/kisup.2011.34 | pmc=|url=http://www.nature.com/kisup/journal/v2/n1/full/kisup201134a.html }} </ref> | |||
====Other interventions==== | |||
Other pharmacological agents, such as [[furosemide]], [[mannitol]], [[dopamine]], and [[atrial natriuretic peptide]] have been tried, but have either not had beneficial effects, or had detrimental effects.<ref name="pmid7969280"/><ref name="pmid10073832">{{cite journal | author=Abizaid AS, Clark CE, Mintz GS, Dosa S, Popma JJ, Pichard AD, Satler LF, Harvey M, Kent KM, Leon MB | title=Effects of dopamine and aminophylline on contrast-induced acute renal failure after coronary angioplasty in patients with preexisting renal insufficiency | journal=Am J Cardiol | year=1999 | pages=260-3, A5 | volume=83 | issue=2 | id=PMID 10073832}}</ref> | |||
==2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury (DO NOT EDIT)<ref name="pmiddoi:10.1038/kisup.2011.34">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 |pmid=doi:10.1038/kisup.2011.34 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10}}</ref>== | ==2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury (DO NOT EDIT)<ref name="pmiddoi:10.1038/kisup.2011.34">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 |pmid=doi:10.1038/kisup.2011.34 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10}}</ref>== | ||
Latest revision as of 08:53, 22 February 2018
|
Contrast Induced Nephropathy Microchapters |
|
Differentiating Contrast induced nephropathy from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Contrast induced nephropathy primary prevention On the Web |
|
American Roentgen Ray Society Images of Contrast induced nephropathy primary prevention |
|
Directions to Hospitals Treating Contrast induced nephropathy |
|
Risk calculators and risk factors for Contrast induced nephropathy primary prevention |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohamed Moubarak, M.D. [2]
Overview
Many strategies have aimed at preventing CIN. Non-therapeutic measures include smaller doses of contrast and use of low-osmolar or iso-osmolar agents.
Prevention
Non-Pharmacologic Approaches
Dose of contrast media
The 2012 clinical practice guidelines by KDIGO recommended using the smallest possible dose in every procedure requiring IV contrast especially in patients at high risk for developing CIN.[1] Nyman et al suggested an alternative approach, using the ratio of dose of iodine (in grams) to estimated glomerular filtration rate (eGFR). The team found the ratio to be predictive of the risk of CIN. A ratio I(g)/eGFR < 1 was shown to be relatively safe even in patients with many possible risk factors. The estimated risk decreased eightfold when the ratio dropped below 1.[2]
Route of Administration
Most studies illustrating the pathophysiology, treatment and prophylaxis of CIN focus on intra-arterial (IA) injection of contrast media considering it has been associated with the highest cases of CIN. A number of trials have also shown that intra-venous (IV) contrast has a significantly lower risk of CIN than IA contrast.[3][4] In fact, a review by Rao and Newhouse showed that in studies with proper controls, the risk of CIN after IV contrast administration did not differ between the study groups and the control groups.[5] This further emphasizes the importance of the route of contrast administration, and points to the fact that IV contrast has not been explicitly shown to be nephrotoxic.
Osmolarity of Contrast Agent
The clinical practice guidelines from 2012 by KDIGO advocate the use of either iso-osmolar or low-osmolar iodinated contrast media, rather than high-osmolar media particularly in patients at increased risk of CIN.[1]
More recently:
- A more recent randomized controlled trial found no difference in frequency of nephropathy between iso and low osmolar contrast agents.[6]
 |
 |
Pharmacologic Approaches
Volume Expansion
The mechanisms by which volume expansion decrease the risk of CIN may include dilution of the contrast media, increase in renal prostaglandins, counteraction of altered renal hemodynamics, and inhibition of the renin-angiotensin system.
Clinical practice guidelines from 2012 by KDIGO recommend fluid administration should be initiated 1-2 h intravenously before and maintained for 3–6 hours after contrast exposure.[1]
More recently:
- Sodium bicarbonate was found beneficial by a meta-analysis of patients with pre-existing renal insufficiency.[7] The 2012 KDIGO guidelines did not recommend against the use of bicarbonate stating possible benefit but inconsistent data.
- Among patients undergoing cardiac catheterization, dosing the amount of fluid based on the left ventricular end-diastolic pressure is beneficial.[8]
N-acetylcysteine
N-acetylcyteine (NAC) is a mycolytic agent and an antioxidant used in the treatment of acetaminophen overdose.
Clinical practice guidelines by KDIGO from 2012 recommend NAC along with isotonic crystalloids.[1]
More recently:
- A meta-analysis suggests "High-dose statins plus hydration with or without NAC might be the preferred treatment strategy to prevent contrast-induced". [9] Consistent with the meta-analysis[9]
- Morerandomized controlled trials found similar outcomes between normal saline (NS) alone, NS with N-acetylcysteine, NS with sodium bicarbonate.[10][11]
Two commonly used regimens are N-acetylcysteine (NAC) 600 mg orally twice daily, one day before the procedure and on the day of the procedure,[12] or a higher dose of 1200 mg orally twice daily administered in the similarly.[13].
Prophylactic Hemodialysis
Considering studies have shown association with estimated GFR and risk of CIN, and given the fact that contrast media can be effectively removed with as little as one session of hemodialysis, many studies have aimed at evaluating the benefit of pre-emptive hemodialysis in patients with underlying renal disease. Studies until recently have had very variable results with some showing lower risk of CIN,[14][15] some showing no added benefit over saline infusion or NAC,[16][17] and some even showing a worse outcome following hemodialysis.[18] Given the very conflicting evidence, the eleveated costs, and the difficult logistics, no recommendations can be made about the use of prophylactic hemodialysis for CIN prevention. The 2012 KDIGO guidelines recommend against the use of prophylactic hemodialysis stating that use can only be advocated if future studies convincingly show added benefit.[19]
Theophylline
Interest in theophylline for CIN prophylaxis stems from the association of adenosine with the pathophysiology of CIN in certain studies.[20] Theophylline is a methylxanthine previously used for the treatment of asthma that also acts as an adenosine antagonist. Data about the use of theophylline is conflicting and several meta-analysis have shown little to not benefit from the use of theophylline prophylaxis.[21][22] However, more recent studies have shown some significant decrease in the risk of CIN when theophylline was compared to other prophylactic measures notably N-acetylcysteine and bicarbonate.[23][24] Still, the use of theophylline is not advocated given the limited data and the skewed risk to benefit ratio. Theophylline has many side effects including cardiac and CNS toxicity, and a very narrow therapeutic index entailing cautious use. The 2012 KDIGO guidelines recommend against the use of theophylline for CIN prophylaxis.
Statins
Clinical practice guidelines by KDIGO from 2012 did not recommend statins.[1]
More recently:
- A meta-analysis suggests "High-dose statins plus hydration with or without NAC might be the preferred treatment strategy to prevent contrast-induced". [9] Consistent with the meta-analysis[9]
Fenoldopam
Fenoldopam is a selective dopamine A1 receptor agonist used as an anti-hypertensive with the added effect of increased renal medullary blood flow. Although small retrospective reviews showed benefit from using fenoldopam with isotonic saline, two randomized control trials showed no added benefit from using fenoldopam with saline compared to saline alone.[25][26] The 2012 KDIGO AKI guidelines recommend against using fenoldopam as a CIN prophylactic agent.[19]
Other interventions
Other pharmacological agents, such as furosemide, mannitol, dopamine, and atrial natriuretic peptide have been tried, but have either not had beneficial effects, or had detrimental effects.[27][28]
2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury (DO NOT EDIT)[29]
Nonpharmacological prevention strategies of CI-AKI
| Level 1 |
| "1. We recommend using either iso-osmolar or low-osmolar iodinated contrast media, rather than high-osmolar iodinated contrast media in patients at increased risk of CI-AKI. (Level of Evidence: 1B)" |
| Not Graded |
| "1. Use the lowest possible dose of contrast medium in patients at risk for CI-AKI. (Level of Evidence: Not Graded)" |
| Level 2 |
| "1. We suggest not using prophylactic intermittent hemodialysis (IHD) or hemofiltration (HF) for contrast-media removal in patients at increased risk for CI-AKI. (Level of Evidence: 2C)" |
Pharmacological prevention strategies of CI-AKI
| Level 1 |
| "1. We recommend i.v. volume expansion with either isotonic sodium chloride or sodium bicarbonate solutions, rather than no i.v. volume expansion, in patients at increased risk for CI-AKI. (Level of Evidence: 1A)" |
| "2. We recommend not using oral fluids alone in patients at increased risk of CI-AKI. (Level of Evidence: 1C)" |
| "3. We recommend not using fenoldopam to prevent CI-AKI. (Level of Evidence: 1B)" |
| Level 2 |
| "1. We suggest using oral NAC, together with i.v. iso-tonic crystalloids, in patients at increased risk of CI-AKI. (Level of Evidence: 2D)" |
| "2. We suggest not using theophylline to prevent CI-AKI. (Level of Evidence: 2C)" |
2011 ACCF/AHA/SCAI Guideline Recommendations: Pre-procedural Considerations (DO NOT EDIT)[30]
Contrast-Induced Acute Kidney Injury
| Class I |
| "1. Patients should be assessed for risk of contrast-induced acute kidney injury before PCI.[31][32] (Level of Evidence: C)" |
| "2. Patients undergoing cardiac catheterization with contrast media should receive adequate preparatory hydration.[33][34][27][35] (Level of Evidence: B)" |
| "3. In patients with chronic kidney disease (CKD) (creatinine clearance <60 mL/min), the volume of contrast media should be minimized.[36][37][38] (Level of Evidence: B)" |
| Class III: Harm |
| "'1. Administration of N-acetyl-L-cysteine is not useful for the prevention of contrast-induced acute kidney injury.[39][40][41][42][43] (Level of Evidence: B)" |
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Kidney Disease Improving Global Outcomes Work Group (2012). "2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury". Kidey Int Supp. 2: 69–88. doi:10.1038/kisup.2011.34.
- ↑ Nyman U, Björk J, Aspelin P, Marenzi G (2008). "Contrast medium dose-to-GFR ratio: a measure of systemic exposure to predict contrast-induced nephropathy after percutaneous coronary intervention". Acta Radiol. 49 (6): 658–67. doi:10.1080/02841850802050762. PMID 18568558.
- ↑ Cramer BC, Parfrey PS, Hutchinson TA, Baran D, Melanson DM, Ethier RE; et al. (1985). "Renal function following infusion of radiologic contrast material. A prospective controlled study". Arch Intern Med. 145 (1): 87–9. PMID 3882071.
- ↑ Heller CA, Knapp J, Halliday J, O'Connell D, Heller RF (1991). "Failure to demonstrate contrast nephrotoxicity". Med J Aust. 155 (5): 329–32. PMID 1895978.
- ↑ Rao QA, Newhouse JH (2006). "Risk of nephropathy after intravenous administration of contrast material: a critical literature analysis". Radiology. 239 (2): 392–7. doi:10.1148/radiol.2392050413. PMID 16543592.
- ↑ Eng J, Wilson RF, Subramaniam RM, Zhang A, Suarez-Cuervo C, Turban S; et al. (2016). "Comparative Effect of Contrast Media Type on the Incidence of Contrast-Induced Nephropathy: A Systematic Review and Meta-analysis". Ann Intern Med. 164 (6): 417–24. doi:10.7326/M15-1402. PMID 26830055.
- ↑ Zhang B, Liang L, Chen W, Liang C, Zhang S (2015). "The efficacy of sodium bicarbonate in preventing contrast-induced nephropathy in patients with pre-existing renal insufficiency: a meta-analysis". BMJ Open. 5 (3): e006989. doi:10.1136/bmjopen-2014-006989. PMC 4368906. PMID 25783425.
- ↑ Brar SS, Aharonian V, Mansukhani P, Moore N, Shen AY, Jorgensen M; et al. (2014). "Haemodynamic-guided fluid administration for the prevention of contrast-induced acute kidney injury: the POSEIDON randomised controlled trial". Lancet. 383 (9931): 1814–23. doi:10.1016/S0140-6736(14)60689-9. PMID 24856027.
- ↑ 9.0 9.1 9.2 9.3 Su X, Xie X, Liu L, Lv J, Song F, Perkovic V; et al. (2016). "Comparative Effectiveness of 12 Treatment Strategies for Preventing Contrast-Induced Acute Kidney Injury: A Systematic Review and Bayesian Network Meta-analysis". Am J Kidney Dis. doi:10.1053/j.ajkd.2016.07.033. PMID 27707552.
- ↑ Weisbord SD, Gallagher M, Jneid H, Garcia S, Cass A, Thwin SS; et al. (2018). "Outcomes after Angiography with Sodium Bicarbonate and Acetylcysteine". N Engl J Med. 378 (7): 603–614. doi:10.1056/NEJMoa1710933. PMID 29130810.
- ↑ Turedi S, Erdem E, Karaca Y, Tatli O, Sahin A, Turkmen S; et al. (2016). "The High Risk of Contrast-induced Nephropathy in Patients with Suspected Pulmonary Embolism Despite Three Different Prophylaxis: A Randomized Controlled Trial". Acad Emerg Med. 23 (10): 1136–1145. doi:10.1111/acem.13051. PMID 27411777.
- ↑ Kay J, Chow W, Chan T, Lo S, Kwok O, Yip A, Fan K, Lee C, Lam W (2003). "Acetylcysteine for prevention of acute deterioration of renal function following elective coronary angiography and intervention: a randomized controlled trial". JAMA. 289 (5): 553–8. PMID 12578487.
- ↑ Marenzi G, Assanelli E, Marana I, Lauri G, Campodonico J, Grazi M, De Metrio M, Galli S, Fabbiocchi F, Montorsi P, Veglia F, Bartorelli A (2006). "N-acetylcysteine and contrast-induced nephropathy in primary angioplasty". N Engl J Med. 354 (26): 2773–82. PMID 16807414.
- ↑ Lee PT, Chou KJ, Liu CP, Mar GY, Chen CL, Hsu CY; et al. (2007). "Renal protection for coronary angiography in advanced renal failure patients by prophylactic hemodialysis. A randomized controlled trial". J Am Coll Cardiol. 50 (11): 1015–20. doi:10.1016/j.jacc.2007.05.033. PMID 17825709 Check
|pmid=value (help). Review in: ACP J Club. 2008 Mar-Apr;148(2):43 - ↑ Marenzi G, Marana I, Lauri G, Assanelli E, Grazi M, Campodonico J; et al. (2003). "The prevention of radiocontrast-agent-induced nephropathy by hemofiltration". N Engl J Med. 349 (14): 1333–40. doi:10.1056/NEJMoa023204. PMID 14523141.
- ↑ Kawashima S, Takano H, Iino Y, Takayama M, Takano T (2006). "Prophylactic hemodialysis does not prevent contrast-induced nephropathy after cardiac catheterization in patients with chronic renal insufficiency". Circ J. 70 (5): 553–8. PMID 16636489 Check
|pmid=value (help). - ↑ Reinecke H, Fobker M, Wellmann J, Becke B, Fleiter J, Heitmeyer C; et al. (2007). "A randomized controlled trial comparing hydration therapy to additional hemodialysis or N-acetylcysteine for the prevention of contrast medium-induced nephropathy: the Dialysis-versus-Diuresis (DVD) Trial". Clin Res Cardiol. 96 (3): 130–9. doi:10.1007/s00392-007-0473-4. PMID 17180572.
- ↑ Vogt B, Ferrari P, Schönholzer C, Marti HP, Mohaupt M, Wiederkehr M; et al. (2001). "Prophylactic hemodialysis after radiocontrast media in patients with renal insufficiency is potentially harmful". Am J Med. 111 (9): 692–8. PMID 11747848.
- ↑ 19.0 19.1 Kidney Disease Improving Global Outcomes Work Group (2012). "2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury". Kidey Int Supp. 2: 69–88. doi:10.1038/kisup.2011.34.
- ↑ Arakawa K, Suzuki H, Naitoh M, Matsumoto A, Hayashi K, Matsuda H; et al. (1996). "Role of adenosine in the renal responses to contrast medium". Kidney Int. 49 (5): 1199–206. PMID 8731082.
- ↑ Bagshaw SM, Ghali WA (2005). "Theophylline for prevention of contrast-induced nephropathy: a systematic review and meta-analysis". Arch Intern Med. 165 (10): 1087–93. doi:10.1001/archinte.165.10.1087. PMID 15911721.
- ↑ Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC (2008). "Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy". Ann Intern Med. 148 (4): 284–94. PMID 18283206 Check
|pmid=value (help). - ↑ Huber W, Eckel F, Hennig M, Rosenbrock H, Wacker A, Saur D; et al. (2006). "Prophylaxis of contrast material-induced nephropathy in patients in intensive care: acetylcysteine, theophylline, or both? A randomized study". Radiology. 239 (3): 793–804. doi:10.1148/radiol.2393041456. PMID 16714461 Check
|pmid=value (help). - ↑ Baskurt M, Okcun B, Abaci O, Dogan GM, Kilickesmez K, Ozkan AA; et al. (2009). "N-acetylcysteine versus N-acetylcysteine + theophylline for the prevention of contrast nephropathy". Eur J Clin Invest. 39 (9): 793–9. doi:10.1111/j.1365-2362.2009.02173.x. PMID 19500141 Check
|pmid=value (help). - ↑ Allaqaband S, Tumuluri R, Malik AM, Gupta A, Volkert P, Shalev Y; et al. (2002). "Prospective randomized study of N-acetylcysteine, fenoldopam, and saline for prevention of radiocontrast-induced nephropathy". Catheter Cardiovasc Interv. 57 (3): 279–83. doi:10.1002/ccd.10323. PMID 12410497 Check
|pmid=value (help). - ↑ Stone GW, McCullough PA, Tumlin JA, Lepor NE, Madyoon H, Murray P; et al. (2003). "Fenoldopam mesylate for the prevention of contrast-induced nephropathy: a randomized controlled trial". JAMA. 290 (17): 2284–91. doi:10.1001/jama.290.17.2284. PMID 14600187 Check
|pmid=value (help). - ↑ 27.0 27.1 Solomon R, Werner C, Mann D, D'Elia J, Silva P (1994). "Effects of saline, mannitol, and furosemide to prevent acute decreases in renal function induced by radiocontrast agents". The New England Journal of Medicine. 331 (21): 1416–20. doi:10.1056/NEJM199411243312104. PMID 7969280. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ Abizaid AS, Clark CE, Mintz GS, Dosa S, Popma JJ, Pichard AD, Satler LF, Harvey M, Kent KM, Leon MB (1999). "Effects of dopamine and aminophylline on contrast-induced acute renal failure after coronary angioplasty in patients with preexisting renal insufficiency". Am J Cardiol. 83 (2): 260–3, A5. PMID 10073832.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID doi:10.1038/kisup.2011.34 Check
|pmid=value (help). - ↑ Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B; et al. (2011). "2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions". Circulation. 124 (23): e574–651. doi:10.1161/CIR.0b013e31823ba622. PMID 22064601.
- ↑ Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, Leon MB, Dangas G (2004). "A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation". Journal of the American College of Cardiology. 44 (7): 1393–9. doi:10.1016/j.jacc.2004.06.068. PMID 15464318. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ Moscucci M, Rogers EK, Montoye C, Smith DE, Share D, O'Donnell M, Maxwell-Eward A, Meengs WL, De Franco AC, Patel K, McNamara R, McGinnity JG, Jani SM, Khanal S, Eagle KA (2006). "Association of a continuous quality improvement initiative with practice and outcome variations of contemporary percutaneous coronary interventions". Circulation. 113 (6): 814–22. doi:10.1161/CIRCULATIONAHA.105.541995. PMID 16461821. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ Bader BD, Berger ED, Heede MB, Silberbaur I, Duda S, Risler T, Erley CM (2004). "What is the best hydration regimen to prevent contrast media-induced nephrotoxicity?". Clinical Nephrology. 62 (1): 1–7. PMID 15267006. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Mueller C, Buerkle G, Buettner HJ, Petersen J, Perruchoud AP, Eriksson U, Marsch S, Roskamm H (2002). "Prevention of contrast media-associated nephropathy: randomized comparison of 2 hydration regimens in 1620 patients undergoing coronary angioplasty". Archives of Internal Medicine. 162 (3): 329–36. PMID 11822926. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ Trivedi HS, Moore H, Nasr S, Aggarwal K, Agrawal A, Goel P, Hewett J (2003). "A randomized prospective trial to assess the role of saline hydration on the development of contrast nephrotoxicity". Nephron. Clinical Practice. 93 (1): C29–34. PMID 12411756. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Marenzi G, Assanelli E, Campodonico J, Lauri G, Marana I, De Metrio M, Moltrasio M, Grazi M, Rubino M, Veglia F, Fabbiocchi F, Bartorelli AL (2009). "Contrast volume during primary percutaneous coronary intervention and subsequent contrast-induced nephropathy and mortality". Annals of Internal Medicine. 150 (3): 170–7. PMID 19189906. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ McCullough PA, Wolyn R, Rocher LL, Levin RN, O'Neill WW (1997). "Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality". The American Journal of Medicine. 103 (5): 368–75. PMID 9375704. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ Russo D, Minutolo R, Cianciaruso B, Memoli B, Conte G, De Nicola L (1995). "Early effects of contrast media on renal hemodynamics and tubular function in chronic renal failure". Journal of the American Society of Nephrology : JASN. 6 (5): 1451–8. PMID 8589322. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ Gonzales DA, Norsworthy KJ, Kern SJ, Banks S, Sieving PC, Star RA, Natanson C, Danner RL (2007). "A meta-analysis of N-acetylcysteine in contrast-induced nephrotoxicity: unsupervised clustering to resolve heterogeneity". BMC Medicine. 5: 32. doi:10.1186/1741-7015-5-32. PMC 2200657. PMID 18001477. Retrieved 2011-12-06.
- ↑ Ozcan EE, Guneri S, Akdeniz B, Akyildiz IZ, Senaslan O, Baris N, Aslan O, Badak O (2007). "Sodium bicarbonate, N-acetylcysteine, and saline for prevention of radiocontrast-induced nephropathy. A comparison of 3 regimens for protecting contrast-induced nephropathy in patients undergoing coronary procedures. A single-center prospective controlled trial". American Heart Journal. 154 (3): 539–44. doi:10.1016/j.ahj.2007.05.012. PMID 17719303. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ Thiele H, Hildebrand L, Schirdewahn C, Eitel I, Adams V, Fuernau G, Erbs S, Linke A, Diederich KW, Nowak M, Desch S, Gutberlet M, Schuler G (2010). "Impact of high-dose N-acetylcysteine versus placebo on contrast-induced nephropathy and myocardial reperfusion injury in unselected patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. The LIPSIA-N-ACC (Prospective, Single-Blind, Placebo-Controlled, Randomized Leipzig Immediate PercutaneouS Coronary Intervention Acute Myocardial Infarction N-ACC) Trial". Journal of the American College of Cardiology. 55 (20): 2201–9. doi:10.1016/j.jacc.2009.08.091. PMID 20466200. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ Webb JG, Pate GE, Humphries KH, Buller CE, Shalansky S, Al Shamari A, Sutander A, Williams T, Fox RS, Levin A (2004). "A randomized controlled trial of intravenous N-acetylcysteine for the prevention of contrast-induced nephropathy after cardiac catheterization: lack of effect". American Heart Journal. 148 (3): 422–9. doi:10.1016/j.ahj.2004.03.041. PMID 15389228. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help) - ↑ "Acetylcysteine for prevention of renal outcomes in patients undergoing coronary and peripheral vascular angiography: main results from the randomized Acetylcysteine for Contrast-induced nephropathy Trial (ACT)". Circulation. 124 (11): 1250–9. 2011. doi:10.1161/CIRCULATIONAHA.111.038943. PMID 21859972. Retrieved 2011-12-06. Unknown parameter
|month=ignored (help)
- Pages with reference errors
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- CS1 maint: PMC format
- CS1 errors: PMID
- Pages with citations using unsupported parameters
- Pages using citations with accessdate and no URL
- Disease
- Nephrology
- Radiology
- Cardiology
- Up-To-Date
- Up-To-Date cardiology