Colposcopy
For patient information, click here
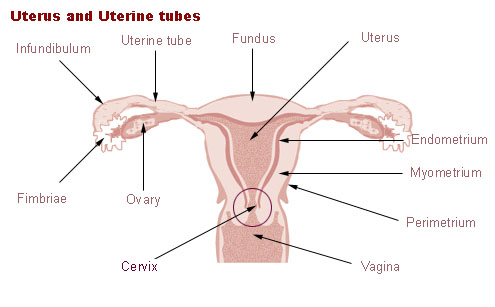
The transformation zone, at the opening of the cervix into the vagina, is the area where most abnormal cell changes occur.
|
WikiDoc Resources for Colposcopy |
|
Articles |
|---|
|
Most recent articles on Colposcopy |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Colposcopy at Clinical Trials.gov Clinical Trials on Colposcopy at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Colposcopy
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Colposcopy Discussion groups on Colposcopy Patient Handouts on Colposcopy Directions to Hospitals Treating Colposcopy Risk calculators and risk factors for Colposcopy
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Colposcopy |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Colposcopy or colcoscopy is a medical diagnostic procedure to examine an illuminated, magnified view of the cervix and the tissues of the vagina and vulva. Many premalignant lesions and malignant lesions in these areas have discernible characteristics which can be detected thorough the examination. It is done using a colposcope, which provides an enlarged view of the areas, allowing the colposcopist to visually distinguish normal from abnormal appearing tissue and take directed biopsies for further pathological examination. The main goal of colposcopy is to prevent cervical cancer by detecting precancerous lesions early and treating them. The procedure was developed in 1925 by the German physician Hans Hinselmann.
Indications for colposcopy
Most women undergo a colposcopic examination to further investigate a cytological abnormality on their pap smears. Other indications for a woman to have a colposcopy include:
- assessment of diethylstilbestrol (DES) exposure in utero,
- immunosuppression such as HIV infection, or
- an abnormal appearance of the cervix as noted by a physician.
Many physicians base their current evaluation and treatment decisions on the report "Guidelines for the Management of Cytological Abnormalities and Cervical Cancer Precursors", created by the American Society for Colposcopy and Cervical Pathology, during a September 2001 conference. [1]
The procedure

During the initial evaluation, a medical history is obtained, including gravidity (number of prior pregnancies), parity (number of prior deliveries), last menstrual period, contraception use, prior abnormal pap smear results, allergies, significant past medical history, other medications, prior cervical procedures, and smoking history. In some cases, a pregnancy test may be performed before the procedure. The procedure is fully described to the patient, questions are asked and answered, and she then signs a consent form.
A colposcope is used to identify visible clues suggestive of abnormal tissue. It functions as a lighted binocular microscope to magnify the view of the cervix, vagina, and vulvar surface. Low power (2× to 6×) may be used to obtain a general impression of the surface architecture. Medium (8× to 15×) and high (15× to 25×) powers are utilized to evaluate the vagina and cervix. The higher powers are often necessary to identify certain vascular patterns that may indicate the presence of more advanced precancerous or cancerous lesions. Various light filters are available to highlight different aspects of the surface of the cervix. Acetic acid solution and iodine solution (Lugol's or Schiller's) are applied to the surface to improve visualization of abnormal areas.
Colposcopy is performed with the woman on her back, legs in stirrups, and buttocks close to the lower edge of the table (a position known as the dorsal lithotomy position). A speculum is placed in the vagina after the vulva is examined for any suspicious lesions.
Three percent acetic acid is applied to the cervix using cotton swabs. The transformation zone is a critical area on the cervix where many precancerous and cancerous lesions most often arise. The ability to see the transformation zone and the entire extent of any lesion visualized determines whether an adequate colposcopic examination is attainable.
Areas of the cervix which turn white after the application of acetic acid or have an abnormal vascular pattern are often considered for biopsy. If no lesions are visible, an iodine solution may be applied to the cervix to help highlight areas of abnormality.
After a complete examination, the colposcopist determines the areas with the highest degree of visible abnormality and obtains biopsies from these areas using a long biopsy instrument. Some doctors consider anesthesia unnecessary, however, many colposcopists now recommend and use a topical anesthetic such as lidocaine or a cervical block to diminish patient discomfort, particularly if many biopsy samples are taken.
Following any biopsies, an endocervical curettage (ECC) is often done. The ECC utilizes a long straight curette to scrape the inside of the cervical canal. The ECC should never be done on a pregnant woman. Monsel's solution is applied with large cotton swabs to the surface of the cervix to control bleeding. This solution looks like mustard and becomes black in color when exposed to blood. After the procedure this material will be expelled naturally: women can expect to have a thin coffee-ground like discharge for up to several days after the procedure.
Complications
Significant complications from a colposcopy are not common, but may include bleeding, infection at the biopsy site or endometrium, and failure to identify the lesion. Monsel's solution and silver nitrate interfere with interpretation of biopsy specimen, so these substances should not be applied until all biopsies have been taken. Most patients experience some degree of pain during the curettage, and almost all experience pain during the biopsy.
Follow up
Adequate follow-up is critical to the success of this procedure. Human Papilloma Virus (HPV) is a common infection and the underlying cause for most cervical dysplasia. Women should be counseled on the benefits of safe sex for reducing their risks of contracting and spreading the HPV virus.[2]
A new vaccination against HPV (Gardasil) was approved June 8, 2006 by the US Food and Drug Administration after being tested for five years on 20,541 girls from age 16 to 26. The vaccine is indicated for prevention of cervical cancer, precancerous and dysplastic lesions and genital warts caused by HPV types 6, 11, 16 and 18. Adequate widespread vaccination may reduce the need for colposcopic examinations in the future.
Smoking predisposes women to developing cervical abnormalities. A smoking cessation program should be part of the treatment plan for women who smoke.
Without proper treatment, minor abnormalities may develop into cancerous lesions. Various treatments exist for significant lesions, most commonly cryotherapy, loop electrical excision procedure (LEEP), and laser ablation.
Future technologies
Colposcopy is the "gold standard" tool in the United States for diagnosing cervical abnormalities after an abnormal pap smear. The procedure requires many resources and can be expensive to perform, making it a less-than-ideal screening tool.
Newer visualization techniques on the horizon utilize broad-band light (e.g., direct visualization, speculoscopy, cervicography, and colposcopy) and electronic detection methods (e.g., Polarprobe and in-vivo Spectroscopy). These techniques are less expensive and can be performed with significantly less training. At this point, these newer techniques have not been validated by large-scale trials and are not in general use.