Coccidioidomycosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 13: | Line 13: | ||
{{Search infobox}} | {{Search infobox}} | ||
{{CMG}} | {{CMG}} | ||
==Overview== | ==Overview== | ||
| Line 49: | Line 47: | ||
==External links== | ==External links== | ||
* [http://www.cdc.gov/ncidod/dbmd/diseaseinfo/coccidioidomycosis_t.htm U.S. Centers for Disease Control and Prevention page on Coccidioidomycosis] | * [http://www.cdc.gov/ncidod/dbmd/diseaseinfo/coccidioidomycosis_t.htm U.S. Centers for Disease Control and Prevention page on Coccidioidomycosis] | ||
* [http://www.nlm.nih.gov/medlineplus/ency/article/001322.htm Medline Plus Entry for Coccidioidomycosis] | * [http://www.nlm.nih.gov/medlineplus/ency/article/001322.htm Medline Plus Entry for Coccidioidomycosis] | ||
{{Mycoses}} | {{Mycoses}} | ||
| Line 62: | Line 55: | ||
[[Category:Fungal diseases]] | [[Category:Fungal diseases]] | ||
[[Category:Biological weapons]] | [[Category:Biological weapons]] | ||
[[Category:Infectious | [[Category:Infectious disease]] | ||
[[Category:Mature chapter]] | |||
[[de:Kokzidioidomykose]] | [[de:Kokzidioidomykose]] | ||
[[es:Coccidioidomicosis]] | [[es:Coccidioidomicosis]] | ||
| Line 68: | Line 63: | ||
[[pt:Coccidioidomicose]] | [[pt:Coccidioidomicose]] | ||
{{SIB}} | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Revision as of 17:50, 1 August 2011
Template:DiseaseDisorder infobox Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
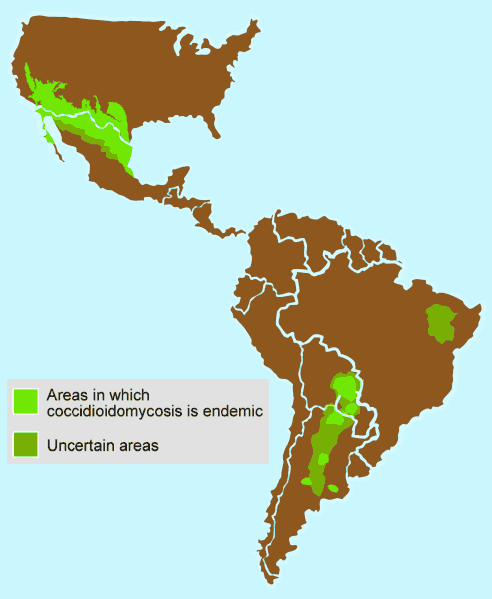
Coccidioidomycosis (also known as Valley fever, San Joaquin Valley Fever, California valley fever, desert fever, and (incorrectly) coccidiomycosis) is a fungal disease caused by Coccidioides immitis or C. posadasii.[1] It is endemic in certain parts of Arizona, California, Nevada, New Mexico, Texas, Utah and northwestern Mexico.[2]
C. immitis resides in the soil in certain parts of the southwestern United States, northern Mexico, and parts of Central and South America [2]. It is dormant during long dry spells, then develops as a mold with long filaments that break off into airborne spores when the rains come. The spores, known as arthroconidia, are swept into the air by disruption of the soil, such as during construction or farming. Infection is caused by inhalation of the particles. The disease is not transmitted from person to person. C. immitis is a dimorphic saprophytic organism that grows as a mycelium in the soil and produces a spherule form in the host organism.
The disease is usually mild, with flu-like symptoms and rashes, and the Mayo Clinic estimates that half the population in some affected areas have suffered from the disease. On occasion, those particularly susceptible, including pregnant women, people with weakened immune systems, and those of Asian, Hispanic and African descent, may develop a serious or even fatal illness from valley fever. Serious complications include severe pneumonia, lung nodules, and disseminated disease, where the fungus spreads throughout the body. The disseminated form of valley fever can devastate the body, causing skin ulcers and abscesses to bone lesions, severe joint pain, heart inflammation, urinary tract problems, meningitis, and death.
It has been known to infect humans, dogs, cattle, livestock, llamas, apes, monkeys, kangaroos, wallabies, tigers, bears, badgers, otters and marine mammals. [3]
Symptomatic infection (40% of cases) usually presents as an influenza-like illness with fever, cough, headaches, rash, and myalgia (muscle pain).[4] Some patients fail to recover and develop chronic pulmonary infection or widespread disseminated infection (affecting meninges, soft tissues, joints, and bone). Severe pulmonary disease may develop in HIV-infected persons.[5] The disease can be fatal.
Occurrence
California state prisons have been particularly affected by Coccidioidomycosis, as far back as 1919. In 2005 and 2006, the Pleasant Valley State Prison near Coalinga and Avenal State Prison near Avenal on the western side of the San Joaquin Valley had the highest incidence rate in 2005, of at least 3,000 per 100,000 [3].
Biological Warfare
C. immitis was investigated by the United States during the 1950s and 1960s as a potential biological weapon. The Cash strain received the military symbol OC, and original hopes were for its use as an incapacitant. As medical epidemiology later made clear, OC would have lethal effects on several segments of the population, so it was later considered a lethal agent. It was never standardized, and beyond a few field trials, it was never weaponized. Most military work on OC was on vaccines by the mid-1960s.
Diagnostic test
The fungal infection can be demonstrated by microscopic detection of diagnostic cells in body fluids, exudates, sputum and biopsy-tissue. With specific nucleotide primers C.immitis DNA can be amplified by PCR. It can also be detected in culture by morphological identification or by using molecular probes that hybridize with C.immitis RNA. An indirect demonstration of fungal infection can be achieved also by serologic analysis detecting fungal antigen or host antibody produced against the fungus.
Pathology
<youtube v=RtpvzCfFwfg/>
Popular culture
The illness is mentioned in episode Lines in the Sand of the TV Show House, as the cause of a young girl's loss of inhibition. The illness does not actually cause loss of inhibition, nor does it cause milky tears. This was not a factual error in the episode: House was tricking the girl, however this was not obvious to many viewers.
It is also the center of an episode of the TV series Bones, The Man In the Fallout Shelter. After being exposed to the fungus, the team was quarantined over Christmas to determine whether or not they had become infected. It was erroneously claimed to be contagious from person to person.
References
- ↑ Walsh TJ, Dixon DM (1996). Spectrum of Mycoses. In: Baron's Medical Microbiology (Baron S et al, eds.) (4th ed. ed.). Univ of Texas Medical Branch. (via NCBI Bookshelf) ISBN 0-9631172-1-1.
- ↑ Hector R, Laniado-Laborin R (2005). "Coccidioidomycosis--a fungal disease of the Americas". PLoS Med. 2 (1): e2. PMID 15696207.
- ↑ Valley Fever Center for Excellence | url = http://www.vfce.arizona.edu/VFID-other.htm
- ↑ Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. pp. pp. 680-83. ISBN 0838585299.
- ↑ Ampel N (2005). "Coccidioidomycosis in persons infected with HIV type 1". Clin Infect Dis. 41 (8): 1174–8. PMID 16163637.
External links
- U.S. Centers for Disease Control and Prevention page on Coccidioidomycosis
- Medline Plus Entry for Coccidioidomycosis